After clinical evaluation, especially clinical prediction rules, appropriately ordered venous duplex has become the standard test for evaluating and excluding deep vein thrombosis (DVT). Ultrasound is useful for lower- and upper-extremity veins. Protocols include grayscale, color Doppler, and spectral Doppler. Recommended lower-extremity protocols include central leg and calf veins. Duplex Doppler is widely used to evaluate patients with chronic venous disease, especially with suspected venous reflux. Mapping to identify adequate veins before surgery is another widely used indication for venous ultrasound. Ultrasound for thrombosis can be characterized as normal, acute DVT, superficial thrombosis, or chronic postthrombotic changes in most patients.
Key points
- •
Lower-extremity peripheral venous ultrasound when performed as a complete compression ultrasound is an accurate single test to rule in and rule out lower-extremity deep vein thrombosis (DVT).
- •
Most patients can be assigned normal, acute DVT, or chronic postthrombotic change. A small number of cases will be inadequate, or the findings will be indeterminate.
- •
Patients with less-comprehensive protocols or technically difficult examinations may require serial or alternative testing.
Compression duplex venous ultrasound (CUS) is the most common test for deep vein thrombosis (DVT). It is sufficiently accurate, superior to venous physiologic tests, better tolerated by the patient, and easier to perform than contrast venography.
Clinical overview
DVT does have significant morbidity, but its most important complication, pulmonary embolism (PE), means that accurate testing may be lifesaving.
The triad of risk factors for DVT has been described by Virchow: stasis, damage to the vein, and a hypercoagulable state. Approximately 69 per 100,000 patients develop DVT or PE, affecting hundreds of thousands of people in the United States each year.
DVT has known signs and symptoms, but these findings are not specific to thrombosis. Therefore, the history and physical examination are not adequate to exclude or diagnose DVT. Hoping to avoid unindicated ultrasound (US) for low-risk patients, many societies have recommended a strategy of clinical evaluation and an assessment of pretest probability before ordering a study. The most common rule set to determine risk is the Wells criteria. This score has 1 point for each major risk factor: active cancer or cancer within 6 months, paralysis, paresis or cast, bedridden for at least 3 days or major surgery within 12 weeks, localized tenderness along the deep venous system, swelling of the entire leg, unilateral calf swelling, unilateral pitting edema, dilation of superficial collateral veins, and prior DVT. Points are subtracted from the score when an alternative diagnosis is at least as likely as DVT. The Wells score is graded as “DVT-likely” or “DVT-unlikely.” DVT-likely patients go on to CUS, whereas the DVT-unlikely patients are recommended to get a D-dimer blood test. A negative D-dimer and a DVT-unlikely score effectively excludes acute DVT. Unfortunately, the D-dimer test is sensitive but not specific, and so a positive D-dimer test does not adequately rule in acute DVT. For this reason, patients with positive D-dimer tests go on to CUS. The D-dimer test is frequently falsely positive in inpatients, so the test is only useful for outpatients and emergency room patients.
Anatomy
The veins of the leg are typically distinguished as deep veins and superficial veins. The deep veins have an accompanying similarly named artery (except for the intramuscular veins of the calf), whereas superficial veins do not have an accompanying artery. Central veins are those located above the knee (popliteal and above), whereas distal veins are in the calf (intermuscular and intramuscular).
The deep veins lie below the muscular fascia and are the major veins draining the lower extremity. The common femoral vein becomes the external iliac vein at the inguinal canal. The common femoral vein is created by the junction of the femoral vein (previously called superficial femoral vein) and the deep femoral vein. The deep femoral vein is usually only evaluated for several centimeters at its termination at the femoral deep femoral confluence. The femoral vein is evaluable throughout its course, although visualization can be challenging at the adductor (Hunter) canal. The femoral vein becomes the popliteal vein as it exits the Hunter canal in the lower thigh. Duplications of the femoral and popliteal veins are not unusual. The popliteal vein is created from the confluence of the intermuscular, typically paired, deep veins in the calf: the anterior tibial, tibioperoneal trunk (formed from the posterior tibial and peroneal veins). There are calf deep veins that lie within the muscles of the calf; most importantly, the soleal and gastrocnemius veins. The intramuscular veins are important because they are frequently the earliest site of acute thrombi, and they may be incorrectly considered superficial veins.
US tends to focus on the 2 major superficial veins: the great saphenous and the small saphenous. The saphenous veins lie superficial to the deep muscular fascia but are bounded more superficially by a saphenous fascia. The great saphenous joins the common femoral vein in the thigh. The small saphenous vein runs along the back of the calf with a variable termination either at the saphenopopliteal junction or more superiorly. Perforating veins connect the superficial and deep system.
In the upper extremity, the deep venous system that is evaluable includes the internal jugular, axillary, subclavian, and brachiocephalic veins centrally, and the brachial vein in the upper arm. The upper-extremity examination also includes the superficial cephalic and basilic veins in the upper arm. Extension to the examination to the forearm veins, such as the radial, ulnar, and superficial veins in the forearm, may be performed if there are symptoms.
Deep vein thrombosis pathophysiology
The development of DVT depends on baseline susceptibility to thrombosis and the presence of risk factors. Hypercoagulable states may be congenital or acquired.
Lower-extremity DVT frequently begins in the calf, and 50% of these remain isolated. Few, if any, of these small calf clots cause symptomatic PE. Of calf DVT, 10% will propagate more centrally.
Acute DVT in the central veins may be either in isolation or in combination with calf DVT. Central DVT can be in one or more veins. Discontinuous, independent sites of acute DVT are the norm rather than one long thrombus. For this reason, the US examination consists of evaluating all accessible portions of the veins because normal veins may be seen next to affected sites.
Acute thrombus consists of combinations of red blood cells, fibrin, and platelets; it is soft and smooth. DVT typically begins behind vein valves and, as it expands, it enlarges the vein. Complete occlusion by the thrombus is usually short-lived because thrombolysis creates a separation of the clot from the vein wall. This accounts for the outline of DVT around the lumen on color Doppler and venography. Weak attachment to the wall and growth toward the heart may create a “free-floating” appearance.
Embolization occurs in acute DVT and may be clinically symptomatic or silent. Following PE, US demonstrates DVT in approximately 30% to 50%. Contrast venography demonstrates more, in part because of nonvisualized veins on US, such as pelvic and some calf veins.
Even as thrombus is forming, the fibrinolytic system is attempting to remove it. Clot lysis consists of retraction from its edges and recanalization through its substance. Most of the evolution from clot to scar takes days to weeks, with some pathologic changes even noted at months to years. By serial US, half of DVT resolves completely without any evidence by US, and half show chronic changes.
Chronic change is no longer thrombus but rather collagen. Society of Radiologists in Ultrasound guidelines have suggested an alternative name for scarring: chronic postthrombotic change. This nomenclature highlights the mechanism and cause. More importantly, it does not use the word thrombus , which can lead to unnecessary anticoagulation if scarring is mistaken for an acute DVT.
Lower-extremity veins
Protocol
Different specialists evaluate different veins in their protocols, leading to inconsistent care. Historically, US had limited resolution and could only evaluate larger central veins. These limited scans are still practiced in some emergency rooms and medicine practices; they consist of portions of the femoral and popliteal veins at 2 (or 3) areas. Limited scans have a significant limitation: a single negative study is inadequate to exclude some DVT. Therefore, although one test is safe temporarily, an acceptably safe strategy requires 2 negative limited scans 1 week apart to adequately exclude DVT.
Complete compression ultrasound (CCUS) from the inguinal ligament to the ankle is recommended by radiological societies and other organizations. , CCUS is a safe strategy: one technically adequate normal study rules in most important sites of DVT and effectively rules out DVT. Serial US is unnecessary unless certain conditions are present ( Tables 1 and 2 ).
| Clinical Characteristic | Recommendation |
|---|---|
| Negative complete duplex ultrasound | |
| Persistent or worsening symptoms | Repeat scan in 5 d to 1 wk, earlier if concern is high |
| High risk | Consider repeat scan if cause for symptoms not otherwise elucidated |
| Technically compromised study | Recommend repeat scan in 5 d to 1 wk if more than minor limitation. D-dimer may be helpful if it is negative |
| Concern for iliocaval DVT | Pelvic venous imaging, especially CT or MR venography, or iliocaval duplex ultrasound |
| Negative extended compression or 2-region ultrasound | |
| Risk of DVT persists or cause of symptoms not elucidated | Repeat scan, preferably complete duplex ultrasound, in 5 d to 1 wk |
| Clinical Characteristic | Recommendation |
|---|---|
| Positive complete duplex ultrasound | |
| Acute calf DVT, not treated | Repeat scan in 1 wk, earlier if symptoms progress. If progression to femoropopliteal DVT, treat. If normal, stop. If persistent calf thrombus, which is not treated, repeat scan at 2 wk. Scanning after 2 wk is generally not warranted |
| Acute DVT, on treatment | Repeat not warranted unless a change in the scan will change patient management Follow-up at the end of treatment to establish new baseline |
| Indeterminate results | D-dimer may be helpful if negative. Recommend repeat scan in 5 d to 1 wk to evaluate for change |
| Concern for recurrent DVT, equivocal findings for scar vs recurrence at site of scar | D-dimer may be helpful if negative. Recommend repeat scan in 1–3 d and 7–10 d |
Scanning the groin to ankle overcomes any potential confusion on who needs follow-up after a more limited study. Adding the calf gives more information and detects calf DVT. The treatment of calf DVT is still in evolution. If calf DVT is treated, no short-term follow-up is needed. If not treated, the patient needs a follow-up in 1 week to exclude propagation. If femoropopliteal DVT appears at follow-up, patients are treated. If the calf DVT is gone, no further evaluation is warranted. However, if the 1-week scan continues to show calf DVT, a second follow-up at 2 weeks is needed. If at 2 weeks there is no change, no further imaging is required unless symptoms worsen.
Complete Compression Ultrasound Protocol
Adequately visualized veins are compressed in their short axis at 1- to 2-cm intervals. With modern equipment, calf veins can be seen in most patients, particularly if the calf is well positioned and the veins are distended by elevating the chest and heart above the leg. The anterior tibial vein is not in the standard protocol, as it is rarely isolated. When compressing the intermuscular calf, attention to the adjacent intramuscular veins can frequently identify soleal or gastrocnemius thrombi. Intramuscular veins may be included when symptomatic areas are scanned. If DVT is seen in the common femoral vein, many laboratories extend the examination to the external iliac vein using curved array transducers to determine if proximal thrombus is present.
The protocol also includes Doppler. Color Doppler is used routinely in the common femoral vein and popliteal vein and may be added to evaluate any areas of suspected thrombus or exclude the presence of a filling defect. Spectral Doppler at both common femoral veins and the ipsilateral popliteal vein is used to evaluate for proximal obstruction or excess pulsatility. Both common femoral veins waveforms are used to evaluate symmetry.
Scanning an area of pain may also detect nonvascular causes, particularly musculoskeletal entities that mimic DVT, for example, Baker cysts, muscular or articular abnormalities that may or not warrant additional imaging.
The sensitivity CCUS for acute DVT in the central veins is high, 96.5% (95% CI: 95.1%–97.6%) with high specificity. Calf DVT has lower sensitivity, 63.5% (95% CI: 59.8%–67%) also with high specificity. Calf DVT is more likely to be detected if there are focal calf symptoms.
Normal and Abnormal Ultrasound Findings
DVT US examination determines if the vein is normal, has acute DVT, has chronic postthrombotic change, or is indeterminate (equivocal) ( Table 3 ).
| Acute Venous Thrombosis | Chronic Postthrombotic Change | |
|---|---|---|
| Vein size | Enlarged | Small |
| Normal if early, too small to enlarge vein | Normal | |
| Vein wall | Thrombus weakly adherent to wall | Scar, incorporated into wall |
| Thickening may be focal, broad based, or circumferential | ||
| Convex outward | Retracted | |
| Intraluminal material with compression the residual lumen will collapse, the intraluminal material will persist | Smooth | Irregular |
| Round | Flat, rough, or lumpy | |
| Soft | Hard | |
|
| |
| Free floating | Thin webs (synechiae) | |
| Flat bands |
Compression Ultrasound
A normal vein will compress completely with apposition of the walls with modest probe pressure. The compression is performed in the short axis so the entire vein can be evaluated during compression. Either paired compression and noncompression views or cine loops may be used as documentation.
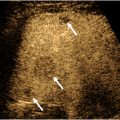
The authors’ laboratory favors the term normal compression when the lumen is completely obliterated, and the walls of the vein are inapparent or thin ( Fig. 1 A, B ). Noncompression is reserved for any situation where the vein does not compress completely ( Fig. 2 A, B ). Noncompressible veins may be due to acute DVT, chronic postthrombotic change, or inadequate compression. “Partial” compressibility is not recommended because it is not descriptive of why the vein does not compress, and this term is not specific enough to describe if there is an acute or chronic process.