KEY FACTS
Terminology
- •
Synonyms: Peritoneal pseudocyst, benign cystic mesothelioma
- •
Not true cyst but peritoneal or ovarian fluid trapped by peritoneal adhesions
Imaging
- •
Unilocular or multilocular pelvic cystic lesion
- •
Boundaries defined by pelvic structures and walls
- •
Unilateral in 65%, bilateral in 35%, midline if large
- •
Normal ovary surrounded or displaced by fluid and septations; entrapped ovary: Spider in web appearance
- •
Fine septations most common
- •
Thick septations with nodules possible
- •
Blood flow can be seen in septations, especially if thick
- •
Transvaginal ultrasound 1st-line to localize ovary and exclude signs of malignancy
- •
MR most useful if peritoneal inclusion cyst (PIC) is large and normal ovaries cannot be found using ultrasound
- •
CT useful for large PIC and for excluding malignant peritoneal disease but less sensitive at locating ovaries
Top Differential Diagnoses
- •
Ovarian cystic neoplasm
- •
Hydrosalpinx
- •
Paraovarian cyst
- •
Endometriosis
- •
Lymphangioma/mesenteric cyst
Pathology
- •
Requires functioning ovary and peritoneal adhesions
Clinical Issues
- •
Almost exclusively premenopausal women
- •
Pelvic pain, palpable mass, abdominal distension, or pressure symptoms or incidentally noted on imaging
- •
Indolent course: May grow, remain stable, or regress
- •
Tend to recur after drainage
Scanning Tips
- •
Look for solid components and normal ovary using transabdominal and transvaginal probes
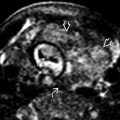
 , and consists of simple fluid with thin septa
, and consists of simple fluid with thin septa  .
.
 . A thin adhesion is present
. A thin adhesion is present  . The left ovarian follicle
. The left ovarian follicle  is smaller; the right ovary has developed a larger cyst
is smaller; the right ovary has developed a larger cyst  .
.
 superior and posterior to the uterus
superior and posterior to the uterus  . Internal echoes were from hemorrhage, confirmed at surgery.
. Internal echoes were from hemorrhage, confirmed at surgery.