Abstract
The persistence of the hypoglossal artery is a rare embryonic vascular variant in which a transient connection between the carotid and vertebrobasilar systems fails to regress. Typically asymptomatic and incidentally discovered on imaging, this condition can alter cerebral blood flow and increase the risk of vascular complications such as aneurysms, strokes, and arteriovenous malformations. We present the case of a 70-year-old female with no prior medical history who was admitted to the emergency department with right-sided hemiparesis. A cerebral CT angiography, performed to evaluate for acute ischemic stroke and potential thrombolysis, revealed a persistent hypoglossal artery arising from the internal carotid artery at the C1-C2 level and connecting to the basilar artery through the hypoglossal canal. This case highlights the importance of recognizing this rare anatomical variant on imaging to prevent misinterpretation and avoid complications during surgical or endovascular interventions at the skull base.
Introduction
The persistent hypoglossal artery is one of the persistent carotid-vertebrobasilar anastomoses that would normally regress during embryonic development. It originates from the posterior aspect of the cervical internal carotid artery, typically between the vertebral levels C1 and C3. It follows the path of the hypoglossal nerve, passing through an enlarged hypoglossal canal, and ultimately joins the basilar artery from below [ ].
The PHA is the second most common type of persistent carotid-basilar anastomosis, following the persistent trigeminal artery. It is a rare anomaly, with an estimated prevalence of 0,02%-0,26% [ ]. However, its recognition on imaging is important due to its potential to cause neurovascular complications [ ].
Case report
We report the case of a 70-year-old female with no known medical history who presented to the emergency department with sudden-onset left-sided hemiparesis evolving over 2 hours. She denied any history of trauma, headache, visual disturbances, seizures, or previous similar episodes. There was no family history of stroke, aneurysm, or other cerebrovascular diseases. The patient was not on any chronic medication and had no history of prior surgeries. She was active and independent, with no apparent cardiovascular risk factors.
On arrival, the patient was hemodynamically stable, with a blood pressure of 120/60 mmHg, heart rate of 88 bpm, respiratory rate of 18 breaths per minute, oxygen saturation of 98% on room air, and body temperature of 36.8°C. Neurological examination revealed motor weakness graded 3/5 in the left upper and lower limbs, while strength was preserved (5/5) on the right side. Superficial and deep sensitivity was intact, reflexes were symmetrical, and there was no facial asymmetry, speech impairment, or cerebellar dysfunction. Cardiovascular, pulmonary, and abdominal examinations were unremarkable.
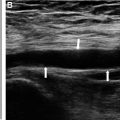
Given the suspicion of an acute ischemic stroke, blood samples were drawn immediately to assess eligibility for thrombolysis, and a cerebral CT angiography was performed without delay. The noncontrast brain CT was unremarkable, ruling out hemorrhage. After contrast injection, imaging revealed a large vessel originating from the internal carotid artery at the C1-C2 level, connecting to the basilar artery through the hypoglossal canal ( Fig. 2 ). 3D reconstructions (MIP and VR) facilitated visualization of the unusual anatomical course of this artery ( Fig. 3 ). The left vertebral artery was found to be hypoplastic ( Fig. 4 ), with no evidence of arterial occlusion. The findings were consistent with an anatomical variant, specifically a carotid-vertebrobasilar anastomosis of the persistent hypoglossal artery type.
While awaiting laboratory results, the patient remained clinically stable, and her symptoms began improving spontaneously. The blood tests returned within normal limits, with hemoglobin at 13.4 g/dL (reference: 12-16 g/dL), white blood cell count at 7,500/mm³ (reference: 4,000-11,000/mm³), platelet count at 235,000/mm³ (reference: 150,000-450,000/mm³), INR at 1.0 (reference: <1.2 for nonanticoagulated patients), and an aPTT of 30 seconds (reference: 25-35 seconds). Blood glucose was 98 mg/dL (reference: 70-140 mg/dL), and kidney function was normal, with a serum creatinine of 0.8 mg/dL (reference: 0.6-1.2 mg/dL). Electrolytes were within normal ranges, and troponin and ECG were unremarkable, ruling out a concurrent cardiac event.
As there was no evidence of large vessel occlusion, no established ischemic infarct, and the patient’s neurological function was rapidly improving, intravenous thrombolysis was not administered. She was admitted to the stroke unit for neurological monitoring and was started on aspirin 100 mg daily, atorvastatin 40 mg daily, and blood pressure management as preventive measures. A carotid Doppler ultrasound was performed, showing no significant atherosclerosis.
The patient recovered fully within 1 hour, and the diagnosis of a transient ischemic attack (TIA) was confirmed. She was discharged on secondary stroke prevention therapy and scheduled for follow-up in neurology and vascular medicine.
This case highlights the importance of recognizing persistent hypoglossal artery as a rare but clinically relevant vascular anomaly. While often asymptomatic, this variant can alter cerebral hemodynamics and predispose patients to vascular complications such as aneurysms and ischemic events. Identifying it on imaging is crucial to prevent misdiagnosis and avoid complications during surgical or endovascular interventions at the skull base.
Discussion
During early embryonic development, posterior cerebral vascularization relies on the neural longitudinal arteries, which are the precursors of the vertebral arteries and the basilar artery. These primordial vessels emerge very early and run along the developing brainstem. At this stage, the vertebral arteries have not yet formed, and the posterior brain depends on anastomoses between the anterior carotid system and these neural longitudinal arteries. These include several important transient arteries, such as the embryonic trigeminal artery, the embryonic otic artery, the embryonic hypoglossal artery, and the embryonic proatlantal artery [ ].
Each of these anastomoses temporarily allows the internal carotid artery to supply the posterior cerebral structures, including the brainstem, until the vertebral and basilar arteries are fully developed. These connections persist during the early weeks of embryonic development, typically up to the sixth week of gestation, when the vertebral arteries form from the cervical intersegmental arteries. The right and left vertebral arteries then ascend along the cervical spine to merge at the base of the brain, forming the basilar artery [ ].
At this point, the posterior circulation becomes fully established, and the embryonic anastomoses progressively regress and disappear [ ].
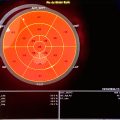
If this regression does not occur correctly, these primitive anastomoses persist, forming persistent carotid-vertebrobasilar anastomoses. This means that the vertebrobasilar system remains partially or entirely dependent on blood flow from the internal carotid artery through these anastomoses. These abnormal connections give rise to vascular variants, [ ].( Fig. 1 ):
- ✓
Persistent trigeminal artery: This is the most common variant, with a prevalence of 0.1%-0.2%. It connects the ICA at the cavernous level to the basilar artery.
- ✓
Persistent hypoglossal artery: With a prevalence of 0.03%-0.09%, it emerges from the cervical ICA, usually at the C1-C2 level, and traverses the hypoglossal canal to join the basilar artery.
- ✓
Persistent otic artery: It connects the ICA to the basilar artery via the path of the vestibulocochlear nerve.
- ✓
Persistent proatlantal intersegmental artery: This variant links the ICA or external carotid artery (ECA) to the vertebral artery. It has 2 subtypes:
Type I: Originates from the ICA and connects to the vertebral artery at the C1-C3 levels.
Type II: Originates from the ECA and joins the vertebral artery at the same levels.