Abstract
Negative pressure pulmonary edema (NPPE) is a rare, underdiagnosed, and potentially dangerous postoperative complication with the prevalence of 0.05%-0.1%. An 18-year-old healthy and athletic male developed a sensation of a lump in the throat, hemoptysis, wheezing, and acute respiratory failure, after an extubation following general anesthesia for an uncomplicated appendectomy. Computed tomography showed extensive bilateral pulmonary edema. He was managed with supplemental oxygen, albuterol, and diuretic. Supplemental oxygen was weaned off on hospital day 3. The hospital course was complicated by presyncope from orthostatic hypotension secondary to over-diuresis. The pathophysiology, diagnosis, management, and outcome of NPPE are illustrated and discussed in this case report. Furthermore, this case highlights that clinicians should balance the benefit of removing fluid from lungs and the risk of hypovolemia with the cautious use of diuretic.
Introduction
Negative pressure pulmonary edema (NPPE), which is a noncardiogenic cause of pulmonary edema, is a rare postoperative complication [ ]. The prevalence of postoperative NPPE is estimated to be 0.05%-0.1% [ ]. Young, healthy, and athletic patients who underwent endotracheal intubation are at higher risk of developing this disorder, as they can generate the most negative intrathoracic pressure (up to −140cmH 2 O) [ , ]. Some studies suggest that smoking is also strongly associated with NPPE, as smoking increases upper airway reflex sensitivity [ ]. The majority of cases are related to upper airway occlusion – postanesthetic laryngospasm and/or endotracheal tube occlusion by biting [ ]. Herein, we report a case of acute hypoxic respiratory failure with bilateral pulmonary edema secondary to negative pressure pulmonary edema immediately after an appendectomy.
Case
An 18-year-old athletic male with no significant medical history presented with 1 day of right lower quadrant abdominal pain. He was diagnosed with acute appendicitis and underwent an uneventful laparoscopic appendectomy. He received 1.8L crystalloid between the Emergency Department and the operating room. The duration of intubation was 63 minutes from intubation to extubation. The intubation was remarked as uneventful with a size 7 ET tube. Induction of anesthesia was achieved with rocuronium 50 mg, midazolam 2 mg, sevoflurane, and propofol a total of 250 ug during the case. Following emergence from the general anesthesia, he experienced a sensation of a lump in the throat. He had 2 episodes of continuous cough that lasted for 5-10 minutes with acute fall in oxygen saturation. During these episodes, he expectorated about 20ml of frothy blood-tinged fluid. The patient’s vital signs were as follows: temperature, 36.6°C; heart rate, 112 beats/min; respirations, 22 breaths/min; BP, 113/69 mmHg; and oxygen saturation, 80% on 3L NC with an FiO2 of 33 percent. Pulmonary examination was notable for respiratory distress with wheezing. Oropharynx and cardiac examination were unremarkable. No jugular venous distension, skin rash, clubbing, or peripheral edema was present. Albuterol nebulization of 3 mL was given with some subjective transient improvement and was repeated a total of 3 times. 50 minutes later, patient had another episode of hemoptysis and wheezing with increasing oxygen requirement from 3L nasal canula to 50% venti-mask with a flow rate of 10L which improved the patients SpO2 to 96 percent.
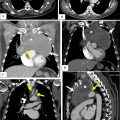
Postoperation laboratory result shows WBC 30.4 × 1000/uL, hemoglobin 14.9 g/dL, and platelets 331 × 1000/uL. The comprehensive metabolic panel, coagulation profile, and NT-proBrain natriuretic peptide were normal. The chest x-ray ( Fig. 1 A) revealed bilateral perihilar airspace opacities. The subsequent chest computed tomography (CT) ( Fig. 2 A-B) showed extensive patchy airspace opacities throughout the lungs bilaterally, more prominent centrally with a slight basilar predominance.



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree