Practical Aspects of Endocavitary Beam Therapy and Brachytherapy
Key Points
Endocavitary beam therapy can be an excellent method for delivering boost doses to selected patients presenting with accessible, well-circumscribed oral cancer.
Brachytherapy, performed by an experienced team, either alone or as a supplement to external beam radiation, can yield high tumor control rates with low toxicity profiles in selected patients.
Most brachytherapy is currently delivered by using remote-controlled afterloaders that insert radioactive (192Ir) sources.
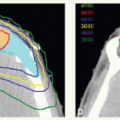
Currently available brachytherapy equipment and planning systems allow the flexibility to adjust radioactive source dwell time or intensity to optimize dose distribution.
Endocavitary beam therapy is a valuable method of delivering boost doses to well-circumscribed lesions in the anterior oropharynx or oral cavity as an alternative to brachytherapy or higher doses of external beam therapy. We use an orthovoltage x-ray beam of 125 to 250 kVp for this mode of therapy.
Traditionally, brachytherapy has had an important role in the radiotherapeutic management of cancers of the oral cavity. However, better reconstructive surgical techniques for filling defects that are left after tumor excision and for enhancing organ function have decreased the use of brachytherapy for these tumors. The availability of intensity-modulated radiation therapy may also reduce the application of brachytherapy.
Brachytherapy is sometimes used to deliver additional boost doses to residual infiltrative disease of the tongue base after external irradiation or to treat selected lesions involving the buccal mucosa, lip, oral commissure, and nasal vestibule and recurrent tumors of the nasopharynx. In addition, occasional patients with tumors of the oral tongue or floor of mouth who decline surgery are treated primarily with brachytherapy.
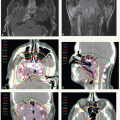
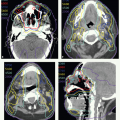
ENDOCAVITARY THERAPY INDICATIONS AND PROCEDURES
Ideal candidates for endocavitary beam therapy are those with a well-circumscribed lesion that is visible and accessible by cone through the mouth and does not involve the mucoperiosteum of the mandible (e.g., cancers of the soft palate or anterior faucial pillar). Patients with an exaggerated gag reflex are not suitable for this type of treatment.
A patient selected for endocavitary beam (intraoral cone) therapy generally receives this treatment component before external beam therapy for better tumor localization. Patients also tend to tolerate intraoral cone therapy better before the manifestation of mucositis induced by external beam irradiation. After a cone of appropriate size is selected, it is sometimes possible to manufacture a stent
for automatic cone positioning (see Chapter 8



for automatic cone positioning (see Chapter 8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree