Practical Aspects of External Beam Therapy
Key Points
Patient positioning, immobilization, and placement of an isocenter (or a reference point) are critical components for planning external beam radiotherapy.
Supine position is most desirable for the vast majority of patients.
Use of radiopaque markers can aid delineation of target volume.
Positional or shielding stents are useful for decreasing radiation dose to normal tissues in certain cases.
CT-based plan with heterogeneity correction is the current standard method.
Intensity-modulated radiation therapy (IMRT) is increasingly used for treating head and neck cancer for improving target volume coverage around the skull base (e.g., nasopharyngeal and sinonasal carcinomas) and for reducing radiation exposure of normal tissues such as salivary glands, cranial nerves, spinal cord, brain stem, etc.
Unilateral radiation is preferred for selected patients with lateralized neoplasms such as cancer of the buccal mocosa, retromolar trigone, parotid, etc.
Bolus, missing tissue compensator, and other devices can improve dose distribution but their use is diminishing with the introduction of IMRT that provides better conformation of radiation to the target volumes.
PATIENT POSITIONING
The supine position is most frequently used to deliver radiation with the conventional technique or intensity-modulated radiation therapy (IMRT). An isocentric technique is applied for matching opposed-lateral fields or IMRT upper neck portals to an anterior or anterior-posterior (AP-PA) lower neck portal(s).
The “open neck” position, in which the head is rotated on the trunk, resulting in flattening of the contours of the neck, is used for irradiating lateralized tumors and the ipsilateral neck. This position is suitable for irradiations with adjoining appositional electron fields or with a wedge-pair photon portal matched to an appositional electron field for lower neck.
The true lateral position is used in very select cases, for example, postoperative situations in which patients are unable to control secretions in the supine position but nonetheless need to be treated with opposed-lateral fields.
The seated position is used very rarely, primarily for those who have difficulty managing their secretions or those who have difficulty breathing in the supine position. Treatment is accomplished using a specially designed chair mounted to the treatment couch. This chair enables the same immobilization and allows the same treatment accessories to be used as in the supine position. The chair is used only if other options are not feasible because complex treatment planning and dosimetry are difficult and because computed tomography (CT) scanners cannot accommodate patients in this position.
PATIENT IMMOBILIZATION
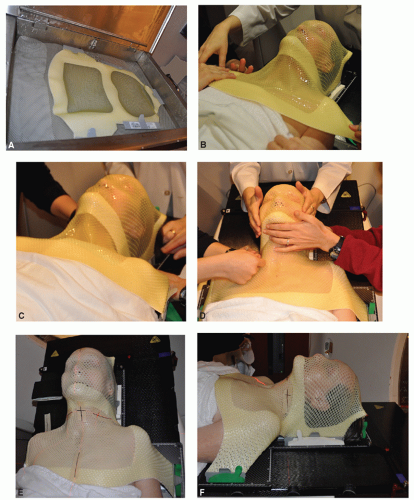
Virtually all patients nowadays are immobilized with thermoplastic masks that are individually made in the desired treatment position. A variety of commercial
neck pads and head holders are available for the purpose of immobilization in different positions. When making a mask, care should be taken to stretch the thermoplastic sufficiently thin to avoid unwanted bolus effect. For treatments limited to the neck region, the mask can be constructed so as to avoid the portals altogether. Figures 3.1 and 3.2 outline briefly the general procedure of constructing immobilization devices.
neck pads and head holders are available for the purpose of immobilization in different positions. When making a mask, care should be taken to stretch the thermoplastic sufficiently thin to avoid unwanted bolus effect. For treatments limited to the neck region, the mask can be constructed so as to avoid the portals altogether. Figures 3.1 and 3.2 outline briefly the general procedure of constructing immobilization devices.
Introduction of IMRT to reduce radiation morbidity or to escalate radiation dose to improve tumor control demands more precise and reproducible immobilization technology. Several methods have been introduced, which can be grouped into invasive and noninvasive techniques. Invasive techniques use head immobilization frames similar to those used for stereotactic radiosurgery. The frame is affixed to the patient’s skull by several screws, usually placed by a neurosurgeon.
Numerous noninvasive immobilization techniques have been described. They are based on thermoplastic mask immobilization or customized polyurethane cradles. Thermoplastic masks can be reinforced with additional straps to increase rigidity. Some systems add individualized cradles for support of the occiput. We currently use a longer headboard for attachment of a mask that extends from the vertex of the scalp to the upper chest, giving additional support to the upper neck and shoulder (Fig. 3.1).
RADIOPAQUE MARKERS AND STENTS
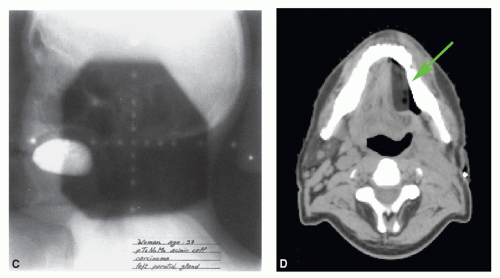
Although CT scan-based simulation and dosimetry are widely used, radiopaque markers can still be useful for delineating the scars and, in select cases, the primary lesion. It is important to realize that it is often difficult to visualize superficial tumors in the diagnostic or planning CT scan. This simple procedure helps in designing treatment portals to minimize the risk of a geographic miss and to avoid unnecessary inclusion of normal tissues. Several types of custom-made stents are useful in reducing the volume of normal tissues irradiated.
Wires and seeds placed on the skin, on the thermoplastic mask, or inserted into the tissue are helpful in marking the boundaries of the primary tumor, nodal biopsy sites, or surgical scar.
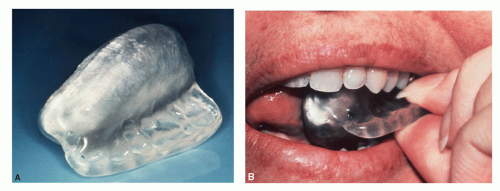
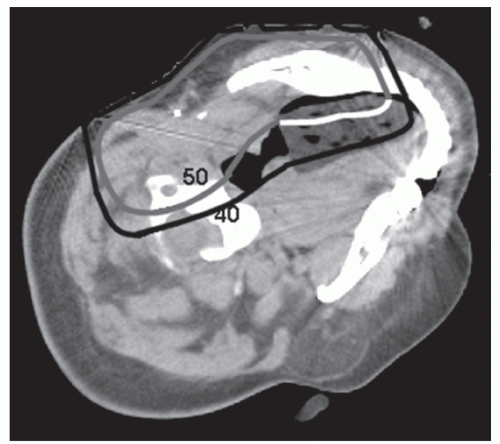
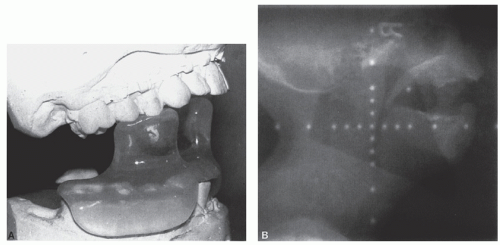
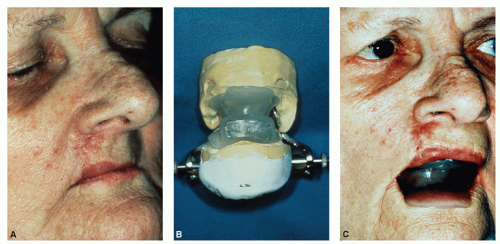
Stents can be custom-made, such as those used to depress or shield the tongue or to protrude the lip. In general, these devices can be categorized into two basic types: shielding stents and positional stents. A shielding device serves to reduce the radiation dose administered to normal tissues by incorporating shielding material, whereas a positional device serves to displace normal tissues out of the treatment fields (Figs. 3.3, 3.4, 3.5, 3.6 and 3.7).
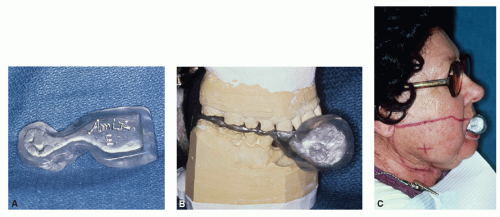 Figure 3.4 A 66-year-old woman presented with a right buccal mucosa lesion. On physical examination, she was found to have an infiltrative tumor measuring approximately 3.5 cm in largest diameter, extending anteriorly almost to the oral commissure. The tumor was 1.0 to 1.5 cm thick, without apparent skin involvement. There were two right submandibular nodes palpable, the largest measuring 2 cm in diameter. Biopsy revealed squamous cell carcinoma. The patient underwent resection of the tumor and a right modified neck dissection. Pathologic examination revealed a well-differentiated squamous cell carcinoma of the buccal mucosa with microscopic extension into the skeletal muscle and skin of the cheek. Nine lymph nodes were recovered in the surgical specimen, four of which contained metastatic squamous cell carcinoma with extension beyond the capsule. The patient received postoperative radiotherapy. The tumor bed and right upper neck were subjected to an ipsilateral appositional 13-MeV electron field to a given dose of 60 Gy in 30 fractions. The ipsilateral mid and lower jugular nodes and the posterior cervical chain were encompassed by a 9-MeV electron field. These areas were treated to a given dose of 50 Gy in 25 fractions. The scar extending into the mid neck was given a 4-Gy boost with 6-MeV electrons. A variation of the stent as described in Figure 3.3 was used for this patient. As in the previous case, the stent-containing cerrobend was placed between the alveolar processes and the tongue, serving to displace the tongue and to shield the tongue and contralateral oral mucosa. In this case, the right oral commissure needed to be included in the field and, therefore, fall off was required anteriorly. The stent protruded anteriorly to shield the contralateral part of both lips and the left oral commissure. A: Lateral view. B: Stent mounted on an articulator. C: Anterior end of the stent protrudes through the mouth for shielding part of the lips and the left oral commissure. (From Kaanders JHAM, et al. Devices valuable in head and neck radiotherapy. Int J Radiat Oncol Bio Phys 1992;23:639-645.) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree