Practice Examples and ‘Fascinomas’
The final chapter consists of two sections. For the first, I have collected a series of chest radiographs on which to practise the diagnostic skills described so far. The concluding section contains some fascinating radiographs encountered over the years. Although ‘fascinomas’, by definition, are rare and you may never come across an example yourself in clinical practice, these radiographs are, I believe, instructive in their own right and illustrate the power of systematic observation – one of the basic themes of this book.
PRACTICE EXAMPLES
Examine the radiographs that follow – each of them is accompanied by short clinical notes in the legend. Follow the investigative approach described in earlier chapters, take time to record all of the abnormalities and then make an attempt at a diagnosis. Your observations and conclusions can be checked with the answers that follow.
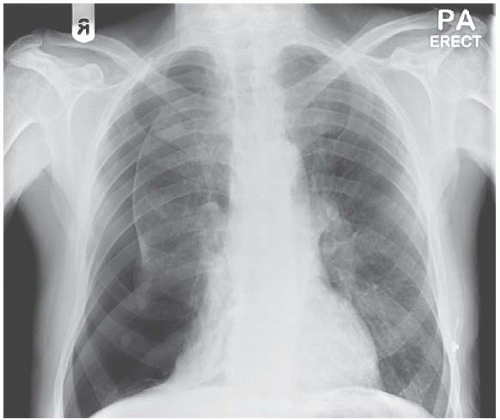 Figure 7.2 Take time to collect all of the information. Then look at Figs 7.3 and 7.4. |
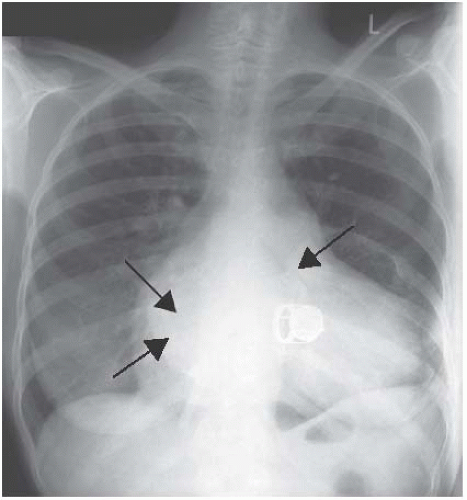 Figure 7.6 There are lots of abnormalities on this radiograph and they come together to tell quite a story about this woman who suffered rheumatic fever in childhood. |
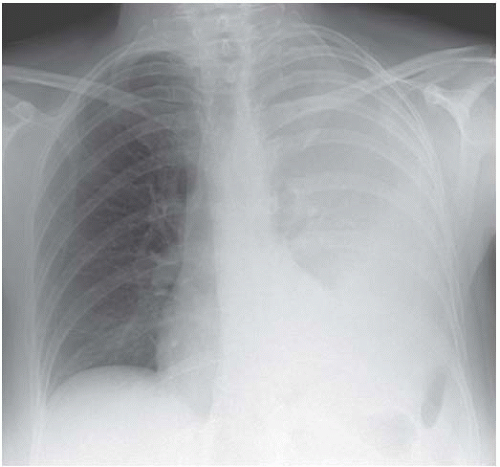 Figure 7.7 Weight loss and fever were the presenting complaints and this woman was severely cachectic when she finally came to hospital. How will you manage the problem? |
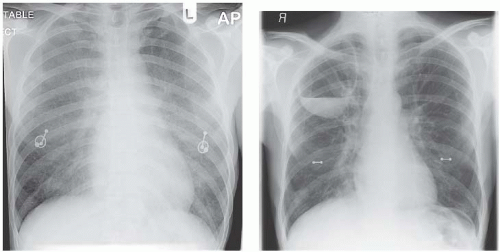
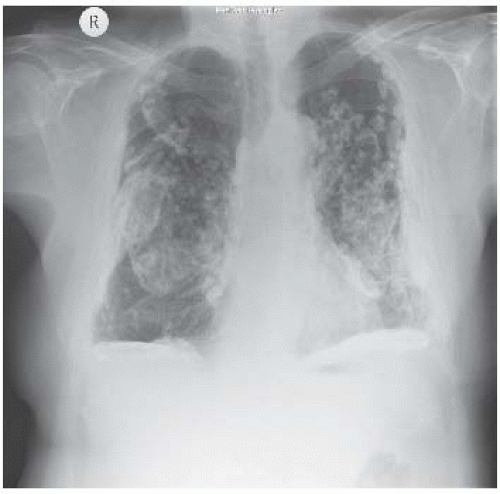
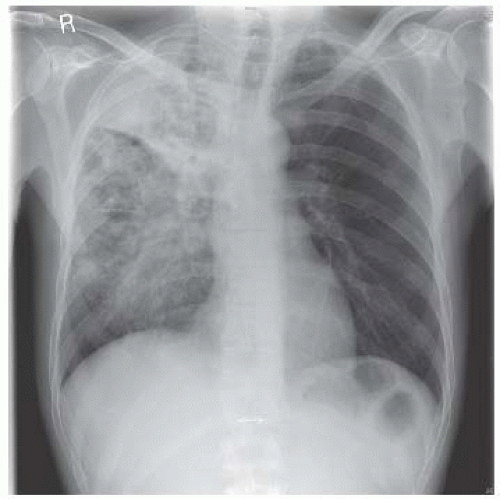 Figure 7.10 The presenting complaints were night sweats and weight loss in both of these patients. Describe the radiographic abnormalities in each X-ray. What is the most likely diagnosis? |
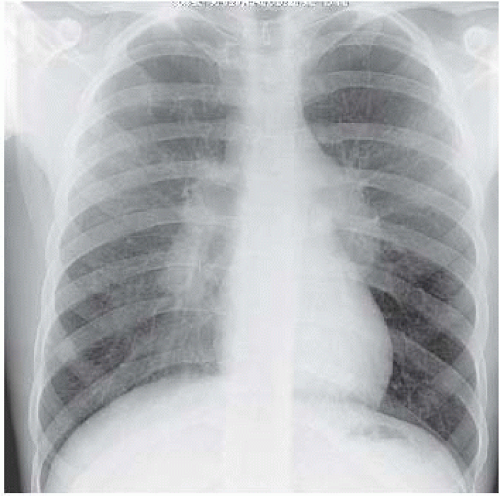 Figure 7.11 The combination of mediastinal and parenchymal lung abnormalities should suggest a particular diagnosis. How do you think this patient (who was in his twenties) might have presented? |
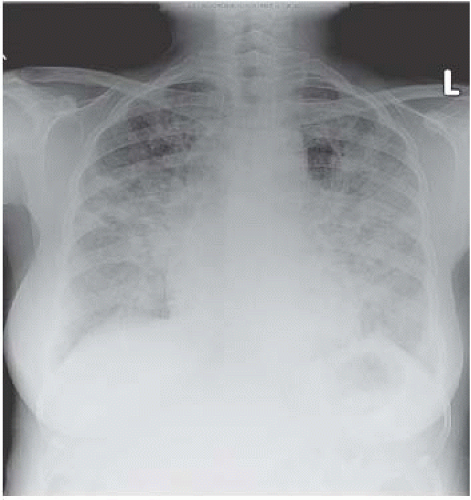 Figure 7.16 Here is another pulmonary infiltrate. Describe the nature of the shadowing and its distribution. |
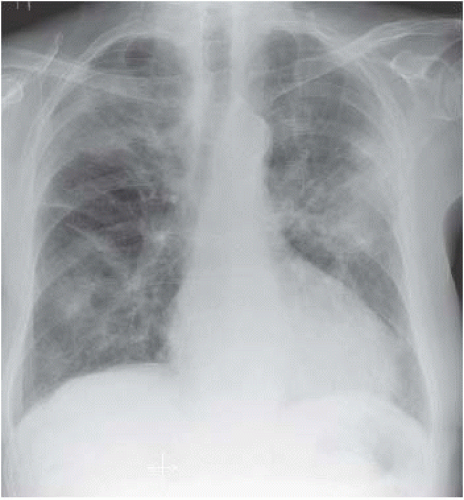 Figure 7.18 The parenchymal lung appearances are quite different here. Just describe what you see and suggest some diagnoses. This was a very unusual case. |
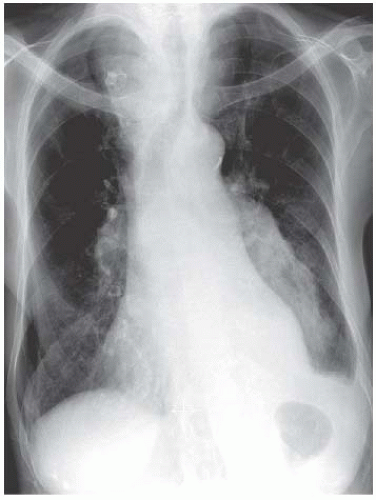 Figure 7.20 This elderly woman has a large mass in the left lower zone which proved to be a carcinoma of the bronchus. There is another abnormality, what is it? |
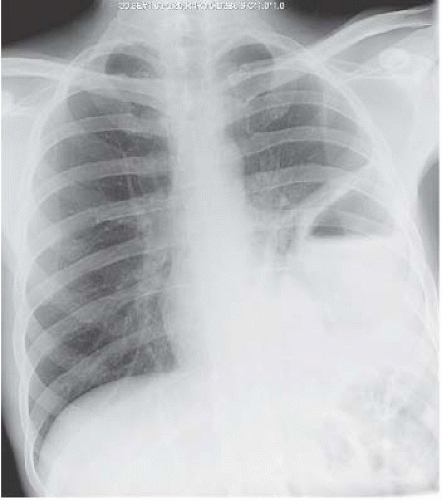 Figure 7.21 Describe the abnormalities. What is the likely diagnosis? How would you manage this problem? |
ANSWERS
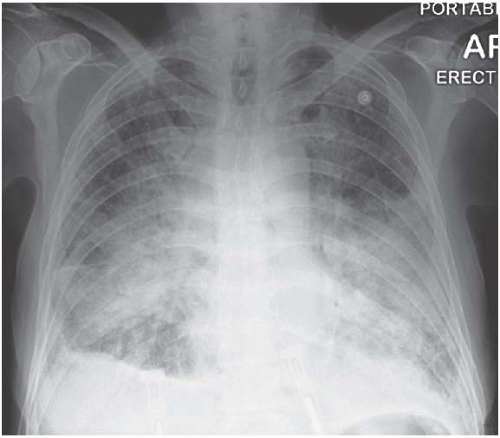
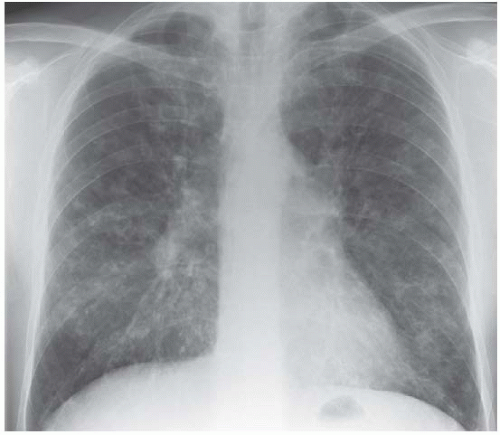
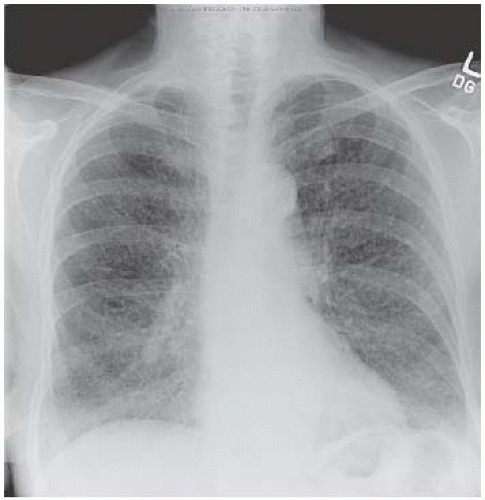
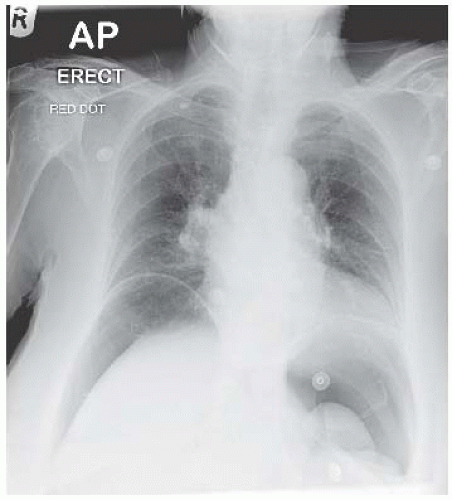
Figure 7.1. Pulmonary infiltration is perihilar in distribution and has coalesced to produce an alveolar-filling pattern. This is an antero-posterior (AP) film and it is impossible to comment on heart size but there is pleural fluid, certainly on the right. The intrapulmonary shadowing is too dense to see septal lines, but the most likely diagnosis is left ventricular failure. However, other possibilities exist, including alveolar haemorrhage, adult respiratory distress syndrome, pneumocystis pneumonia and pulmonary alveolar proteinosis.
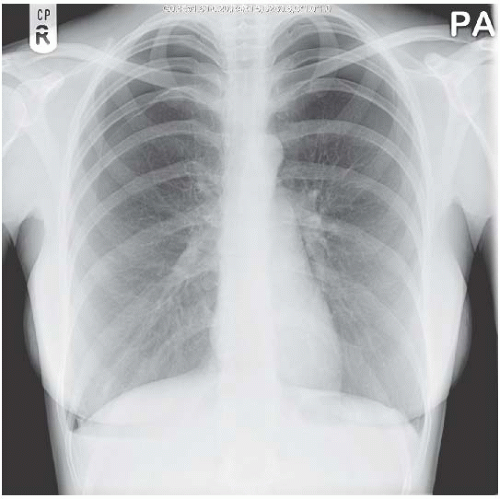
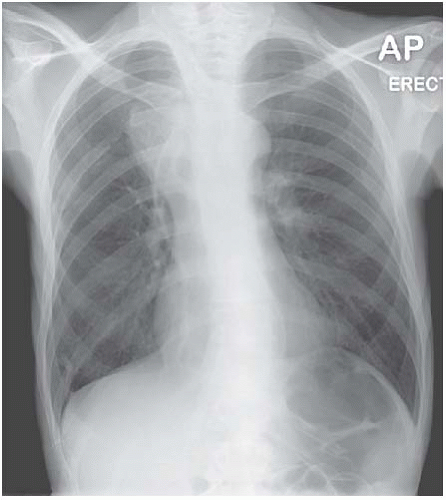
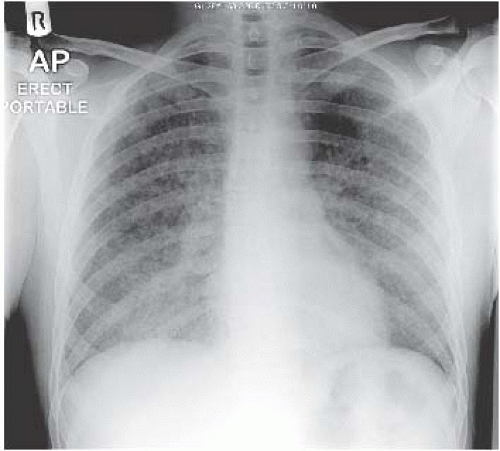
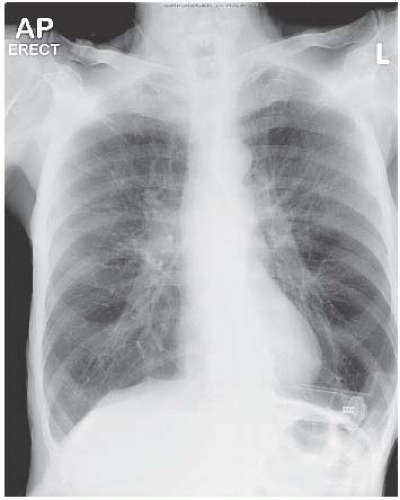
Figure 7.2. This shows a large right-sided pneumothorax and the right lower lobe is completely collapsed (diagonal shadow adjacent to right heart border). The proximal pulmonary vessels are prominent and this was a secondary pneumothorax in a man who had been a life-long heavy smoker.
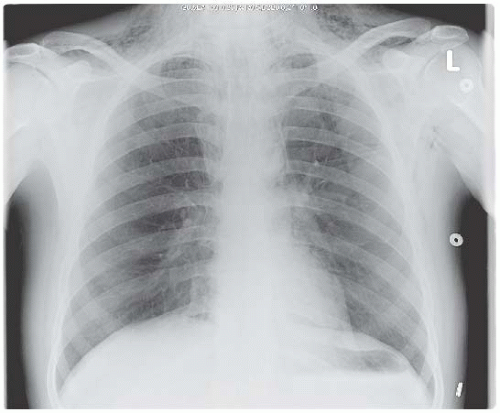
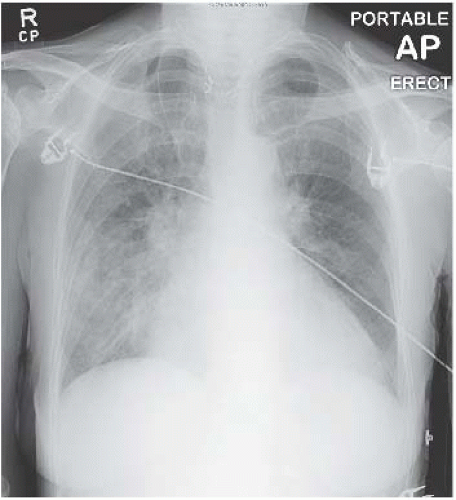
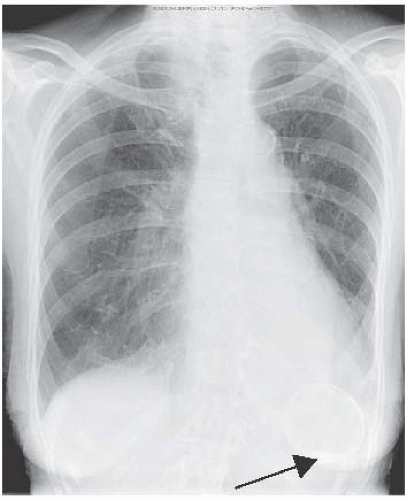
Figure 7.3. This shows bilateral pneumothoraces in a young woman (note the breast shadows). Spontaneous pneumothoraces are possible of course, particularly if she was tall and thin, but consider possible underlying pathology in a young woman – catamenial pneumothorax is unlikely as these are bilateral and there was a primary lung problem in the form of lymphangioleiomyomatosis (see Chapter 4, page 88).
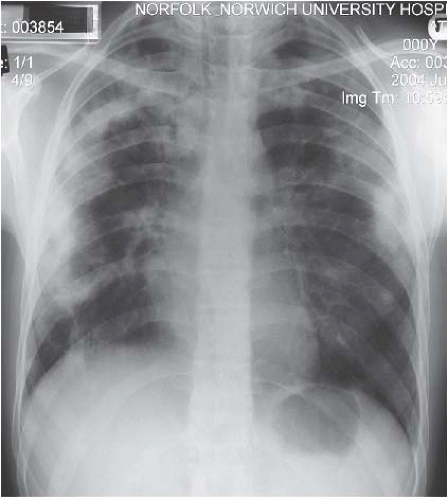
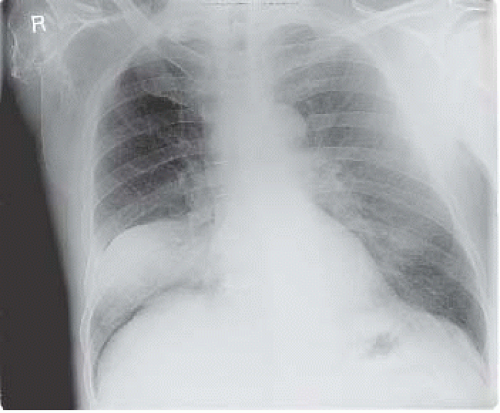
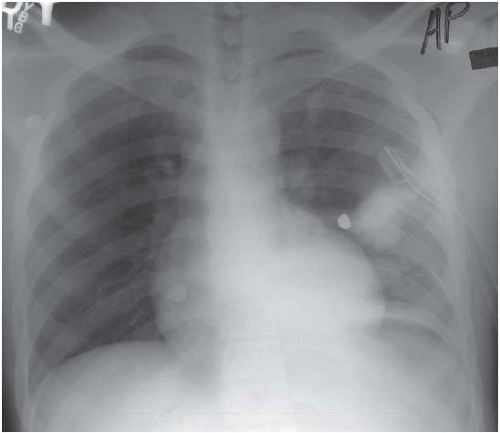
Figure 7.4. A pneumothorax is not evident but there is air in the mediastinum and in the soft tissues of the neck. This was a complication of acute severe asthma but oesophageal perforation should be considered as well.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree