Preoperative Portal Vein Embolization
David C. Madoff
David Li
Surgical resection offers the best chances for long-term survival of patients with primary and metastatic diseases confined to the liver (1,2). Major hepatic resection (i.e., greater than three Couinaud segments) places patients at risk for developing complications related to liver insufficiency in the perioperative period. The anticipated volume of liver which remains after surgery, termed the future liver remnant (FLR), has been shown to be a strong, independent predictor of postoperative complications (3,4). Portal vein embolization (PVE) is an important tool in the preoperative management of select patients with “marginal”
anticipated FLR volumes prior to major hepatectomy (5,6). Embolization of the portal vein branches supplying the liver segments to be resected redirects blood flow to the nondiseased liver. This redistribution induces hypertrophy of the FLR, thereby making it possible for these patients, not previously considered as candidates to safely undergo major hepatectomy. PVE continues to demonstrate an essential adjunctive role to major hepatectomy, even as advances in hepatobiliary surgical techniques evolve and indications for curative hepatectomy expand, given its high safety profile and proven efficacy at promoting liver remnant hypertrophy.
anticipated FLR volumes prior to major hepatectomy (5,6). Embolization of the portal vein branches supplying the liver segments to be resected redirects blood flow to the nondiseased liver. This redistribution induces hypertrophy of the FLR, thereby making it possible for these patients, not previously considered as candidates to safely undergo major hepatectomy. PVE continues to demonstrate an essential adjunctive role to major hepatectomy, even as advances in hepatobiliary surgical techniques evolve and indications for curative hepatectomy expand, given its high safety profile and proven efficacy at promoting liver remnant hypertrophy.
Indications
1. Patients with primary or metastatic liver disease who are otherwise hepatic resection candidates, other than:
a. Normal underlying liver and a standardized future liver remnant (sFLR; see definition in the following text) less than 20% (3,7,8)
2. Patients with diabetes mellitus without underlying liver disease may benefit from PVE, as the magnitude of postresection liver hypertrophy is usually less in these patients (12).
3. Patients undergoing complex hepatectomy with concomitant extrahepatic surgery, particularly pancreatectomy. In this latter group, studies have demonstrated that hepatic regeneration is inversely proportional to the extent of pancreatectomy (7).
Contraindications
Absolute
1. Overt clinical portal hypertension
2. Extensive invasion of the portal vein precluding safe catheter manipulation and optimal delivery of embolic material
3. Complete lobar portal vein occlusion (right or left), as portal blood flow will already have been diverted (5)
Relative
1. Extrahepatic metastatic disease, including portal lymphadenopathy
2. Two-stage hepatectomy has expanded the number of patients with bilobar hepatic disease burden eligible for PVE and potential curative resection; however, diffuse hepatic disease burden remains a contraindication to PVE.
3. Tumor precluding safe access into the portal venous system (approach may vary on the basis of location of tumor—see discussion of ipsilateral and contralateral approaches in the following text)
5. Mild portal hypertension
6. Uncorrectable coagulopathy
7. Renal insufficiency
Preprocedure Preparation
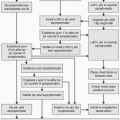
1. Future liver remnant determination
a. Liver volume is directly correlated with a patient’s size; hence, normalizing the anticipated liver volume to a patient’s size results in a more accurate assessment of the FLR. This principle led to the proposal and clinical validation of an sFLR (13).
TELV = – 794.41 + 1267.28 × BSA
where BSA is the body surface area.
d. Computed tomography (CT) is used to directly measure the FLR. Volumetric three-dimensional contrast-enhanced computed tomography (3D-CT) is essential for planning hepatic resection. Calculate the 3D-CT volumes by outlining the hepatic segmental contour area on each slice and summing individual slice volumes (contour area × slice thickness) (13).
(1) Check for portal vein patency and variant anatomy.
e. Most protocols acquire CT images immediately before PVE and approximately 3 to 4 weeks after the procedure to assess the degree of FLR hypertrophy. In addition to sFLR, the degree of hypertrophy (DH) and kinetic growth rate (KGR) are also used as predictors of postoperative course (15). DH = FLR / TELV (post-PVE) – FLR / TELV (pre-PVE). KGR = DH / no. of weeks elapsed after PVE. Patients whose DH is <5% or KGR <2.0% per week have higher postoperative complication rates. DH and KGR serve as additional measures for determining whether or not the involved liver is ultimately resected.
f. If the sFLR is considered inadequate to allow for safe hepatic resection on the initial follow-up CT scan, additional “waiting time” may be useful as regeneration may still occur albeit as a slower rate dependent on DH and KGR.
2. Patients are usually admitted the night before the procedure and kept nil per os (NPO). Informed consent is obtained.
3. Intravenous (IV) antibiotic prophylaxis is usually not required. However, patients with biliary obstruction involving the liver to be resected and/or a biliary drainage catheter within the FLR should be given prophylactic antibiotics (ceftriaxone 1 g IV).
4. PVE can be performed under moderate IV sedation using a combination of fentanyl and midazolam. However, general anesthesia is recommended for patients with multiple comorbidities or for those who cannot cooperate.
5. Ultrasound examination is performed to verify patency of the intended access branch to the portal vein immediately before the procedure.
Procedure
1. Although PVE can promote hypertrophy of either lobe, left PVE is not commonly performed because left hepatectomy results in a remnant liver volume that is sufficient enough that post-hepatectomy liver failure will be unlikely (16




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree