Abstract
Primary sternal osteomyelitis is an uncommon but challenging condition that frequently poses diagnostic difficulties. Imaging plays a crucial role in both diagnosing the condition and assessing potential complications. Treatment typically involves a combination of surgical drainage and a prolonged course of antibiotics. We report the case of a 17-year-old immunocompetent male who presented with chest pain. Laboratory investigations revealed elevated inflammatory markers, and blood cultures, along with contrast-enhanced computed tomography, confirmed the diagnosis of primary sternal osteomyelitis. The patient was started on dual antibiotic therapy and underwent surgical drainage, with subsequent favorable clinical and radiological progression.
Introduction
Primary sternal osteomyelitis (PSO) is an uncommon entity, with fewer than 20 cases reported in the literature to date [ ]. PSO typically originates from a hematogenous source or results from direct extension of an adjacent infection. Risk factors include obesity, HIV, and diabetes mellitus, among others. However, cases have been documented in the absence of these risk factors [ ].
The aim of sharing this case is to describe a rare instance of primary Staphylococcus aureus sternal osteomyelitis in an immunocompetent adolescent and to underscore the critical role of imaging in making an accurate diagnosis, guiding treatment, and facilitating follow-up.
Case report
We report the case of a 17-year-old immunocompetent male with no significant past medical history, including no recent trauma, who presented to the emergency department with a chief complaint of chest pain. The pain, localized to the sternum, had been progressively worsening over the past week. It was described as sharp and constant. The patient also reported a cough but denied hemoptysis, shortness of breath, night sweats, or weight loss.
On physical examination, the patient was febrile and had a maculopapular rash affecting the entire trunk. Palpation of the sternum revealed localized tenderness, but there was no visible swelling. His vital signs were otherwise within normal limits.
Early investigations revealed leukocytosis with a white blood cell count of 20 × 10^9/L (normal range 4-11 × 10^9/L) and a significantly elevated C-reactive protein level of 320 mg/L (normal range <6 mg/L).
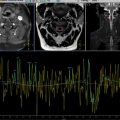
A chest X-ray was performed initially and showed no abnormalities ( Fig. 1 ).

In light of the diagnostic uncertainty, a computed tomography (CT) scan was quickly performed. The scan showed presternal and retrosternal soft tissue swelling with gas and peripheral enhancement, findings that were consistent with septic arthritis and osteomyelitis of the sternum, along with abscess formation ( Fig. 2 ).

Blood cultures was made
The patient was initially started on intravenous empiric antibiotic therapy with Ceftriaxone (2 g every 24 hours) and Vancomycin (15 mg/kg every 12 hours). In addition, he underwent surgical drainage, which revealed a large purulent peristernal abscess extending into the retrosternal space. The procedure involved careful incision and drainage of the abscess, followed by debridement to remove necrotic tissue and ensure adequate drainage. Cultures were obtained from both the abscess and blood samples.
Following confirmation of Staphylococcus aureus from both the blood and abscess cultures, the antibiotic regimen was adjusted based on the susceptibility profile. The patient was transitioned to Cefazolin (2 g every 8 hours) and continued on Vancomycin to ensure adequate coverage. The total duration of antibiotic therapy was planned for 6 weeks, based on clinical progress and microbiological results, to ensure complete resolution of the infection.
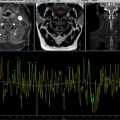
A follow-up CT scan performed 10 days after the initial treatment showed a marked reduction in the size of the abscess collections ( Fig. 3 ). The patient was then closely monitored, and clinical improvement was observed, with a gradual resolution of symptoms. At the subsequent follow-up visit, the patient reported no recurrence of chest pain or fever, and his physical examination revealed no signs of infection. The patient continued on a course of Cefazolin and Vancomycin for a total of 6 weeks, completing the full course without any adverse effects. At the final follow-up, there were no further complications, and the patient had returned to normal activity.