KEY FACTS
Imaging
- •
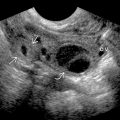
Grayscale US
- ○
Prostate carcinoma (PCa) can appear as hypoechoic (60-70%), isoechoic/invisible (30-40%), rarely hyperechoic ± asymmetric capsular bulging or irregularity
- ○
- •
Color Doppler US
- ○
PCa may be hypervascular; however, absence does not exclude cancer, and other benign entities (e.g., prostatitis) may also be hypervascular
- ○
- •
Transrectal US (TRUS) is imaging of choice to guide biopsy in evaluation for PCa but performs poorly in cancer detection and staging
- •
Calculate prostate volume using largest cross-sectional image in transverse and mid sagittal planes: Transverse x AP x long x 0.52
- •
MR imaging
- ○
Most sensitive imaging technique for PCa diagnosis and staging
- ○
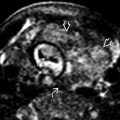
Peripheral zone (PZ): T2 dark lesion with restricted diffusion; transition zone (TZ): Erased charcoal sign on T2WI
- ○
Targeted MR-guided and MR/US fusion-guided biopsy is promising for increasing detection of high-risk prostate cancer while reducing detection of low-risk cancer compared with standard biopsy
- ○
Pathology
- •
Most common noncutaneous malignancy in western world, 2nd most common cause of cancer deaths among men
- •
95% of tumors are acinar adenocarcinoma
- •
Staging based on tumor-node-metastasis staging, prostate specific antigen at time of diagnosis, and Gleason score
- •
Location of prostate cancer: PZ: 70-80%, TZ: 20%, central zone: 1-5%
Clinical Issues
- •
Management is complex due to difficulty in accurate staging and in predicting speed of disease progression
- •
Despite having higher volumes and prostate-specific antigen values at diagnosis, TZ cancers are less likely to be associated with seminal vesicle, extraprostatic and lymphovascular invasion
Scanning Tips
- •
Although classically PCa is hypoechoic on grayscale US, > 30-40% PCa may be invisible on TRUS
 , rectal wall
, rectal wall  , and symphysis pubis
, and symphysis pubis  .
.

 with capsular bulging and nodularity extending into the adjacent fat
with capsular bulging and nodularity extending into the adjacent fat  and left neurovascular bundle
and left neurovascular bundle  . A smaller hypoechoic lesion is seen in the right PZ
. A smaller hypoechoic lesion is seen in the right PZ  .
.
 in the left PZ lesion. The right PZ lesion is mildly hypervascular
in the left PZ lesion. The right PZ lesion is mildly hypervascular  . Prostatectomy revealed multifocal PCa, including Gleason 5 + 5 adenocarcinoma with left extraprostatic extension and lymphovascular and perineural invasion.
. Prostatectomy revealed multifocal PCa, including Gleason 5 + 5 adenocarcinoma with left extraprostatic extension and lymphovascular and perineural invasion.
 . About 70% of prostate cancers occur in the peripheral zone.
. About 70% of prostate cancers occur in the peripheral zone.
 around the mass. The increased vascularity of the left lobe may be due to its dependent position.
around the mass. The increased vascularity of the left lobe may be due to its dependent position.