Pulmonary System
QUESTIONS
1 Which one of the following sentences is true regarding the acquisition of perfusion images using Tc-99m MAA?
A. Rapid tight bolus injection is preferred over slower injection.
B. Perfusion scan should be performed before the ventilation scan.
C. Tc-99m MAA should be administered with the patient in the supine position.
D. Central venous catheter injection is preferred over peripheral venous injection.
E. Clinically significant pulmonary emboli can result if the blood is drawn into the syringe prior to Tc-99m MAA injection.
View Answer
1 Answer C. Because of the gradient created by gravity, the lung bases receive about three times the amount of blood flow compared to the apex when the patient is in the upright position. In order to minimize this gravity-induced physiologic perfusion gradient, Tc-99m MAA should be injected with the patient in the supine position. Also to allow proper mixing with blood and to prolong the bolus, peripheral vein injection is preferred and injection through the central venous catheter should be avoided. The injection should be slow over more than four respiratory cycles and have large enough volume to assist in homogeneous pulmonary distribution. Labeled blood clots formed by blood drawn into the syringe may result in focal hot spots on the perfusion scan; however, they are clinically insignificant. Since both DTPA and MAA are labeled with Tc-99m, sequential ventilation/perfusion images require smaller dose of the first imaging agent to prevent interference with the second. Because it is difficult to deliver high doses of aerosolized DTPA to the lungs and since better count statistics are preferred for the perfusion imaging, ventilation portion of the imaging is usually performed first. Because of the low photo peak and short biologic half-life, Xe-133 ventilation is also performed before the perfusion component of the study.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:197-200.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:206-209.
2 Ventilation images can be acquired with an aerosol such as Tc-99m DTPA or a gas such as Xe-133. Which of the following is an advantage of Tc-99m DTPA compared to Xe-133?
A. DTPA is more sensitive in the evaluation of airway disease.
B. DTPA does not interfere with subsequent MAA perfusion images.
C. DTPA has short biologic half-life with lower radiation exposure to the patient.
D. DTPA has better photon flux and allows acquisition of multiple projections.
View Answer
2 Answer D. Advantages of Tc-99m DTPA include the ability to acquire multiple projections, ready availability, and ideal photon energy resulting in better imaging. Disadvantages include interference with subsequent perfusion images from crosstalk as well as central clumping of the radiopharmaceutical in the setting of poor respiratory effort or increased air turbulence (i.e., COPD or asthma).
Advantages of Xe-133 compared to Tc-99m DTPA include superior sensitivity to detect COPD and lack of interference with the subsequent perfusion images owing to its short biologic half-life and low photo peak of 81 keV. Disadvantages include higher soft tissue attenuation due to low photon energy, inability to acquire multiple protections (with a single dose) or SPECT images due to rapid washout, and requirement of special exhaust system, traps, and negative air pressure rooms.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:198-200.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:211.
3 In which of the following instances can a normal MAA particle dose be administered to the patient?
A. Pregnancy
B. Right-to-left shunt
C. Pediatric population
D. Pulmonary hypertension
E. Saddle pulmonary embolus
View Answer
3 Answer E. Usually, 200,000 to 500,000 particles of MAA are administered to the patient undergoing a ventilation-perfusion study for the evaluation of pulmonary embolus. In children, this number is decreased to 10,000 for the neonates and 50,000 to 150,000 for children <5 years of age. Also, reduction in the particle dose (100,000 to 150,000) should be considered in patients with pulmonary hypertension, right-to-left shunt, and pregnancy. Saddle pulmonary embolus is not an indication for the reduction in the particle dose.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:197.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:206.
A. Xenon-133 and Tc-99m MAA
B. Tc-99m DTPA and Tc-99m MAA
C. Xenon-133 and Tc-99m DTPA
D. Tc-99m sulfur colloid and Tc-99m DTPA
E. Krypton-81m and Tc-99m DTPA
View Answer
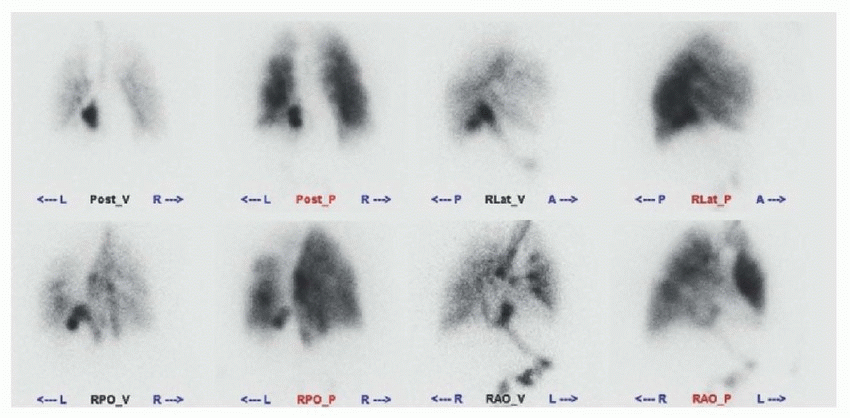
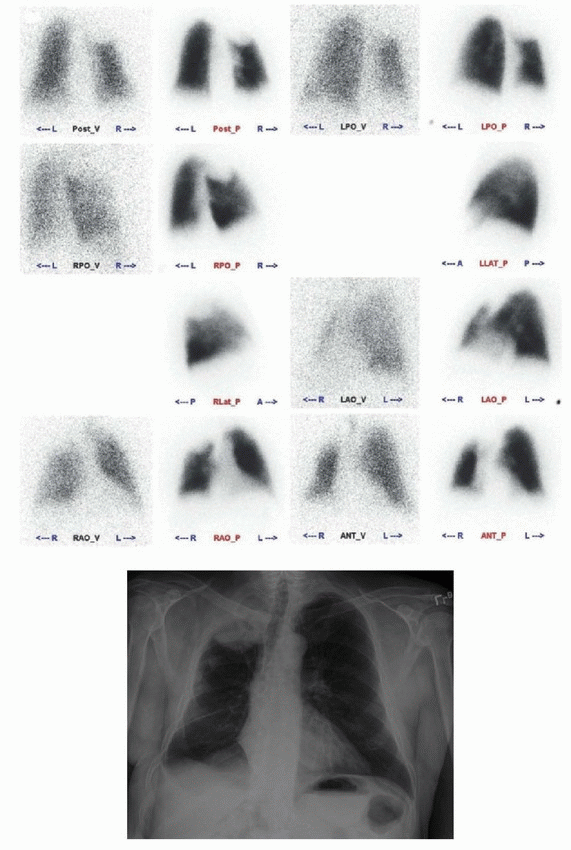
4 Answer B. The acquired ventilation images demonstrate a large focus of intense activity within the posterior upper abdomen toward the left of the midline in what appears to be the stomach (arrows); activity is also visualized in the proximal small bowl. Findings are secondary to swallowed aerosol particles. Deposition of the radiopharmaceutical is also identified within the trachea and central airways (arrowheads). These findings are seen with Tc-99m DTPA ventilation scan. Tc-99m DTPA is aerosolized using nebulizer into small particles. Because of its particulate nature, unlike ventilation performed with gas such as Xe-133, central accumulation of DTPA may occur in patients unable to cooperate with deep breathing or in patients who have increased central airway flow turbulence from COPD or asthma. Also, ingestion of the non-inhaled particles from the oral cavity may result in activity within the esophagus and stomach. This patient had a hiatal hernia (arrows in the chest X-ray below) explaining the activity in the posterior mediastinum. Tc-99m MAA is currently the only agent used for the lung perfusion imaging. Because majority of the particles (60% to 80%) range in size from 10 to 30 µm, it is appropriate for blockage of pulmonary capillaries, which measure approximately 10 µm in diameter. Since perfusion portion of the study is acquired after the ventilation, shine through of activity in stomach and central airways from the ventilation study is often seen on the perfusion images (as is the case with this patient).
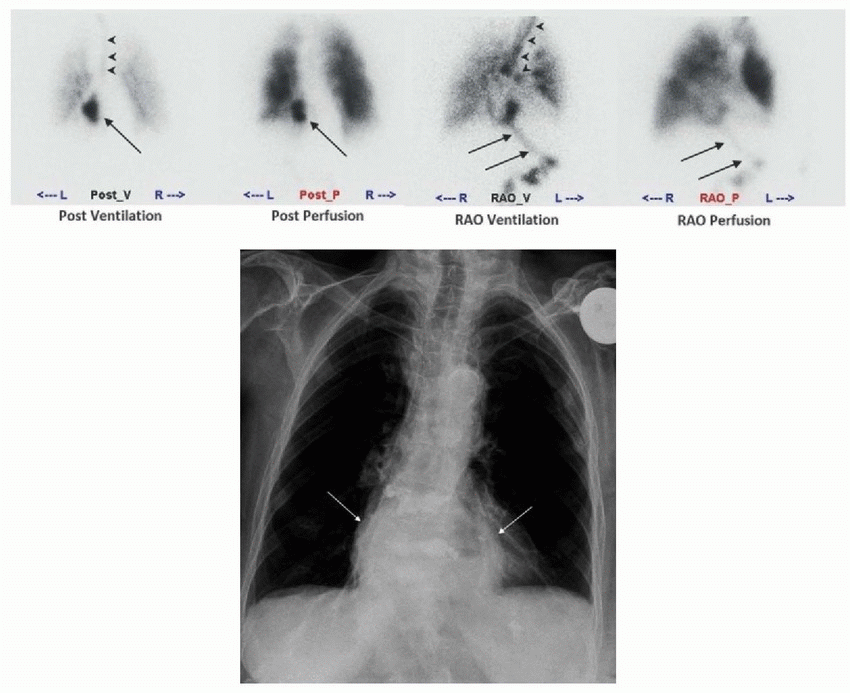 |
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:201-203.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:207, 209-210.
A. Radioiodine treatment
B. FDG-PET/CT
C. Liver function tests
D. Pulmonary function tests
E. CT chest
F. CT abdomen
View Answer
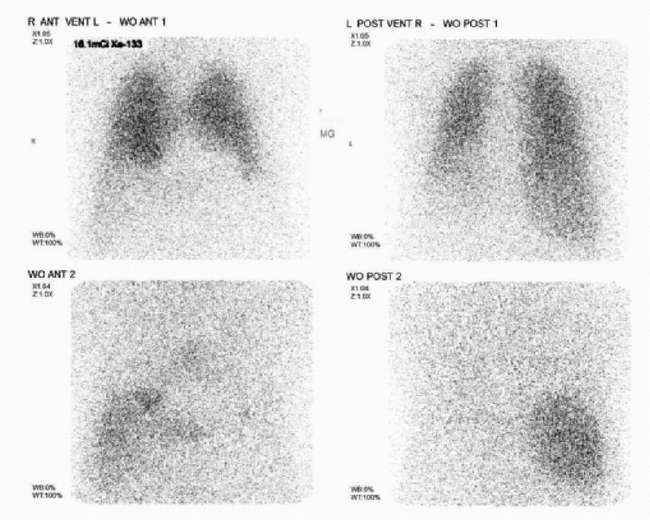
5 Answer C. The sequential anterior and posterior Xe-133 images demonstrate retention of Xe-133 within the right upper quadrant (arrow). This is typically seen in patients with fatty infiltration due to the retention of fat-soluble Xe-133 in the liver parenchyma. Liver function tests would be the most appropriate next step in this case and the other choices would not be appropriate. Retained Xe-133 uptake within the lungs on washout images is associated with air trapping from small airways disease. However, careful inspection of the images demonstrates that the retained radiopharmaceutical is in the liver and not in the lung parenchyma. When present, this finding should not be mistaken for trapping of Xe-133 in the right lower lung.
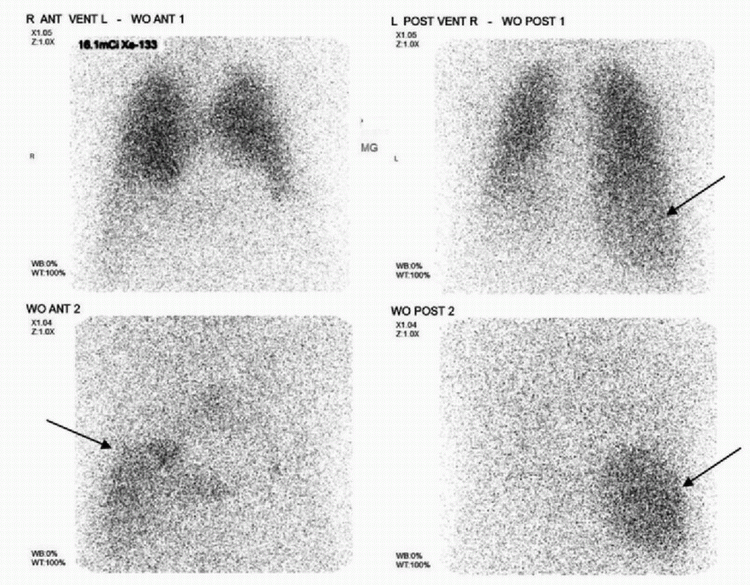 |
References: Conn HL Jr. Equilibrium distribution of radioxenon in tissue: xenon-hemoglobin association curve. J Appl Physiol 1961;16:1065-1070.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:208-211.
6 A 36-year-old pregnant female presents to the emergency department with chest pain. Which of the following is true regarding the CT pulmonary angiogram (CTPA) compared to the ventilation-perfusion scan (VQ) in this patient?
A. CTPA has lower specificity.
B. CTPA has lower fetal radiation exposure.
C. CTPA has lower maternal breast radiation exposure.
D. CTPA has lower maternal total body radiation exposure.
View Answer
6 Answer B. Even though CT pulmonary angiogram (CTPA) may be the initial test of choice to diagnose pulmonary embolus, maternal radiation dose is higher with CTPA (3 to 5 mSv) compared to the V/Q scan (2 mSv or less). While CT scans with newer detector technology can reduce maternal dose further, CTPA delivers higher radiation to the breast tissue compared to the V/Q scan, increasing the risk of breast cancer. On the other hand, even with reduced dose (1 to 2 mCi of Tc-99m MAA), fetal dose from the V/Q scan is higher than with the CTPA. According to the PIOPED II trial, VQ scan and pulmonary CT angiogram performed about equally in the diagnosis of pulmonary embolism. However, the specificity of CTPA for pulmonary emboli detection is greater than that of the V/Q scan. Other weaknesses of V/Q scan include longer examination time and lack of ready availability as the preparation of radiopharmaceutical requires extra time.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:203-204.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:204-205.
A. Cardiac MRI
B. CT angiography
C. Planar images of the brain
D. Contrast echocardiography
View Answer
7 Answer C. Anterior and posterior perfusion images demonstrate activity within the spleen (arrows) and kidneys (arrowheads). Activity is not visualized within the stomach (as would be expected with free pertechnetate). As such, findings represent right-to-left shunt, which should be confirmed with planar images of the brain. Visualization of activity within the brain would indicate a right-to-left shunt. Since Tc-99m pertechnetate cannot cross the blood-brain barrier, absence of radiotracer uptake within the brain would confirm free pertechnetate. Activity within the kidneys and thyroid may be seen due to either free pertechnetate or right-to-left cardiac shunt. When seen, planar images of the brain should be acquired to differentiate between the two.
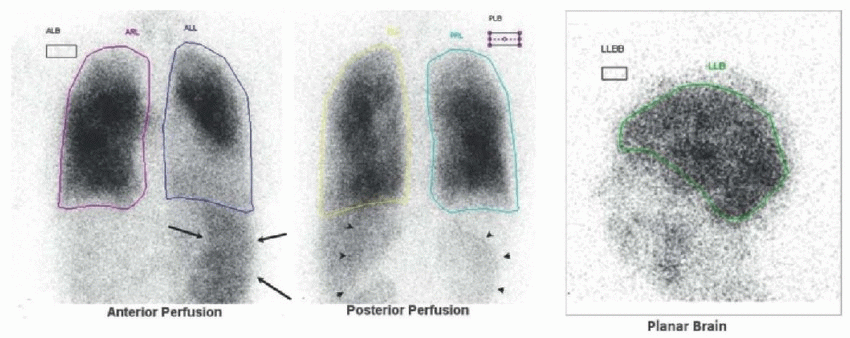 |
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders; 2012:203, 197-198.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders; 2014:211-212.
8 What degree of FDG uptake is typically associated with a pulmonary hamartoma?
A. Less than that of the mediastinum
B. Greater than mediastinum but less than liver
C. Greater than liver but less than bladder
D. Greater than bladder
View Answer
8 Answer A. Pulmonary hamartomas generally have no significant uptake (less than the mediastinum) on the F-18 FDG-PET imaging. If a lung nodule has a CT appearance that is benign but demonstrates increased metabolic activity, malignancy should be suspected. False-positive causes of FDG-PET imaging include infectious or granulomatous processes. Also, since well-differentiated adenocarcinoma with lepidic pattern and carcinoid may demonstrate no significant FDG activity, correlation with prior imaging, follow-up imaging or biopsy should be considered for lesions with low level of F-18 FDG uptake. If the nodule demonstrates characteristic popcorn-like calcifications within it, then hamartoma is likely and further workup would be unnecessary.
References: Bury T, Dowlati A, Paulus P, et al. Evaluation of the solitary pulmonary nodule by positron emission tomography imaging. Eur Respir J 1996;9(3):410-414.
Chang JM, Lee HJ, Goo JM, et al. False positive and false negative FDG-PET scans in various thoracic diseases. Korean J Radiol 2006;7(1):57-69.
9 A 63-year-old lady presents with shortness of breath. Given the following images, what is your interpretation based on the modified PIOPED II criteria?
 |
A. Very low probability
B. Low probability
C. Nondiagnostic
D. High probability
View Answer
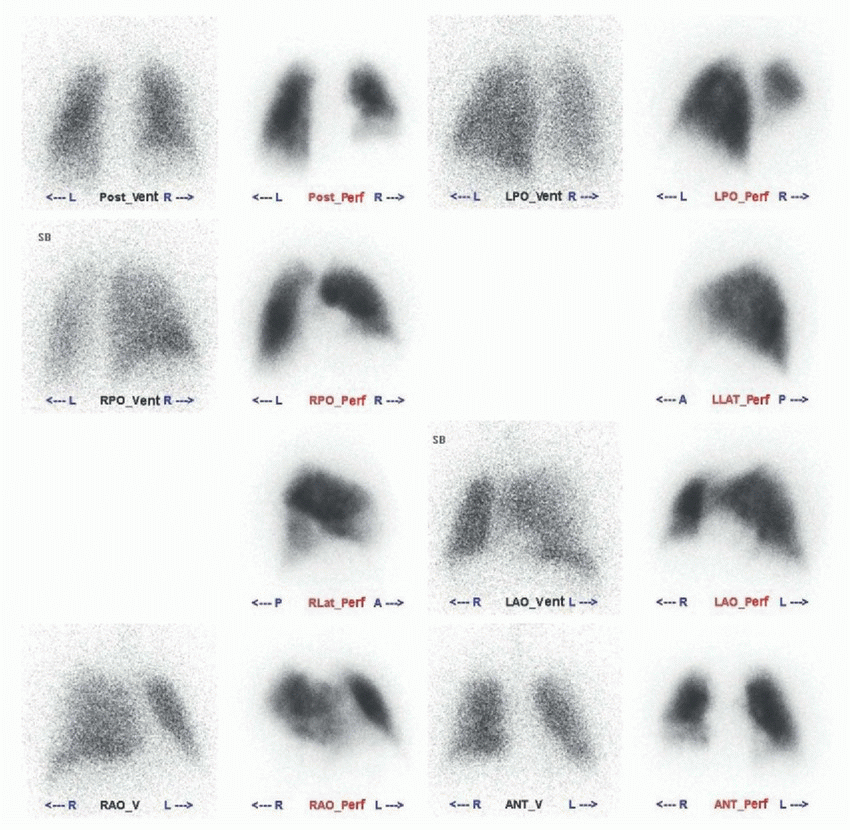
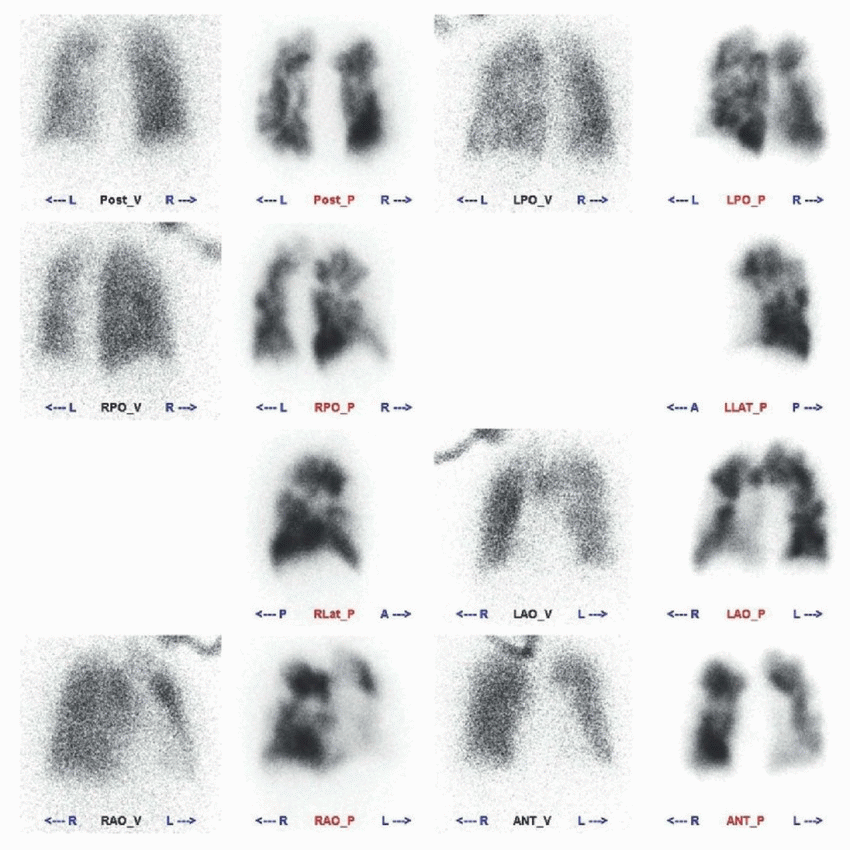
9 Answer D. There is a large multisegmental mismatched perfusion defect involving the entire right lower lobe (arrowheads in the first image below). Since there are ≥2 (superior and four basilar segments of the right lower lobe) large (>75% of the lung segment), segmental (wedge-shaped, extending to pleura), mismatched perfusion defects, the findings are compatible with a high probability (85%-90%) of pulmonary embolism. Occasionally, large defects such as this are misinterpreted when multiple adjacent segments are involved; close attention and correlation with ventilation scan should help prevent this mistake. A more typical appearance of a high probability ventilation perfusion scan is shown in the second image below, which demonstrates multiple, large, wedge-shaped, mismatched segmental perfusion defects in the right and left lungs.
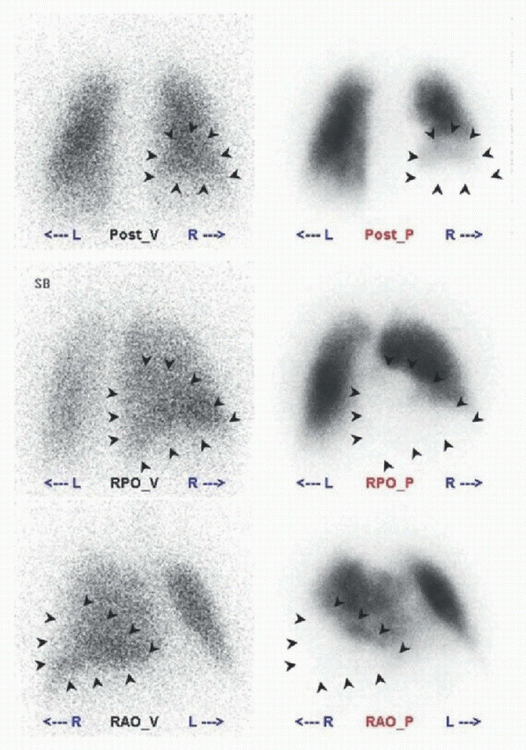 |
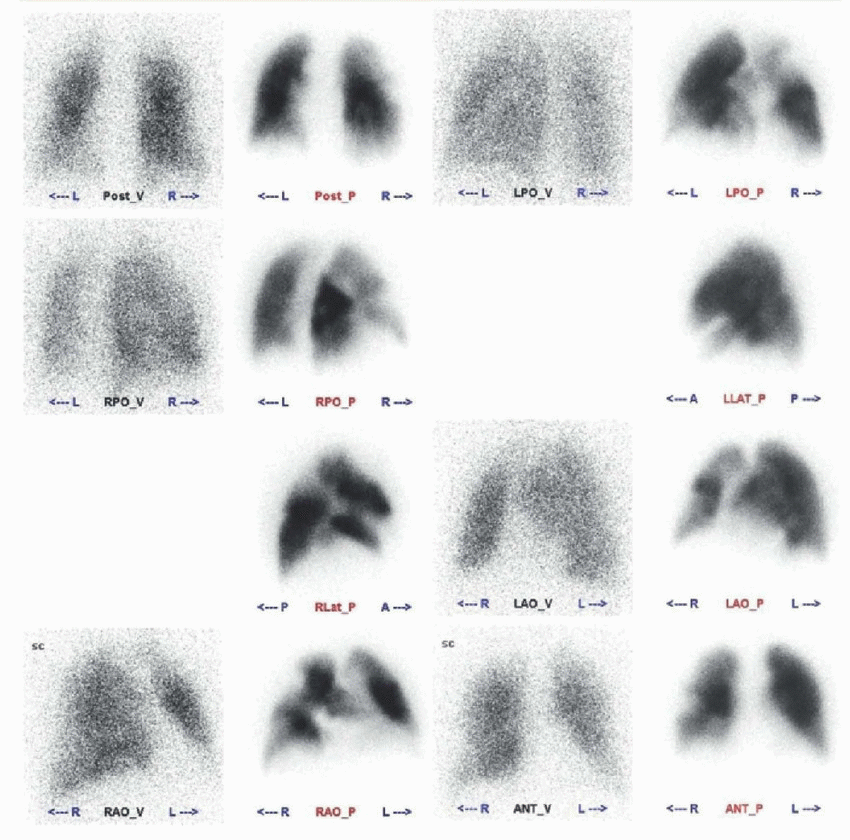 |
Modified PIOPED II Criteria* | |
High probability | ≥2 large mismatched segmental defects |
Very low probability | Nonsegmental defects Stripe sign 1-3 small segmental defects Single triple-matched defect in upper lung Perfusion defect smaller than corresponding radiograph abnormality |
Normal | Normal perfusion. No defects |
* If the perfusion does not fall into one of these categories, then it is nondiagnostic and requires further workup. | |
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:212-216.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:216-219.
10 According to the modified PIOPED II criteria, what is the probability of pulmonary embolism in this patient?
 |
A. Very low probability
B. Low probability
C. Nondiagnostic
D. High probability
View Answer
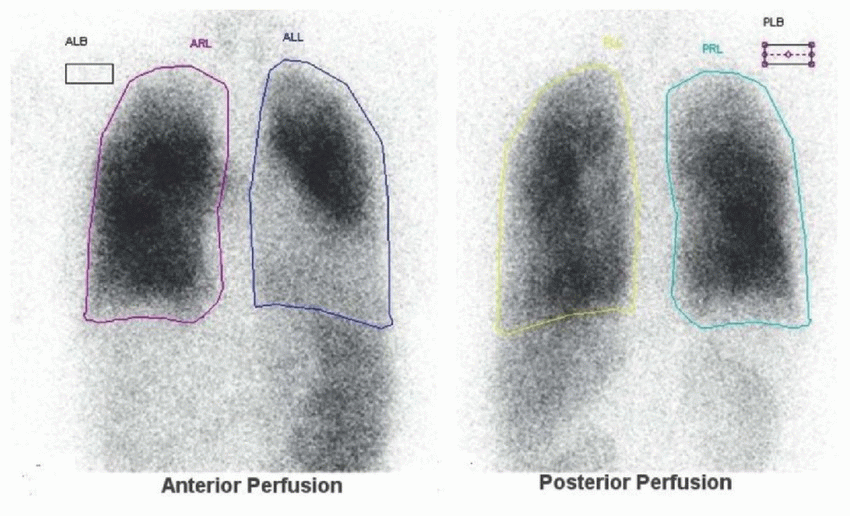
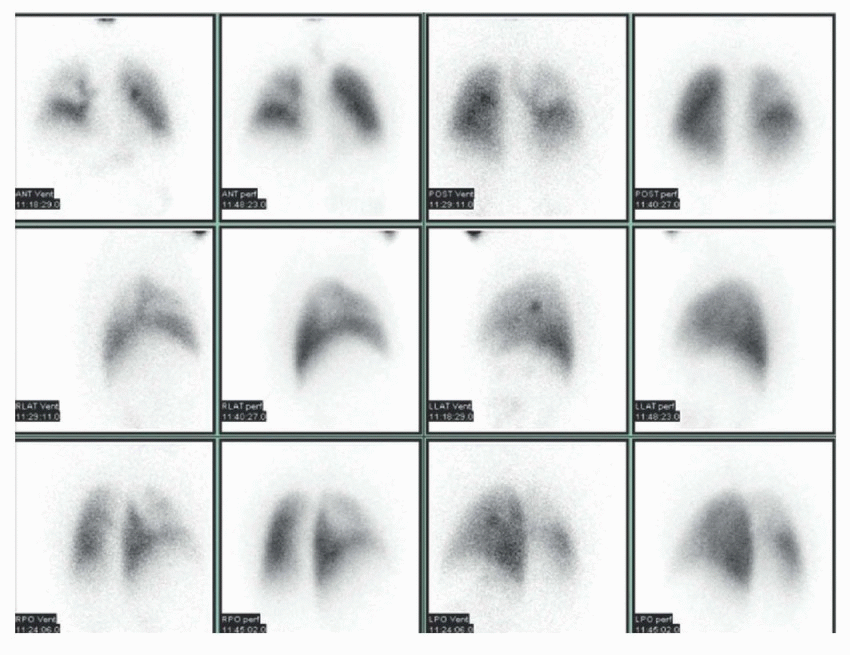
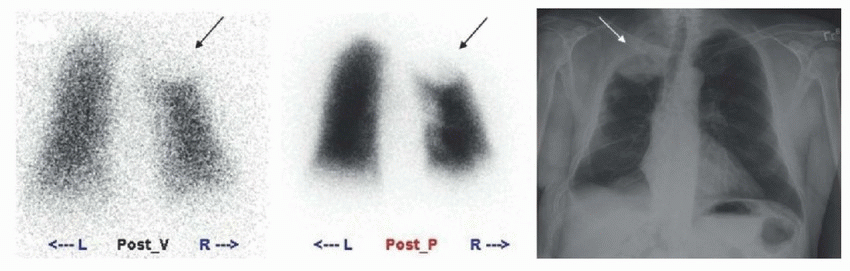
10 Answer A. The ventilation and perfusion images demonstrate presence of a large, nonsegmental, matched perfusion defect involving the right upper lobe. Perfusion is present at the periphery of this defect (arrows); this is known as the stripe sign and represents a very low probability (<10%) of pulmonary embolus. A nonsegmental perfusion defect does not correspond to bronchopulmonary anatomic segment and is generally not wedge-shaped. It may be caused by pulmonary abnormalities such as emphysema/bullae (most common), atelectasis, neoplasm, pneumonia, hemorrhage, or edema. Extra pulmonary abnormalities resulting in nonsegmental perfusion defect include normal variance or pathology of hilar or mediastinal structures and alterations in diaphragmatic contour. According to modified PIOPED II criteria, the category of very low probability includes the following: nonsegmental perfusion defect, a perfusion defect with a stripe sign, one to three small segmental defects, single triple-matched defect in the upper or middle lung zone, and a perfusion defect smaller than the corresponding chest radiograph abnormality. If a VQ scan does not fall into a high probability, a very low probability, or a normal category, then it should be assigned a nondiagnostic category requiring further workup.
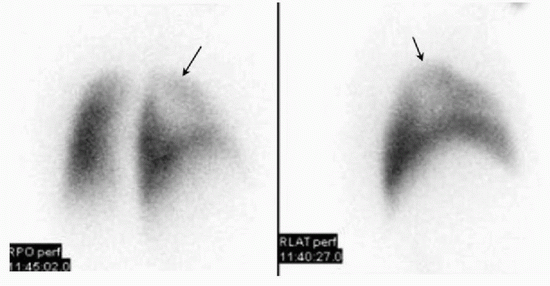 |
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:217.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:221-224.
11 Diffuse lung uptake 1 hour after the injection of Indium-111 labeled white blood cells is secondary to which of the following?
A. Pneumonia
B. Radiation pneumonitis
C. Pleural effusion
D. Physiologic
E. Chemotherapy
View Answer
11 Answer D. On early images after intravenous administration of In-111-labeled WBC scan, diffuse physiologic lung activity is visualized. However, this activity should reduce over the course of 4 hours after the injection, reducing to the background. Persistent lung uptake can be secondary to damaged WBCs during the labeling process. Pneumonia, pneumonitis, and chemotherapy can all be associated with increased pulmonary uptake of tagged WBCs, but it would be present on delayed images. Benign pleural effusion would result in no significant abnormality.
Reference: Love C, Opoku-Agyemang P, Tomas MB. Pulmonary activity on labeled leukocyte images: physiologic, pathologic, and imaging correlation. Radiographics 2002;22(6):1385-1393.
12 A 78-year-old male with past medical history of smoking presents with the complaint of shortness of breath and palpitations. The ED physician was concerned for pulmonary embolism and requested a V/Q scan. What is the most likely interpretation using the modified PIOPED II criteria?
 |
A. Very low probability
B. Low probability
C. Nondiagnostic
D. High probability
View Answer
12 Answer A. The ventilation and perfusion images demonstrate a large matched perfusion defect involving the right lung apex, which corresponds to a masslike density on the chest radiograph (arrows). Findings are consistent with a triple-matched upper lobe perfusion defect, which is considered to be a very low probability (<10%) of PE by the Modified PIOPED II criteria. In this case, the perfusion defect is secondary to the right apical lung cancer. On the other hand, a triple-matched perfusion defect within the lower lungs would be considered nondiagnostic secondary to increased prevalence of PE in the lower lobes. In this case, some would advocate an approach stating that there is no evidence of pulmonary embolus and the perfusion defect corresponds to the pulmonary malignancy.
 |
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:213.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:217-223.
13 A 44-year-old female presents with shortness of breath. You are given the following images. What is the most important thing to review prior to the interpretation of this examination?
 |
A. Chest x-ray
B. Venous Doppler
C. Prior V/Q scan
D. Prior chest CT
View Answer




13 Answer C. The perfusion images demonstrate multiple, large, bilateral, mismatched, segmental defects consistent with a high probability of pulmonary embolus. Incomplete resolution of prior pulmonary emboli is one of the most common causes of mismatched perfusion defects. As such, any prior ventilation/perfusion scan should be reviewed prior to rendering the diagnosis of an acute PE. While it is true that V/Q scans should be interpreted with a recent chest x-ray (at a minimum within past 48 hours and preferably within 24 hours), a chest x-ray is unlikely to change your interpretation in this case with normal ventilation. This patient had a prior VQ scan, which was identical in appearance making acute PE less likely. One should closely look for new mismatched defects in these patients, which would indicate new pulmonary emboli. Patients with high burden of pulmonary emboli and elderly patients are less likely to return to normal after treatment of PE. In these patients, perfusion lung imaging is preferred over CTPA to follow the course of the disease. A 3-month follow-up study should be considered to serve as a baseline for future reference since perfusion defects persisting at 3 months are less likely to resolve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree