Abstract
Pineoblastomas are rare, severe primary brain tumors originating in the pineal gland. They might be challenging to detect and cure. This article recounts the example of a 23-year-old man who suffered from regular headaches and visual issues. During the first MRI, a solid cystic tumor in the pineal area was identified, creating obstructive hydrocephalus by squeezing surrounding brain regions. A low-grade glial tumor was discovered during the operation, which included partial tumor excision and an endoscopic third ventriculostomy. However, follow up imaging revealed a rapid recurrence requiring external ventricular drainage and a second craniotomy. Following the second surgery, histopathology confirmed pineoblastoma, demonstrating the aggressive character of the tumor. Postoperative imaging showed persistent illness despite these measures, requiring the implementation of a comprehensive treatment strategy. The multidisciplinary team suggested craniospinal irradiation (35 Gy in 21 fractions) followed by lesion boost (19.8 Gy in 11 fractions), using VMAT (Volumetric modulated Arc therapy) technique, along with concurrent chemotherapy followed by adjuvant chemotherapy. This case illustrates the difficulties in identifying and managing recurrent pineal tumors, including the need for appropriate adjuvant treatment, surgical constraints, and recurrence concerns. It provides crucial information regarding the challenges of treating aggressive brain tumors and emphasizes the need for interdisciplinary care to achieve the best results. This is a rare case of Central Nervous system recurrent tumor, which was earlier thought to be a low grade pineal tumor but later turns out to be high grade, Pineoblastoma in a young adult male. The case emphasizes the challenges in correct diagnosis of CNS tumors, importance of Immunohistochemistry and prompt management for complete cure of the disease.
Introduction
A rare and extremely dangerous brain tumor, pineoblastoma develops from the pineal gland, a tiny endocrine organ in the brain that produces the hormone melatonin, essential to the body’s regular sleep-wake cycle [ ]. The World Health Organization (WHO) has classified it as a Grade IV tumor, indicating that it is high-grade and aggressive and falls under the category of primitive neuroectodermal tumors (PNETs). Pineoblastoma (PB) accounts for fewer than 0.1% of intracranial neoplasms and is more prevalent in youngsters than adults, with adult cases comprising less than 10% [ ]. Pineal tumors are generally uncommon, accounting for only 0.2% of all brain tumors and having an age-adjusted incidence rate (AAIR) of 0.05 per 100,000. Black patients and children had the highest frequency of PB, while males, small children, elderly persons, and those who did not have surgery had the lowest survival rates [ ].
Historically, pineal parenchymal tumors were categorized as either pineoblastoma, pineocytoma, or pineocytomapineoblastoma. Pineoblastomas are thought to be the most aggressive among the pineal parenchymal tumors. They have a poor prognosis and a high death rate during the first 5 years of diagnosis [ ]. Regarding histology, PBs are infiltrative, weakly differentiated, and have a distinctively primitive neuroectodermal look. Although it seldom occurs outside the central nervous system (CNS), leptomeningeal dispersion is frequent [ ]. Clinically, when PB interferes with cerebrospinal fluid (CSF) flow through the cerebral aqueduct, it can lead to hydrocephalus, a backup of CSF that raises intracranial pressure. Headaches, drowsiness, vomiting, and eye-light alterations are common patient symptoms [ ].
Additionally, depending on the size of the tumor and its local invasion, other symptoms could include visual abnormalities, Parinaud’s syndrome (a combination of eyelid retraction, convergence-retraction nystagmus, and upward gaze palsy), and unspecified neurological deficiencies [ ]. Neuroimaging is essential in diagnosing, planning, and following up patients with pineal masses. Pineoblastomas typically manifest as irregular, poorly defined, lobulated tumors that are huge (more than 3 cm) and frequently invade the nearby brain. Their high cellularity causes them to appear hyperdense on CT compared to the surrounding brain, and because they are highly malignant, they frequently have necrotic regions and hemorrhagic alterations [ ].
The standard therapeutic approach for this aggressive disease involves a multimodal approach, which includes surgery, chemotherapy (CTH), radiation (RTH), high-dose chemotherapy (HDCTH), and stem-cell rescue [ ]. The management of recurrent pineoblastoma, a rare and aggressive brain tumor, is complicated, as demonstrated by the case of a 23-year-old man. The patient’s clinical trajectory reveals several significant obstacles, diagnostic challenges, surgical restrictions and recurrence Issues. This case highlights the need for a multidisciplinary approach to address the complex issues associated with recurrent pineoblastoma involving radiologists, radiation oncologists, neurosurgeons, and neuro-oncologists. It also emphasizes the significance of continuing research into innovative therapeutic approaches and the requirement for customized patient care regimens.
Case presentation
A 23-year-old male patient reported to our institution complaining of headaches and blurring vision for a month. He reported no comorbidities and no history of family cancer. On examination, he was in good condition, with no pallor or palpable lymph nodes. He had blurred vision in both eyes, while his rest cranial nerves were normal, with normal higher functions. His Power 5/5 was in all 4 limbs. He had no sensory deficits. No cerebellar signs were found; he reported having visited another hospital early that same month with similar complaints; investigations were carried out, including a brain MRI scan that revealed a well-defined heterogeneously enhancing solid cystic lesion of approximate size 2.6 × 2.4 × 2.1 cm (AP X CC X TR), noted in midline in pineal region appearing hyperintense on T2W/FLAIR and heterogeneously hypointense on T1W with hyperintense rim, showing multiple central foci of blooming on SWI with patchy areas of diffusion restriction in solid component. The patient underwent a successful endoscopic third ventriculostomy with excision of the third ventricular tumor at our hospital, which was noted as his first surgery. The histopathology results showed no evidence of malignancy; immunohistochemistry was requested to rule out low-grade glial neoplasm. He was enrolled in a regular follow-up program at our neurosurgery department.
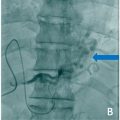
Later on, the patient did a follow up brain MRI scan that reported evidence of heterogeneously enhancing solid cystic altered signal intensity lesion noted along the midline in the pineal region and third ventricle region appearing heterogeneously hyperintense on T1W1/2W1, dirty signal on FLAIR with patchy areas of diffusion restriction of solid component and showing multiple central foci of blooming on SWI. The pineal gland is not seen separately from the lesion. Most of the cystic areas showed hemorrhage within. It measures 4.9 × 3.7 × 3.5 cm. Inferiorly, the lesion compresses the midbrain. The above features suggested a residual/recurrent neoplastic lesion, likely a pineal germ cell tumor. Some features of obstructive hydrocephalus were seen along with postoperative changes in the right frontal region ( Fig. 1 ).

The patient underwent suboccipital craniotomy with excision of pineal gland tumor (Supratentorial approach), and later, External ventricular drainage was done at our institution. Histopathology report from the sample collected reported features suggestive of pineoblastoma.
Afterwards, the patient returned for postoperative review and a plain brain MRI was done and revealed Postoperative status in the form of suboccipital craniotomy. CSF drainage tube noted in situ with a tip in the frontal horn of the left lateral ventricle. The postoperative extra-axial lesion in the retro cerebellar region in the midline extends to the suboccipital region in the intramuscular and subcutaneous plan. It measures 5 × 3.8 × 6.9 cm (AP into transverse into CC) in size. It appears hyperintense on T2 and hypointense on T1 and isointense on FLAIR with peripherally enhancing wall İll-defined lesion heterogeneously hyperintense lesion with peripheral hypointense rim on T2 and hyperintense at the superior aspect and hypointense at the inferior aspect on T1 seen at the postoperative site in the pineal region. The lesion shows peripheral blooming on SWI and no significant restricted diffusion. The lesion measures approximately 3.1 × 1.5 × 2 cm in size (AP × CCxT). The lesion is seen to abut and compress the superior tectal plate; Superiroly, it abuts the corpus callosum’s internal cerebral vein and selenium. It is seen to compress the cerebral aqueduct. Bilateral lateral ventricles appear mildly dilated. No periventricular ooze was seen. The focal abnormal signal appears hyperintense on T2 and hyperintense on T2 with the peripheral hypointense rim, and peripheral blooming on SWI is seen in the right cerebellar region. A focal area of gliosis was seen in the right frontal lobe at the site of previously placed EVD. Mucosal thickening was seen in the left maxillary sinus. The above findings were suggestive of a recurrent pineoblastoma. Fig. 2 shows postoperative T1 contrast MRI axial mages.