Abstract
Recurrence of vaginal squamous cell carcinoma (SCC) involving the rectum is extremely rare and usually results from direct spread of the primary tumor. Such cases often present with pelvic metastases and can mimic infectious or inflammatory conditions, complicating diagnosis and delaying treatment. While computed tomography scans are commonly used for diagnosis, they may be misleading. Endoscopic ultrasound (EUS) is crucial for accurately assessing rectal and perirectal lesions. We present the case of a 60-year-old female with a history of vaginal SCC who presented with refractory constipation. Initial imaging suggested a perirectal abscess, but a definitive evaluation with EUS revealed rectal wall thickening and a lesion involving the submucosa. Biopsy confirmed high-grade squamous intraepithelial neoplasia consistent with recurrent vaginal SCC. This case highlights the critical role of EUS in diagnosing recurrent pelvic malignancies with rectal involvement.
Introduction
Local recurrence of vaginal squamous cell carcinoma (SCC) occurs in approximately 23%-26% of patients within 5 years [ ]. However, recurrence involving the rectum is exceedingly rare and typically results from the direct spread of the primary vaginal tumor. Such cases are often accompanied by other metastatic lesions in the pelvis, making this a highly uncommon manifestation of vaginal cancer recurrence [ ]. When vaginal malignancies invade adjacent structures, such as the rectum, they can present with symptoms resembling infectious or inflammatory conditions. This overlap can complicate diagnosis and delay treatment due to the nonspecific nature of the symptoms [ ]. While imaging studies like CT scans are commonly the initial diagnostic step, their findings are often nonspecific or misleading [ ]. Endoscopic ultrasound (EUS), with its ability to provide high-resolution imaging and enable tissue sampling, plays a crucial role in assessing rectal and perirectal lesions [ ]. In this report, we discuss a case of recurrent vaginal SCC presenting as rectal wall involvement, initially misdiagnosed as a perirectal abscess on CT, emphasizing the critical role of EUS in achieving an accurate diagnosis.
Case presentation
A 60-year-old female with a history of hyperlipidemia and vaginal SCC presented to the emergency department with a 1-week history of constipation. Previous treatments of vaginal SCC included laparoscopic-assisted vaginal hysterectomy in 1995, radical vaginectomy in 2018, and subsequent teletherapy and brachytherapy. She described passing small, pebble-like stools with mucus and reported mild improvement with over-the-counter remedies, including enemas, suppositories, magnesium citrate, and prune juice. However, her symptoms persisted. She denied nausea, fever, chills, hematochezia, melena, or any history of inflammatory bowel disease (IBD). Her last colonoscopy 5 years prior was unremarkable.
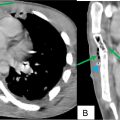
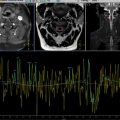
On examination, the patient was afebrile. Her blood pressure, heart rate, and respiratory rate were normal. Initial laboratory studies revealed mild anemia with a hemoglobin level of 10.9 g/dL, normal white blood cell count, liver function tests, electrolytes, and renal function. Urinalysis showed trace ketones, small leukocyte esterase, and 1+ proteinuria. A CT scan of the abdomen and pelvis demonstrated a thickened rectal wall with a probable 2.7 × 2.6 cm mural abscess and significant stool burden consistent with constipation ( Figs. 1 A and B) . The patient was started on piperacillin/tazobactam and referred to gastroenterology for endoscopic ultrasound (EUS) guided abscess drainage. Standard endoscopy revealed an 8 mm ulcer in the recto-sigmoid colon ( Fig. 2 A) . EUS demonstrated diffuse rectal wall thickening and a 24 × 16 mm left posterolateral rectal wall noncircumferential lesion predominantly in the submucosal layer, raising concern for a neoplastic process ( Fig. 2 B) . A fine-needle biopsy (FNB) of the lesion was performed, and tissue was sent for histopathological analysis.


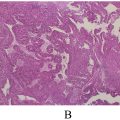
Subsequent imaging with an MRI of the pelvis confirmed a complex left-sided perirectal mass measuring 2.4 × 2 × 1.8 cm at the level of mid-rectum with infiltration into the rectum, and a separate 2.8 × 1.3 × 2.9 cm lesion along the right pelvic sidewall ( Fig. 3 ). PET imaging revealed intense radiotracer uptake in the left pelvic mass abutting the rectal wall, as well as moderate metabolic activity in a right pelvic lymph node, concerning metastatic disease. Histopathological analysis of the biopsied tissue demonstrated high-grade squamous intraepithelial neoplasia ( Figs. 4 A and B ) with positive P16 and Ki-67 markers, consistent with a recurrent malignant process ( Figs. 5 A and B) . These findings collectively suggested recurrent vaginal SCC with rectal wall invasion and possible metastatic spread. The patient is following up with general surgery and gynecology for further treatment of recurrent vaginal SCC into the rectum.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree