Retrieval of Intravascular Foreign Bodies
Aneeta Parthipun
Tarun Sabharwal
The majority of intravascular foreign bodies (FBs) are the result of iatrogenic complications. First-line treatment is percutaneous radiologic extraction. Since its first description 50 years ago, there has been increased application of these techniques correlating with the expansion of endovascular procedures generally (1). Early reports on FB retrieval techniques focused on broken catheters, guidewires, and vena cava filters. The spectrum of endoluminal foreign bodies requiring removal has broadened and now includes embolization coils, ruptured angioplasty balloons, and endovascular stents.
Endovascular retrieval of FBs is generally an effective, safe technique, which avoids the need for major surgery. Given the disparate group of potential FBs, retrieval strategies depend on the device and its position within the vasculature. In the majority of cases, it is essential to retrieve the FB to prevent potentially life-threatening complications including sepsis, thrombosis, clot embolism, arrhythmias, and vascular perforation (2).
Indications
1. Misplaced or fractured guidewire, catheter, pacemaker wire, and broken endovascular device fragments
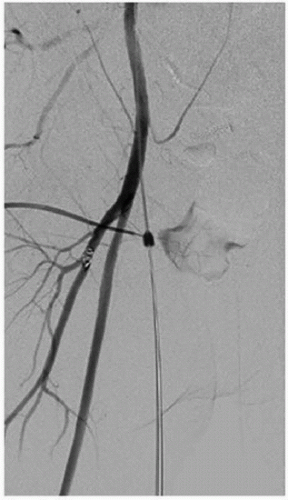
2. Misplaced embolization coils (Fig. e-82.1)
3. Malpositioned arterial and venous stents
4. Inferior vena cava (IVC) filters including both routine and complicated removal particularly when the filter tip is angled against the IVC wall, is discussed further elsewhere in the book.
Contraindications
Absolute
1. Uncorrectable bleeding diathesis
Relative
Each individual case must be considered in regard to the benefits of the procedure in light of the risks associated with endovascular retrieval, if in fact removal is necessary. The risk of surgical removal must also be considered.
1. Extensive thrombus attached to the FB that will embolize on removal
2. Firmly embedded or adherent FB that might result in vessel wall perforation. A sturdy tug on the catheter fragment after snaring may result in a life-threatening or hazardous vasculature tear. In such cases, surgery as a primary treatment option may be more appropriate.
3. When structural damage to the heart or vascular system might result. Surgery may be required in patients with FBs in high-risk sites.
Preprocedure Preparation
1. Review of all imaging, preferably in a multidisciplinary setting, to identify (a) the precise location of the FB and (b) the vascular access most suitable for retrieval. Multiplanar reconstructed computed tomography (CT) is a valuable tool for planning.
2. For intracardiac FB, assess the presence of tamponade, valve involvement, and arrhythmias.
3. Check to ensure the appropriate equipment is available (Fig. e-82.2). In certain cases, more than one retrieval system or technique may be necessary to achieve successful removal (3).
4. Laboratory evaluation including complete blood count (CBC), clotting parameters, and renal function. The international normalized ratio (INR) should be corrected to <1.5 seconds, and the platelet count corrected to >75,000 per µL.
a. Ensure anticoagulants have been stopped, if appropriate. If the patient is at moderate risk of bleeding, clopidogrel should be withheld for 5 days prior to the intervention. If the patient is at high risk of bleeding, then both clopidogrel and aspirin should be withheld for 5 days.
5. Patients should be on nil per os (NPO) 6 to 8 hours prior to the procedure. No clear liquids should be consumed for 3 to 4 hours prior to the procedure.
6. Start intravenous fluids (150 mL per hour) to ensure adequate hydration of the patient. Monitor fluid status. Renal dialysis patients may need coordination of dialysis. However, it is important to note that these cases often require only small volumes of contrast.
7. Informed written consent
Procedure
1. General considerations
a. Appropriate vascular access is chosen to facilitate FB removal, commonly single access or a combination of the common femoral artery or vein and the jugular vein. An appropriately sized sheath should be inserted to allow for easy removal and avoid trauma at the exit site. A “buddy wire” or parallel wire introduced outside the sheath may be beneficial to maintain vascular access when FB removal requires sheath removal.
b. Intraprocedural anticoagulation. An intra-arterial or intravenous dose of 5,000 IU heparin is injected at the beginning of the procedure. Thereafter, further doses of heparin may be required to maintain an activated clotting time (ACT) of greater than 250 seconds.
c. Anesthesia. FB retrieval can often be performed under local anesthesia; however, as part of the planning stage of the procedure and following consideration of the complexity of the individual case along with the patients’ clinical status, sedation or general anesthesia may be required.
2. Specific scenarios
a. FB with free end
(1) Manufactured loop snare. The most popular snare device is a single-loop snare such as Amplatz GooseNeck Snare (ev3, Plymouth, MN) or the ONE Snare (Merit Medical Systems, South Jordan, UT) (Fig. e-82.2A) manufactured in a range of sizes (diameters from 5 to 35 mm). There are also microsnares (diameters from 2 to 7 mm). The chosen diameter should correspond to the target vessel diameter. The snare is deployed through a guide catheter (which has a radiopaque marker). To use the snare:
(a) Place a guidewire next to the FB. This is an essential beginning point. If this is not achieved, the retrieval of the FB will not be possible.
(b) Advance the guide catheter over the guidewire and then remove the guidewire.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree