This article brings to light the importance of MR imaging not only as a tool for the diagnosis of spine and spinal cord infections but also for identifying potential complications that can increase morbidity and mortality. The authors explore the typical imaging characteristics of common and infrequent spine infections and discuss their relevant pathophysiology and clinical features. Infections are categorized by the affected anatomic structure and by the pathogenic microorganisms, such as bacteria, fungi, parasites, and viruses. It also highlights the role of MR imaging in detecting complications such as epidural abscess, and distinguishing these pathologies from other spinal conditions.
Key points
- •
Inflammatory and infectious spine diseases are clinically significant and may impact quality of life due to potential complications.
- •
Spinal infections often present with nonspecific symptoms, requiring clinical, laboratory, and imaging correlation for early diagnosis.
- •
Involvement of different spinal structures can result in vertebral osteomyelitis, discitis, epidural abscesses, or myelitis.
| CARD9 | caspase-associated recruitment domain-9 |
| CMV | cytomegalovirus |
| CNS | central nervous system |
| CSF | cerebrospinal fluid |
| CT | computed tomography |
| DWI | Diffusion-weighted imaging |
| ESR | erythrocyte sedimentation rate |
| GBS | Guillain-Barré syndrome |
| H&E | hematoxylin–eosin stain |
| HIV | human immunodeficiency virus |
| HSV | herpes simplex virus |
| HTLV-1 | human T-lymphotropic virus type 1 |
| IV | intravenous |
| NCC | neurocysticercosis |
| PCR | polymerase chain reaction |
| T1W | T1-weighted |
| T2W | T2-weighted |
Introduction
Inflammatory and infectious spine involvement is of concern in clinical practice due to the potential complications and impact on patient’s quality of life. The spine is affected in 7% of musculoskeletal infections. These conditions frequently have nonspecific clinical manifestations that may resemble those of other diseases. Early diagnosis and therapeutic approach rely on a combination of clinical signs and symptoms, laboratory tests, and imaging findings.
Infections can involve different structures, including the intervertebral discs, the vertebral bodies, the paravertebral spaces, and the cord, resulting in vertebral osteomyelitis, discitis, epidural abscesses, and myelitis. , Bacterial infections are the most common cause of spinal infections. However, parasitic infections have a significant epidemiologic presence in countries with inadequate sanitary conditions.
Despite a significantly decreased incidence of parasitic diseases in recent years, cysticercosis remains the most prevalent in countries like Brazil, while toxoplasmosis is the most common central nervous system (CNS) condition in immunosuppressed patients. In the spine, however, this occurrence is rare. Trypanosomiasis and echinococcosis are less frequent as well. ,
In recent decades, the prevalence of spinal infections has significantly increased, mainly due to an aging population, the rise of invasive medical procedures, and the increasing prevalence of immunosuppressive conditions such as diabetes mellitus, chronic corticosteroid use, chronic renal failure, and abuse of intravenous (IV)-administered substances. Additional predisposing factors include hematogenous dissemination of systemic infections, such as urinary or respiratory tracts infections, and prior spinal surgical procedures. ,
Axial skeletal infections
Vertebral infection affects more commonly the anterior endplate due to its rich blood supply. Subsequently, it may spread to the psoas muscles in the lumbar region, to the surrounding paraspinal soft tissues and to the epidural space. Infection of the disc-endplate is termed spondylodiscitis; septic arthritis refers to an infection of the facet joint; and epidural abscess describes infectious fluid collections within the epidural space. , ,
Infections may develop as a result of hematogenous seeding, direct introduction, or extension from a contiguous focus of infection. In hematogenous spread, infected microemboli get stuck in narrow segments of vertebral metaphyseal arteries, while direct or contiguous dissemination refers to the spread of infection from nearby infected tissues, usually after surgery or a trauma. The Batson venous plexus, a network of veins located around the spine, allows blood to flow upward and downward, thus helping viruses arrive in the spine from other body regions. The anatomic compartments that can be affected by infectious processes are illustrated in Fig. 1 .

As in other fields of radiology, the use of standardized nomenclature is essential for an accurate interpretation of findings, minimizing the risks of misinterpretation. The main descriptors related to spine infection are detailed in Table 1 .
| Descriptor | Medical Condition | Additional Information |
|---|---|---|
| Spondylodiscitis | Disc infection with adjacent vertebral body osteomyelitis | Most common form of spinal infections at diagnosis |
| Discitis | Isolated disc infection | Occurs mostly in children that have more vascularized intervertebral discs |
| Facet joint septic arthritis | Hematogenous pyogenic infection within facet joints | Historically rare but increasingly diagnosed |
| Spondylitis | Vertebral endplate infection | Very early osteomyelitis in adults |
| Secondary epidural abscess | Contiguous spread of infection into the vertebral canal | Ventral epidural space: usually secondary to discitis Dorsal epidural space: usually secondary to septic facet joint |
| Primary epidural abscess | Isolated epidural abscess with no signs of infectious disease in other structures | Extremely rare in the MR imaging era |
Spondylodiscitis
Pyogenic spondylodiscitis
Staphylococcus aureus is the most frequent pathogen in pyogenic spondylodiscitis, accounting for about 60% of all cases. Other agents include Streptococcus viridans (usually in IV drug users and immunocompromised patients) and some gram-negative bacteria like Enterobacter species and Escherichia coli .
Although pyogenic spondylodiscitis can occur anywhere in the spine, it most often affects the lumbar region. In about 65% of patients, a single vertebral segment is involved; contiguous segments are seen in 20% of patients; and noncontiguous infections are responsible for 10% of cases. , , ,
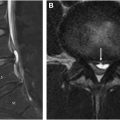
MR imaging findings include erosion of the endplates of adjacent vertebral bodies, hypointensity of the bone marrow on T1-weighted (T1W) images, and higher than usual T2-weighted (T2W) hyperintensity in the intervertebral disc. Additionally, gadolinium enhancement is observed in both the disc and the adjacent vertebral body. Associated fluid collections are characterized by peripheral gadolinium enhancement, with variable signal intensity of their contents. Diffusion-weighted imaging (DWI) plays an important role in differentiating purulent collections from other fluid collections, such as seromas related to surgery. Collections with purulent content tend to show lower signal intensity on T2W images compared to collections with less proteinaceous material. These collections can extend to the paraspinal spaces and to the anterior epidural space , , , ( Fig. 2 ).

Epidural space anatomy offers little resistance to the longitudinal spread of infection. Anterior epidural abscesses are a complication of spondylodiscitis or vertebral osteomyelitis, seen in 20% of cases due to contiguous spread. Direct inoculation occurs in about 15% of cases, as a result of neurosurgical interventions, lumbar puncture, epidural analgesia, and other invasive procedures. Additionally, approximately 20% of cases are idiopathic, with no identifiable cause. Pyogenic epidural collections can cause various local and systemic complications, such as resistance to antimicrobial treatment, dissemination of the infectious process to the spinal cord and subdural space, spinal and radicular compression, spinal ischemia, or even septicemia and shock. ,
Tuberculous spondylodiscitis
Tuberculous spondylodiscitis, also referred to as Pott’s disease, is a result of infection by Mycobacterium tuberculosis . Although infrequent even in emerging countries, this condition is still epidemiologically relevant. There are imaging features that may help differentiate it from pyogenic spondylodiscitis. , ,
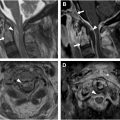
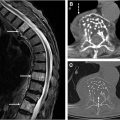
Radiological findings for tuberculous spondylitis include abnormal signal intensity of the paraspinal soft tissues, thin-walled abscesses, and inflammatory tissue underneath spinal ligaments spanning over 3 or more vertebral segments. In comparison to other forms of spondylitis, this extensive involvement often includes several vertebral bodies or even the entire vertebral column ( Fig. 3 ).

“Cold” abscesses in the paraspinal region are frequent manifestations of tuberculous spondylitis. These occur without redness, swelling, or severe pain typically observed in acute inflammation caused by pyogenic (bacterial) infections. MR imaging signs that suggest cold abscesses include well-defined margins, rim gadolinium enhancement, and subligamentous spread spanning multiple segments. Cold abscesses caused by spinal tuberculosis do not usually entrap intercostal arteries as those caused by common bacteria. ,
Unlike pyogenic bacteria, M tuberculosis does not produce proteolytic enzymes. For that reason, infections tend not to severely damage the intervertebral disc, resulting in subligamentous dissemination. Radiographs and computed tomographic (CT) scans are more sensitive than MR imaging for the detection of paraspinal calcifications, a near pathognomonic feature in spinal tuberculosis. However, the combined MR imaging findings of multisegmental extension, characteristic abscess formation, and spreading underneath the anterior longitudinal ligament can be very useful in diagnosing this condition ( Fig. 4 ).

Candida spondylodiscitis
Fungi are typically restricted to the host’s gastrointestinal, urinary, and vaginal tracts prior to the development of clinical infection. Signs of infectious disease appear as a result of disruption of the mucosal barriers, especially in immunosuppressed patients. Some risk factors include central venous catheterization, antibiotic use, dialysis, total parenteral nutrition, severe burns, surgery, and IV drug use. Candida albicans is the most common species; however, albicans and nonalbicans candidiasis have similar treatment and prognosis. , In the spine, candidiasis presents primarily as spondylodiscitis; however, it can also present as myelitis. The next section of this article focuses on fungal myelitis, with emphasis on Candida myelitis. , ,
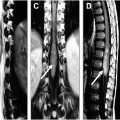
Diagnosis often occurs 2 to 6 months after symptom onset; and the typical clinical scenario includes history of immunosuppression and low back pain. MR imaging usually shows involvement of 2 or more vertebral bodies, with signal loss along the endplates on T2W images suggestive of iron deposition or presence of fungi. Ill-defined postgadolinium enhancement may be present within the paravertebral muscles, usually associated with small abscesses. Fungal paravertebral involvement is usually associated with less intense gadolinium enhancement, when compared to pyogenic and tuberculous infections ( Fig. 5 ). Most cases of Candida infection occur in the lumbar spine. ,

Aspergillus spondylodiscitis
Aspergillus is commonly contracted via inhalation of airborne spores. Spread to the spine can be either hematogenous or transpleural. , Aspergillosis is more likely to involve the lower cervical spine or the cervicothoracic junction than candida osteomyelitis.
On imaging, there is irregularity of the vertebral body endplates and involvement of the intervertebral discs, without any signs of bone destruction. MR imaging shows linear areas of T2 hypointensity in the subchondral region of the vertebral body. Subligamentous dissemination usually occurs along the anterior aspect of the vertebral bodies, while the vertebrae remain intact, similar to tuberculous spondylodiscitis. It can be easier to tell the difference between tuberculosis and aspergillosis infection if abscesses spread to the paravertebral soft tissues or epidural space, as Aspergillus abscesses have a thick, irregular wall, whereas tuberculous abscesses have a smooth thin wall ( Fig. 6 ). ,

Posterior epidural abscess
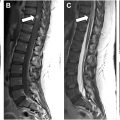
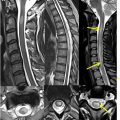
Purulent collections in the posterior epidural space arise from contiguous spread of infection from the facet joints in patients with septic arthritis ( Fig. 7 ). S aureus is the most common pathogen, encountered in about 70% of cases, including methicillin resistant strains; however, other microorganisms such as Staphylococcus epidermidis , E coli , Pseudomonas aeruginosa (especially among IV drug users), anaerobes, mycobacteria, and parasites could be found. , ,

Epidural abscess, joint effusion, periarticular bone marrow edema, and periarticular soft tissue edema with enhancement are key imaging findings that help make the diagnosis on MR imaging.
Infectious Myelitis
It should be noted that viral agents such as herpes viruses and Varicella-zoster virus are the main cause of infectious myelitis, commonly associated with radiculitis. Acute flaccid myelitis is seen in a significant number of patients that have enteroviral infections caused by poliovirus and enteroviruses A71 and D68. Additionally, human immunodeficiency virus (HIV) or human T-lymphotropic virus type 1 (HTLV-1) can lead to certain types of chronic myelitis. Infections involving the spinal cord may also have a bacterial, fungal, or parasitic origin.
Viral myelitis
There are a myriad of clinical manifestations of viral infection of the spinal cord and nerve roots. Symptoms might occur as a result of direct viral invasion or due to the associated immune response, and include paraplegia, quadriplegia, sensory impairment, gait disturbance, bowel, or bladder dysfunction. The most common viruses that can cause myelitis are herpes simplex virus (HSV), varicella-zoster virus, enteroviruses, and cytomegaloviruses. There are well-defined syndromes that are associated with specific viral agents. ,
Lumbosacral radiculitis is commonly a result of HSV infections. This type of infection usually manifests as acute urinary retention and lower limb weakness, which are major signs for Elsberg’s syndrome, an uncommon form of viral myelitis. ,
Guillain-Barré syndrome (GBS) is a condition in which the host’s immune system damages the peripheral nervous system. It can manifest as acute inflammatory demyelinating polyradiculoneuropathy. GBS has been associated with cytomegalovirus and Epstein-Barr virus infections. Motor weakness in GBS develops rapidly and symmetrically, starting in the lower extremities and evolving upwards to compromise cranial nerves, upper limbs, and autonomic system. In GBS, the ventral and dorsal nerve roots may be affected, in particular, in the region of the conus and cauda equina; however, thickening and enhancement of the ventral nerve roots are more common on MR imaging ( Fig. 8 ).