Abstract
Mycotic pseudoaneurysms are rare vascular abnormalities caused by infections, often leading to high rates of morbidity and mortality. Mycotic pseudoaneurysms are most commonly present in the aorta and femoral arteries, but a small number are observed in the common iliac artery. Here, we report the unusual instance of a Salmonella -induced mycotic pseudoaneurysm in the right common iliac artery of a 73-year-old male. Traditional imaging modalities supplemented with novel postprocessing techniques like 3D cinematic rendering enabled more confidence in differentiating between true aneurysms and pseudoaneurysms while providing a better anatomical view for preoperative planning. This case underscores the rarity of Salmonella -induced mycotic pseudoaneurysms and emphasizes the importance of early diagnosis using advanced imaging (CT, CTA with 3D cinematic rendering) and a multidisciplinary approach to treatment, which includes both infection management and surgical repair.
Introduction
Pseudoaneurysms are vascular abnormalities mostly found at the site of arterial trauma or infection. Compared to typical aneurysms, which are characterized by weak vessel walls that produce blood-filled outpouchings, pseudoaneurysms are the direct result of blood leaking outside of the vessel. This leakage is locally contained by the surrounding tissue and subsequent clotting mechanisms, forming a balloon shape covered by a false wall, that resembles a true aneurysm. The formation of a false wall is much weaker than the true wall that surrounds typical aneurysms, presenting concern for hemorrhaging in pseudoaneurysms. The most common sites of pseudoaneurysms include cardiac, visceral, aortic, and femoral arteries. Endovascular procedures are high-risk factors for pseudoaneurysms and are the most common cause of femoral pseudoaneurysms . Mycotic pseudoaneurysms are the product of vascular infection and are most common in the femoral and aortic arteries. Here, we present the rare case of mycotic pseudoaneurysm of the right common iliac artery caused by Salmonella bacteremia.
Case presentation
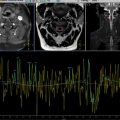
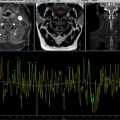
A 73-year-old male with a relevant past medical history of hypertension, hyperlipidemia, mitral stenosis, cardiomyopathy, coronary artery disease, and a coronary artery bypass procedure presented to an outside emergency department with chief complaints of abdominal pain with persistent fever and chills. Computed tomography (CT) of the abdomen ruled out appendicitis but revealed mild induration of fat adjacent to the right common iliac artery (CIA) compatible with aneurysm and possible vasculitis. The vascular team was consulted, and he was recommended for Prednisone and outpatient follow-up. Blood cultures grew Salmonella, and he was started on ceftriaxone and ciprofloxacin and was subsequently discharged. However, 2 days later, he presented again with right groin pain radiating to his flank area. Repeat blood cultures once again grew Salmonella , and a computed tomography angiography (CTA) redemonstrated the right common iliac artery pseudoaneurysm with a diameter of 1.6 cm and extending 3 cm with moderate perivascular stranding concerning for a mycotic aneurysm. At this point, he was transferred to our hospital for further management. A CTA ( Fig. 1 A-G) upon admission revealed the same previous findings but also noted the aneurysm abuts an L5 osteophyte, so magnetic resonance imaging (MRI) was obtained to rule out osteomyelitis – no evidence of osteomyelitis was seen. Infectious disease was consulted, and it was recommended that the patient switch to ampicillin. He was intermittently febrile, but repeat blood cultures remained unchanged. The CTA with 3D postprocess mapping was utilized for preoperative planning and revealed interval enlargement of the outpouching, now measuring 9 mm, suspicious for pseudoaneurysm. Focal outpouching with surrounding soft tissue thickening was demonstrated nicely by 3D mapping. He later underwent a midline laparotomy for iliac artery aneurysm excision and repair using a left central femoral vein interposition graft. During the procedure, dense retroperitoneal inflammation adherent to the aneurysm was noted. Upon dissection of the mycotic aneurysm, the internal fluid and thrombus were cultured. The operative cultures grew Salmonella again.

After surgery, he began a 6-week course of ampicillin. During the treatment process, he was trialed on Bactrim and then Augmentin but was ultimately put back on ampicillin due to nausea and vomiting with oral antibiotics. Recent blood test reported that his erythrocyte sedimentation rate (ESR) was 20, compatible with ongoing resolution of infection. He was recorded feeling well, and it was recommended he finish the 6-week ampicillin course.
Discussion
In this case, we report the extremely rare presentation of mycotic pseudoaneurysm of the common iliac artery caused by Salmonella bacteremia. To our knowledge, this is the first literature report of Salmonella mycotic pseudoaneurysm specific to the iliac artery. Primary infections of the peripheral arterial systems are rare and can be caused by an array of bacterial and fungal organisms, resulting in both true and false aneurysms . In addition, a study performed by Sarkadi et al. evaluated risk factors for the development of pseudoaneurysm and demonstrated that pseudoaneurysms were the second most common complication of procedures requiring arterial puncture with a prevalence of 0.05%-6%. The exact rate of incidence for isolated pseudoaneurysms of the common iliac artery is not well defined (<0.1%) and is less common than femoral or aortic pseudoaneurysms that have an incidence of less than 1% , ]. The incidence of arterial infection by Salmonella is also not well defined by the literature, but it’s accountable for fewer arterial mycotic pseudoaneurysms than other organisms such as Staphylococcus, Pseudomonas aeruginosa, and Streptococcus , , .
Common symptoms of pseudoaneurysm are due to swelling and often present as pain or sometimes even nerve compression. Complications of pseudoaneurysms include rupture, distal embolization, neuropathy, and local skin ischemia , . It is important to correctly identify possible risk factors that increase the likelihood of vascular infection, such as IV drug use, endocarditis, skin and soft tissue infections, vascular grafts, diabetes mellitus, and other endovascular procedures . Any delay in diagnosis and treatment can significantly impact morbidity and mortality , .
Radiological imaging modalities are essential for visualizing and diagnosing both aneurysms and pseudoaneurysms. Timely and accurate diagnosis is necessary for the treatment of potentially unstable pseudoaneurysms. Modern imaging modalities such as CT, CTA, MRI, and 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT can detect true and false aneurysms clinically in suspicious cases. Novel imaging techniques, such as 3D cinematic rendering (CR), which is a CT postprocessing technique, display timely photorealistic images of proximal anatomical structures and are particularly useful in the emergency setting . Pseudoaneurysms appear as focal outpouchings, encased by the outermost layer of the arterial wall, oftentimes with an apparent fat stranding and thick enhancement of irregular arterial walls , . Due to the life-threatening nature of pseudoaneurysms and nonspecific symptoms that challenge diagnostic ability, imaging surveillance is crucial for diagnostic capability and treatment efficacy , .
Treatment of mycotic pseudoaneurysms has been a largely controversial topic between infectious disease and vascular surgeons for a long time. Multiple approaches exist to treat pseudoaneurysms including, open surgery, image-guided endovascular repair, or less often, direct percutaneous trans gluteal puncture . Conventional open surgery generally involves aneurysm resection, clearing of the infected foci, and graft interposition. However, open surgery has extremely high rates of perioperative mortality (11%-21%), amputation (9%-11%), and reinfection (3%) . Endovascular graft therapy methods have shown promise but still present a variety of potential problems, primarily including the lack of debridement of infected tissue, leading to infection of the stent graft [ ].
In addition to the necessary anatomical fixes, the root cause of infection must also be addressed. The complexity of solving both of these issues simultaneously contributes to the high rates of morbidity and mortality among patients . Tissue cultures obtained by surgery, blood and urine tests, should all direct the management plan of infection. In our case of Salmonella bacteremia, Bactrim and then Augmentin were trialed, but was switched for ampicillin following bouts of nausea and vomiting.
Conclusion
This case highlights the rare occurrence of a mycotic pseudoaneurysm of the right common iliac artery caused by Salmonella bacteremia. It underscores the importance of timely recognition and diagnosis of pseudoaneurysms, particularly when infectious etiology is suspected. While Salmonella -induced mycotic pseudoaneurysms in the iliac artery are exceptionally rare, this case demonstrates the need for a thorough diagnostic workup using advanced imaging techniques such as CT and MRI to guide management. Treatment, which involves both addressing the infection with appropriate antibiotics and the surgical or endoluminal repair of the pseudoaneurysm, remains complex and requires careful consideration of case-specific information. Here, we also emphasize the significance of close monitoring, as delays in diagnosis and intervention can lead to severe and deadly complications.
Patient consent
The patient reported in the manuscript signed the informed consent/authorization for participation in research, which includes the permission to use data collected in future research projects such as the presented case details and images used in this manuscript.
Acknowledgments: There was no funding associated with this report.
Competing Interests: The authors have declared that no competing interests exist.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree