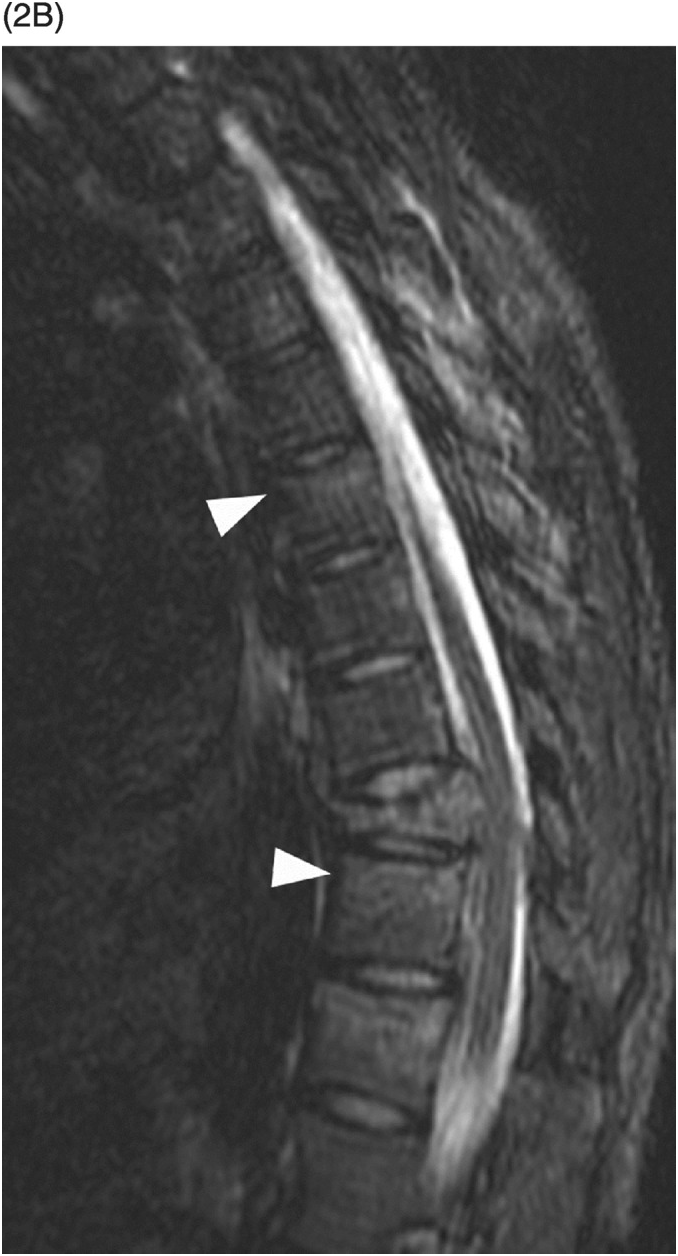
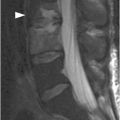
B) Corresponding STIR MR image reveals bone marrow edema of T11 and L2 vertebral bodies (arrowheads), consistent with bone contusions (microfractures). There is indeterminate disruption of the posterior ligamentous complex (PLC, arrow) and severe spinal canal stenosis with compression of the lower thoracic spinal cord/conus medullaris, which has abnormal signal consistent with hemorrhagic and nonhemorrhagic cord injury. TLICS imaging score 2 + 2 + 2 (or 3 for cord injury) = 6 (or 7), directed to surgical management.
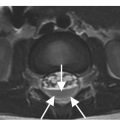
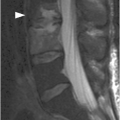
A) Sagittal CT image demonstrates T10 burst fracture (arrow) with significant height loss, wedging (resulting in mild kyphotic deformity), and displacement of the posterior vertebral body into the spinal canal. There is a more subtle compression fracture inlvoing the superior endplate of T12 (arrowhead) without significant retropulsion.
B) Corresponding MR STIR image confirms the CT findings. Additional vertebral body bone contusions (arrowheads) are noted, but no evidence for PLC injury. Although there is mild canal stenosis at T10 level, there is no frank spinal cord compression or abnormal intramedullary signal. TLICS imaging score 2 + 0 = 2, nonsurgical treatment as the patient was neurologically intact.
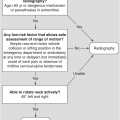
The thoracolumbar injury classification system (TLICS) identifies three major injury characteristics to describe thoracolumbar spine injuries: (1) injury morphology; (2) posterior ligamentous complex (PLC) integrity; and (3) neurological status. Within each category, there are subgroups with a numeric value assigned to each injury pattern, which are then totaled to provide a comprehensive score.
In addition, minor injury characteristics such as injury level, confounding variables (such as ankylosing spondylitis), multiple injuries, and chest wall injuries are also identified. Each major characteristic is assigned a numerical score, weighted by severity of injury, which is then summated to yield the injury severity score.
Imaging Findings
Two of the three major categories are assessed on the imaging studies: injury morphology, and PLC integrity.
Imaging Morphology: Compression injuries result from axial loading and are the most common. TLICS assigns one point for a compression fracture with visible loss of height or disruption of the vertebral endplate. An additional point is assigned if there is involvement of the posterior vertebral body with retropulsion (burst fracture). Translational/rotational injuries are the second subcategory. Rotation of the spinous processes, unilateral or bilateral facet fracture-dislocation, and vertebral subluxation can be seen. Because torsional and/or shear forces cause significant ligamentous and/or osseous damage and instability, TLICS assigns three points to this morphology. The third subcategory is related to distraction injuries and is assigned four points, identified as dissociation through the anterior/posterior ligaments and/or osseous elements.
Posterior Ligamentous Complex (PLC): The PLC can be evaluated using radiographs, CT, or MRI. On radiographs or CT, the PLC is considered disrupted if there is splaying of the spinous processes, avulsion fracture of the superior/inferior aspects of contiguous spinous processes, widening of the facet joints, naked facets, perched/dislocated facets, or vertebral body translation/rotation. MRI with fluid-sensitive sequences (STIR and fat-saturated T2w) allows for direct PLC visualization. The signs of injury are disruption of the normally dark T1/T2 stripe on sagittal images, fluid within facet capsules, or interspinous edema. Disruption of the ligamentous dark band on T1-weighted images is the most reliable and specific. If the PLC is intact, the TLICS assigns zero points. Indeterminate disruption is given two points and complete disruption is assigned three points.
Clinical Findings, Implications, and Treatment
Neurologic Status: There are five categories of neurologic injury: intact (zero points), nerve root injury (two points), complete spinal cord injury (two points), incomplete spinal cord injury (three points), and cauda equina syndrome (three points). Although evaluation requires thorough neurological examination, MR imaging can help identify the presence of nerve root and spinal cord injury.
The total TLICS score is calculated by adding the assigned points in the three categories. Patients with 0–3 points are considered nonoperative candidates. Patients with ≥5 points are directed to surgical management. Patients with a total score of 4 are considered indeterminate, and treatment may be surgical and/or nonsurgical, depending on clinical and functional status, including comorbidities and other traumatic injuries.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree