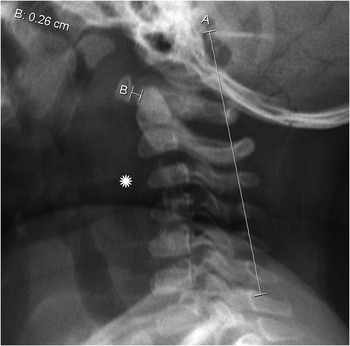
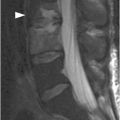
Figure 46.1 Lateral view radiograph in an 18-month-old girl shows oval to slightly triangular shape of the cervical vertebral bodies and buckling of the prevertebral soft tissues (*) due to neck flexion. There is pseudosubluxation of C2 – the spinolaminar line is drawn, and posterior arch of the C2 falls on the line. Normal atlanto-dental measurement of 2.6 mm (under 5 mm).
Imaging Findings
The craniovertebral junction ossification centers should be understood in order to prevent their misinterpretation as fractures. A normal physis can be identified by the presence of its smooth borders with subchondral sclerotic lines. C1: Anterior arch fuses at 7 years while the neural arches fuse posteriorly at approximately 3 years. C2: Ossification center at the odontoid apex, the os terminalis or os odointoideum, normally fuses by 12 years. The body of C2 fuses with the odontoid by 3–6 years. This fusion line is called the subdental synchondrosis and can be seen up until 11 years and even later. The neural arches fuse posteriorly by 2–3 years and the odontoid fuses at 3–6 years.
The shape of the normal vertebral body in infancy is oval on lateral view radiographs, sagittal CT reformats, and sagittal MRI. The vertebral bodies may later have anterior wedging, especially at the C3 level, which is normal in children up to 7 years of age.
Examine the prevertebral/retropharyngeal space swelling in conjunction with the other findings. The normal prevertebral space should not be greater than 6 mm at the level of C3; however, marked buckling of the soft tissues occurs with neck flexion and in expiration. In order to avoid interpretation errors, the radiographs should be obtained with neck extended and in inspiration, the patient awake in the standing or seated position, if possible. This will allow visualization of the patient’s definite cervical lordosis, which can be falsely underestimated in a supine position. If the image is taken supine, lift the patient’s shoulders from the table, because the relatively larger head of a child can diminish the lordosis. Additionally, the x-ray beam should be completely perpendicular to the region of interest in order to decrease pitfalls.
Measurements
Atlanto-Dental Interval: Distance between the anterior aspect of the dens and the posterior cortex of the anterior C1 ring should be less than 5 mm. If greater than 5 mm, ligamentous abnormalities need to be excluded by MRI to depict bone edema and/or ligamentous injury.
“Pseudo-Jefferson Fracture”: Lateral offset of the C1 lateral masses compared to the lateral masses of the axis of up to 6 mm is normal in children (due to discrepancy in growth rates). The atlanto-dental interval should be normal with this pseudospread of atlas.
Pseudosubluxation: Physiologic motion of C2 on C3 in flexion with anterior displacement of C2 measures up to 4 mm in children under 8 years of age. Pseudosubluxation may be differentiated from true subluxation by the posterior spinolaminar line, which connects the anterior cortices of the posterior C1 and C3 arches (Swischuk line). With true subluxation, the posterior C2 arch does not fall within 2 mm from the Swischuk line.
Constitutional Variants: Occipitalization (assimilation) of the atlas is the osseous fusion of the atlas and the occiput. Basilar invagination is when the tip of the odontoid is at or above the foramen magnum.
Clinical Findings, Implications, and Treatment
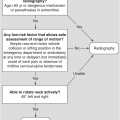
There are many normal variants of the pediatric cervical spine, which can be easily confused with traumatic injuries. The most common presenting symptoms of true cervical spine injury are neck pain, occipital pain, and acute torticollis. If physical examination is unremarkable, unstable cervical spine injury can reliably be excluded in children ≤5 years old.
Additional Information
Atlanto-axial instability (AAI) is present in 10–30% of individuals with Down syndrome. AAI is an increase in the atlanto-dental interval or a decrease in the neural canal width. These patients are usually asymptomatic; however, if the neural canal width is less than 14 mm or the atlanto-dens interval is greater than 4.5 mm on a lateral radiograph, cervical spine MRI should be obtained. If the patient has symptomatic atlanto-axial instability, initial examination should include both a lateral radiograph and an MRI.
References
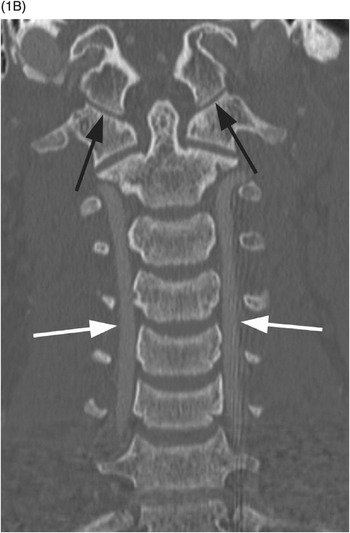
B) Coronal CT image demonstrates a normal atlanto-occiptal interval (black arrows). The vertebral arteries (white arrows) are normal in course and caliber.
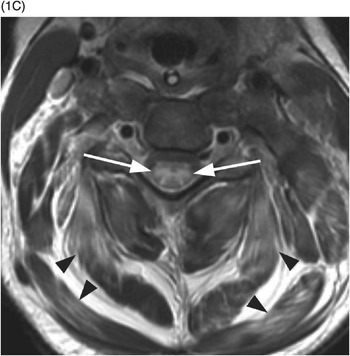
C) Axial T2w MR image shows symmetric cord edema (arrows). There is diffuse myofascial injury with involvement of the paraspinous musculature (arrowheads).
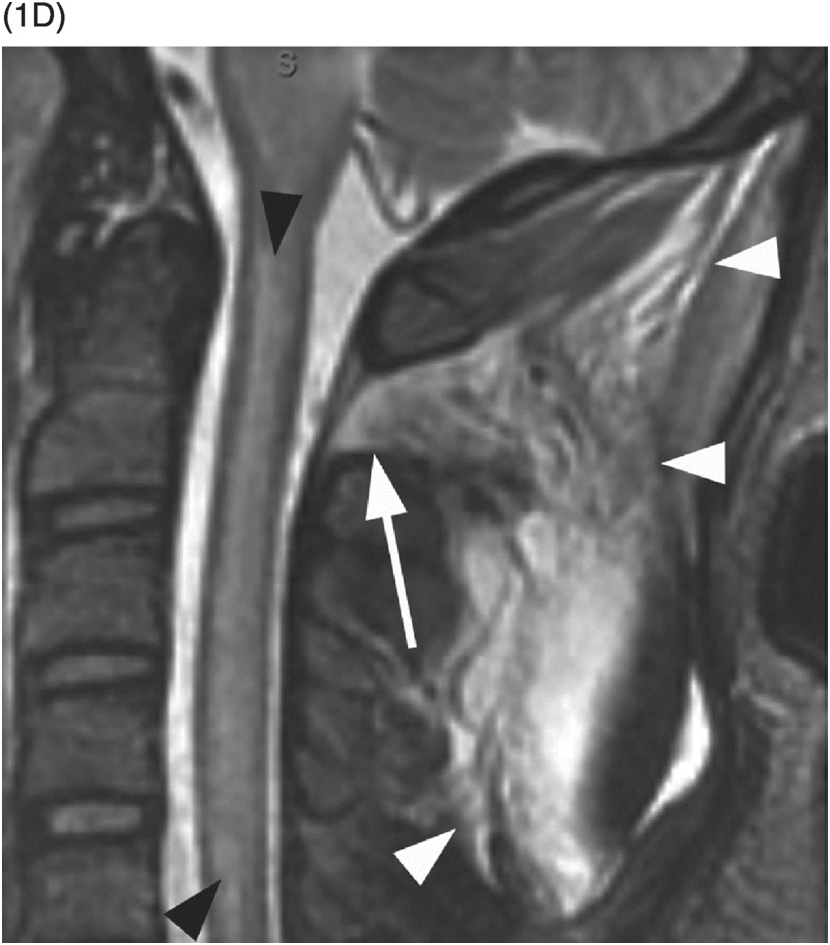
D) Sagittal STIR MR image demonstrates extensive cervical spinal cord edema. There is posterior ligamentous injury at the craniocervical junction with involvement of the posterior atlanto-axial ligament (arrow) and nuchal ligament (arrowheads).
Imaging Findings
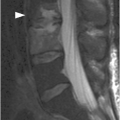
Spinal cord injury without radiographic abnormalities (SCIWORA), as the name would imply, is a syndrome by which patients present with objective signs of myelopathy without plain radiographic or CT abnormalities. Spinal cord injury without CT evidence of trauma (SCIWOCTET) is the same entity in adults with preexisting central canal stenosis and degenerative changes of the cervical spine. Pediatric SCIWORA primarily affects the cervical spine, resulting in cord contusion and axonal injury. STIR is probably the most sensitive MR sequence for depicting soft tissue, ligamentous, and muscular injury and therefore should be performed in all cases of spinal trauma. An acute cord contusion (edema), resulting from either transient subluxation or distraction injury, will appear iso to hypointense on T1WI and hyperintense on T2WI. It is estimated that as many as 35% of patients will have no MR abnormalities, and therefore follow-up imaging is needed to capture the delayed presentation of cord edema. Repeat MRI is typically performed at 1 week and again at 3–6 weeks to evaluate for syrinx, as the incidence of posttraumatic syrinx formation is estimated at 3.5%.
Differential Diagnosis
Spinal Cord Infarct
Typically bilateral anterior gray matter involvement with characteristic symmetric T2 hyperintense lesions (“owl’s eyes”), very bright on DWI (enteroviral infection may look the same); etiologies include trauma (including surgery, especially of the aorta), vasculitis, venous thrombosis, and embolic phenomenon (including fibrocartilaginous emboli); usually no evidence for ligamentous spine injury.
Demyelinating Diseases
Central T2 hyperintense lesion extending three or more vertebral segments with variable post-contrast enhancement pattern; commonly post-infectious or part of the neuro-immune continuum, which includes neuromyelitis optica and acute disseminated encephalomyelitis (ADEM); although the intramedullary lesions may have similar appearance to SCIWORA on imaging, there are no ligamentous injuries.
Clinical Findings, Implications, and Treatment
The presentation of these patients is variable and may range from transient neurological symptoms to complete spinal cord injury. The clinical features of SCIWORA are typically apparent by 48 hours following a traumatic event. Those with minor injuries may demonstrate transient numbness, paresthesias, or paresis. Severe injury can result in one of four neurological syndromes: central cord syndrome, complete cord syndrome, partial cord syndrome, and Brown-Séquard syndrome. SCIWORA patients with minor injuries are treated with external immobilization for up to 12 weeks and requested to avoid high-risk activities for up to 6 months.
Additional Information
The mechanism of injury in SCIWORA is related to hyperextension and flexion, which results in transient vertebral dislocation or distraction. This condition commonly occurs in children less than 8 years of age as a result of increased laxity and elasticity of the developing cervical spine. Extreme extension/flexion can disrupt vertebral and anterior spinal arteries, leading to cord ischemia and/or infarct. Hypermobility of the vertebral column with respect to the cord leads to distraction and transection type injuries. Congenital cervicospinal anomalies may further predispose children to development of SCIWORA and related syndromes.
References
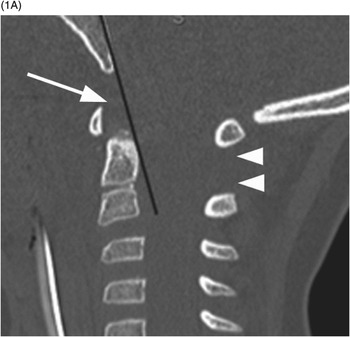
A) In this 3-year-old patient post motor vehicle collision, the Wackenheim line (black line) fails to pass through the odontoid process on this midsagittal CT image, suggestive of atlanto-occipital distraction. The image also shows increased dens-basion interval (arrow) and atlanto-axial instability (arrowheads).
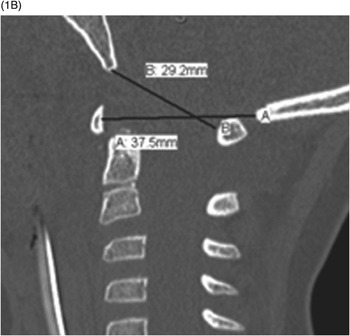
B) A calculated Powers ratio in the same patient was normal (29 mm/37 mm = ~0.8, less than the normal value of 0.9), indicating the importance of using several techniques in evaluation of AOD.