Treatment Strategy
Surgery and radiotherapy are equally effective in curing most skin cancers. The choice of treatment modality is determined by several factors, such as functional and cosmetic results, patient age and occupation, treatment time, and cost. Surgery is preferred for most patients, particularly for younger patients who have years of exposure to sunlight ahead of them.
Primary radiotherapy is often indicated for lesions on and around the nose, lower eyelids, and ear, where it can usually attain better functional and cosmetic results than surgery. Extensive lesions of the cheek and oral commissures, which would require full-thickness resection, may also show better results on irradiation.
Postoperative radiotherapy is indicated for positive surgical margins, perineural invasion, and invasion of bone, cartilage, and skeletal muscle.
Rarely, patients have adenopathy at diagnosis. The choice of treatment of the nodal disease is determined by the type of therapy selected for the primary lesion and by the size of the node. A combination of surgery and radiotherapy is indicated when nodal disease is >3 cm or when ECE is present.
Primary Radiotherapy
Target Volume
The initial target volume encompasses primary tumor with 1- to 2-cm margins, depending on the size, location, and type of tumor (well-circumscribed vs. ill-defined border). Elective nodal irradiation is not indicated except when the primary is a large, infiltrative squamous cell carcinoma (SCC) or poorly differentiated.
The boost volume encompasses primary tumor with 0.5- to 1-cm margins, depending on the size, location, and type of tumor.
Setup and Field Arrangement
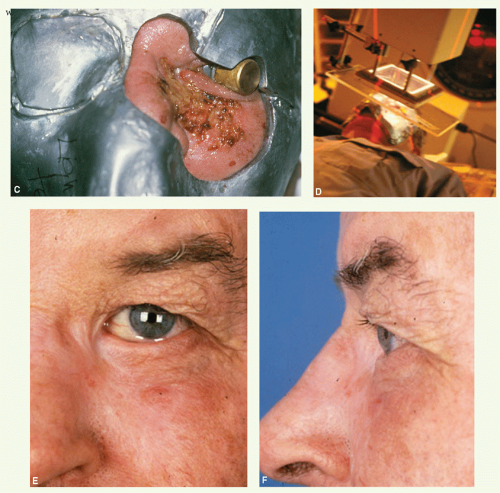
The patient is immobilized in a position that gives the best access to irradiate the tumor (preferably the plane of the skin to be treated is parallel to the surface of the treatment couch to avoid the need for gantry rotation) (see
Fig. 16.1).
An appositional field is used in most cases. The borders of the field are chosen to include a 1- to 2-cm margin of normal skin around the tumor (up to 1 cm for lesions <l-cm tumor and 1 to 2 cm for larger tumors). Margins may be smaller when treating areas close to the eye. More generous margins are appropriate for lesions with an ill-defined border.
Radiation treatment is given with orthovoltage x-rays (usually 75 to 125 kilovolt potential [kVp]) or electrons (usually 6 to 12 MeV). The energy of x-rays or electrons is chosen on the basis of the thickness of tumor. The energy of electron beams should be selected so that the distal 90%-isodose line is a few millimeters deeper than the base of the tumor, including surface bolus.
The treatment distance for x-rays also depends on the thickness of the lesion. A 23-cm focus skin distance (FSD) cone is appropriate for superficial tumors, whereas a 50-cm FSD with open fields and skin collimation is preferable for thicker lesions to avoid a large dose gradient across the lesion. The FSD for electrons is usually 100 cm.
A custom-made lead cutout is used for skin collimation. The cutout should be large enough so that the portal size for an electron beam is at least 4 × 4 cm.
Skin bolus or a perspex scatter plate is used with electrons to ensure full surface dose.
An internal eye shield is inserted when treating an eyelid lesion with orthovoltage x-rays or with electrons of 8 MeV or less. (Note: Eye shields should be individually calibrated with respect to the electron attenuating properties.)
Dose
Effective regimens for treating most skin cancers include a dose of 50 to 55 Gy in 20 fractions, a dose of 45 Gy in 15 fractions, or a dose of 40 Gy in 10 fractions. In general, protracted treatment provides better cosmetic results.
For large tumors close to crucial structures (e.g., eye), maximum tolerance is obtained with a dose of 60 to 70 Gy in 30 to 35 fractions
(see Case Study 15-1).If the patient is in poor general condition, hypofractionation (e.g., 4 fractions of 8 Gy) may be used.
Dose Specification
x-Rays are prescribed at DMmax with electrons at the 90% line. This difference in prescription accounts for the relative biologic effectiveness difference between the two beam qualities.
Postoperative Radiotherapy
Most frequent indications are lymphatic spread to the parotid gland, upper neck nodes, or both, and perineural extension along the branches of the trigeminal nerves, facial nerves, or both.
Target Volume
The initial target volume encompasses the primary tumor bed and ipsilateral parotid and neck nodes, or trigeminal or facial nerve pathways, depending on the indication.
The boost volume encompasses areas of known disease with 1- to 2-cm margins.
Setup and Field Arrangement
For the treatment of parotid and neck nodes or branches of the facial nerve, the technique is similar to that for primary parotid tumors (see
Chapter 13). The patient is immobilized in an open neck position. The anterior margin of the parotid portal can be slightly less generous because there is no need to encompass the parotid duct. Treatment is given with an electron beam of appropriate energy (e.g., 12 MeV for parotid and upper neck nodes and 9 MeV for lower neck nodes).