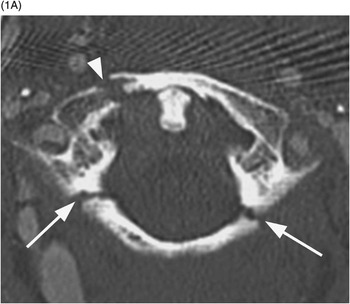
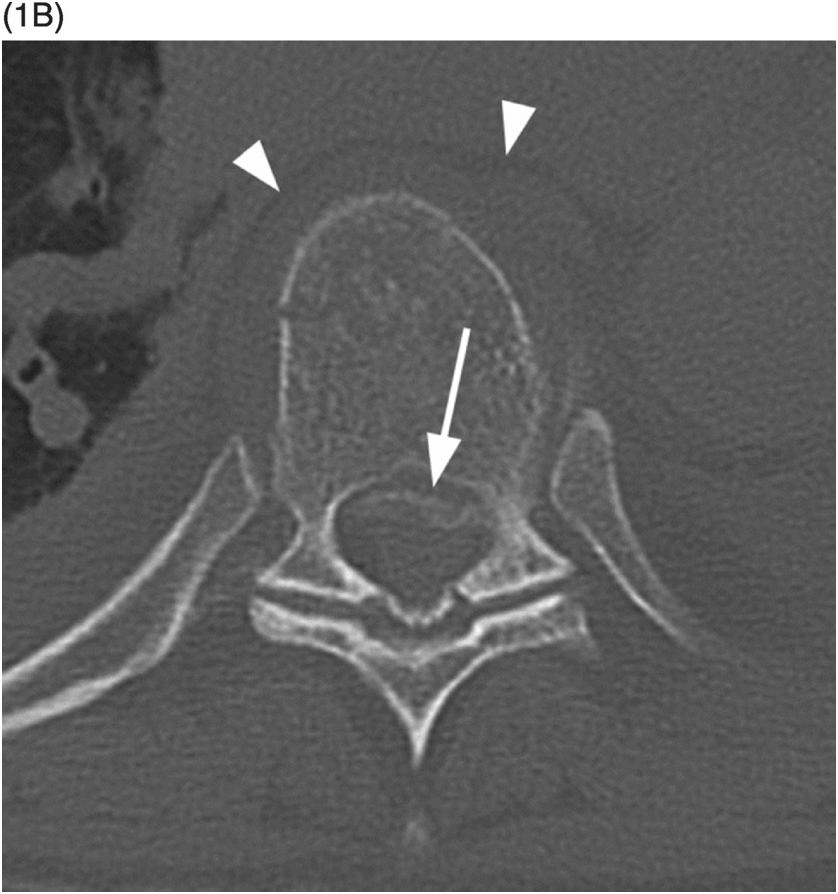
B) Coronal CT shows a normal relationship between the lateral masses of C1 and C2. The atlanto-occipital joints are difficult to see because of obliquity, but the biconcave inwardly sloping wedge appearance of the C1 lateral masses is noted. This causes a centrifugal force when the atlas is loaded axially.
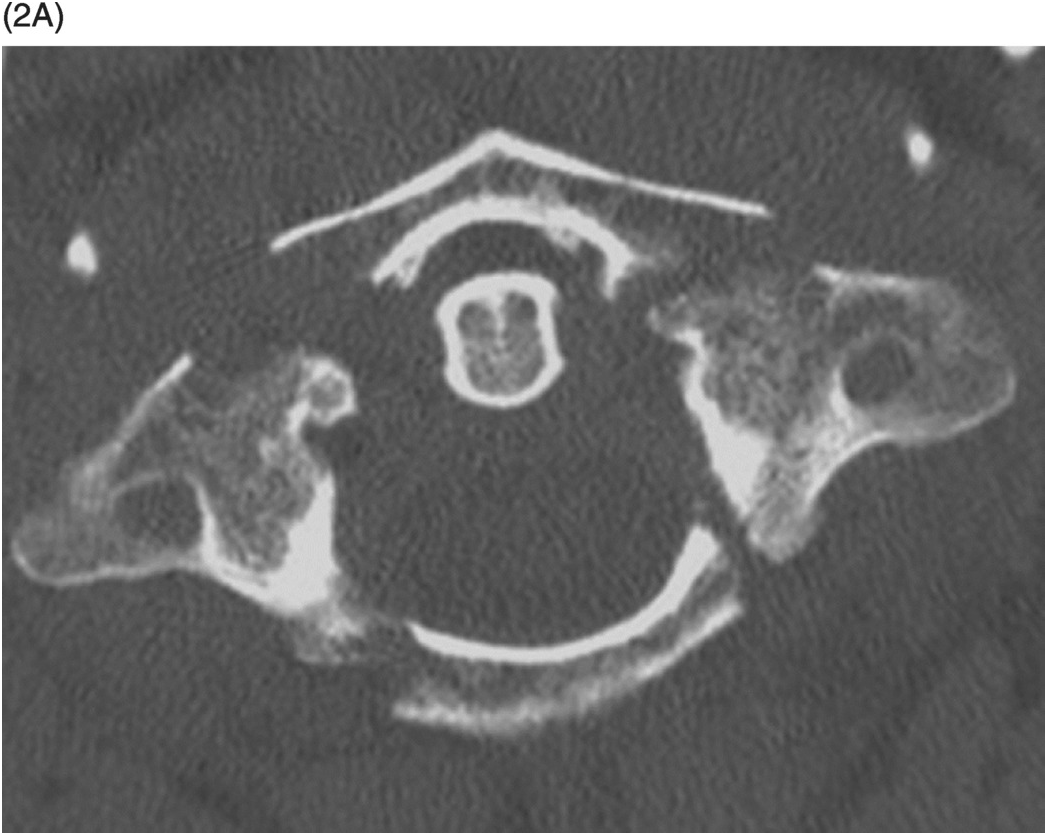
B) Coronal CT image shows outward displacement of the lateral masses of C1 relative to C2 (arrows) measuring 6 mm on the right and 4 mm on the left. A fracture on the right between the dens and atlas (arrowhead) is consistent with a bony avulsion of the transverse ligament from C1. An additional more superior fracture on the right adjacent to the occipital condyle is consistent with an alar ligament avulsion.
Imaging Findings
Burst fractures of the atlas involve both the anterior and posterior arches and are considered type II within the Landells and Van Peteghem classification scheme. While all atlas fractures were classically described by Sir Geoffrey Jefferson, it is best to reserve the description Jefferson exclusively for burst injuries. These are to be distinguished from type I fractures of the atlas, which involve the anterior or posterior arch alone, or type III fractures, which involve the lateral mass of C1.
Despite primarily nonoperative treatment, the integrity of the transverse ligament is central to management of Jefferson fractures. Dickman type I injuries of the transverse ligament involve a midsubstance tear or non-bony avulsion from C1, while type II transverse ligament injuries involve avulsion of bone. On CT, an atlanto-dental interval of >3 mm or combined overhang of 7 mm of the lateral masses of C1 relative to C2 are consistent with transverse ligament disruption. The utility of these criteria has been questioned, and MRI dedicated to evaluation of the transverse ligament has been advocated.
Differential Diagnosis
Isolated Anterior or Posterior Arch Fractures or Lateral Mass Fractures of C1
Clinical Findings, Implications, and Treatment
More than 80% of C1 fractures are due to motor vehicle accidents or falls. Presentation is with neck pain and decreased range of motion. Neurologic injury secondary to cord compromise is uncommon with Jefferson fractures due to outward displacement of fracture fragments. However, approximately 40% of all C1 fractures are accompanied by C2 fractures, placing the patient at a greater risk for cord injury. While pain and neuropathy related to the C2 nerve are common, inferior cranial nerve injuries are not.
Stability of isolated Jefferson fractures is primarily based on the status of the transverse ligament. An atlanto-dental interval of >3 mm or lateral mass atlanto-axial combined overhang of >7 mm is consistent with transverse ligament tear and instability. Additionally, Dickman type I ligament injuries (substance tears) heal poorly compared to type II (bony avulsion) injuries. The decision to evaluate the transverse ligament directly via MRI is based on CT findings suggesting instability and the level of clinical suspicion, which incorporates the mechanism of injury. Most Jefferson fractures are treated with rigid cervical collar stabilization for 10–12 weeks with follow-up flexion-extension radiographs for instability. Unstable fractures are usually treated with halo fixation, C1–C2 posterior screw fixation, or occipital-cervical fusion. Recent studies have highlighted the morbidity of halo fixation, particularly in elderly patients, furthering the trend of C1–C2 fixation for unstable Jefferson fractures and rigid collar use for stable fractures.
Additional Information
While all fractures of C1 are associated with some degree of an axial force, the type II burst injury is due to the most direct compression from a blow to the vertex of the skull (vertical compression). On coronal images, the lateral masses of C1 are anatomically wedge-shaped sloping inward. Therefore, an axial loading injury is translated to a centrifugal force, with the bony ring failing due to distraction. Failure most typically occurs in the arches just anterior or posterior to the lateral masses. When internal fixation is considered, the indentation caused by the horizontal lateral-medial course of the vertebral artery over the posterior arch as well as the possibility of a ponticulus posticus variant must be taken into account.
References
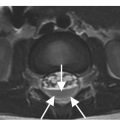
B) Axial CT through that level clearly demonstrates the fracture fragment within the spinal canal (arrow). There is also perivertebral hematoma (arrowheads).
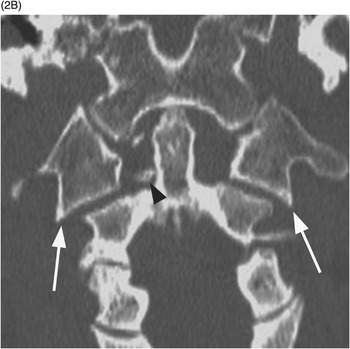
Figure 27.3 Midsagittal T2-weighted MRI in another patient shows burst fracture of L1 vertebral body with retropulsion of the fractured superior posterior corner (arrow) into the spinal canal. The fracture is compressing the conus medullaris; intramedullary edema is present more superiorly. There is also edema in the posterior soft tissues with possible disruption of the posterior ligamentous complex.
Imaging Findings
These injuries are usually found at the thoracolumbar junction – transition zone (T11–L1). There is loss of vertebral height, more in the anterior part; the fracture always involves posterior vertebral body cortex, so that the anterior and middle vertebral columns are always affected. There is a burst appearance of the vertebral body on axial CT, often with sagitally oriented fracture line. Retropulsion of the posterior vertebral body fragments is a characteristic finding, usually the superior posterior corner. Interpedicular widening is best seen on AP radiographs and CT images reconstructed in coronal plane. MRI demonstrates band-like marrow edema surrounding the fracture line, best seen in fat-suppressed T2-weighted images, and may also show spinal cord contusion and/or epidural hematoma.
Differential Diagnosis
Wedge Fracture, (Simple) Compression Fracture
Posterior vertebral body cortex and posterior column elements are intact, without retropulsion into the spinal canal; less than 40% loss of vertebral body height in patients with normal bone density.
Chance Fracture
Anterior wedge fracture with extension of the fracture horizontally through posterior elements or separation of facet joints and spinous processes, possibly also retropulsion of posterior cortex (“burst-Chance” fracture); this is a distraction injury.
Fracture-Dislocation
Spondylolisthesis, due to shearing or distraction, usually with MR evidence of anterior and posterior longitudinal ligament injury.
Pathologic Fracture Due to Tumor Infiltration
Usually compression fracture, rounded area of abnormal appearance on MRI, possibly epidural or paraspinal mass and involvement of other vertebrae.
Butterfly Vertebra
Well-corticated congenital vertebral malformation, no history of trauma.
Clinical Findings, Implications, and Treatment
The common mechanism of injury is fall from height on feet, resulting in excessive axial loading and driving an intervertebral disc into the adjacent vertebral body. Thoracolumbar junction is most frequently affected due to the difference in mobility of ribcage-stabilized rigid thoracic spine and relatively mobile lumbar segments. Back pain is the main presenting symptom. Retropulsion of fragments may cause spinal cord injury, and up to 30% of patients have some degree of neurologic deficit. Radiological report should include the percentage of spinal canal stenosis, assessment of kyphosis angle, and presence of interspinous widening. The Thoracolumbar Injury Classification and Severity Score (TLICS) takes into account three major parameters: injury morphology, integrity of the posterior ligametous complex, and neurologic status of the patient. Surgical treatment is necessary in case of progressive neurological loss, unstable fractures with complete neurological loss, or polytrauma. In case of intact neurology, the opinions differ. The usual treatment is conservative, with initial bed rest and subsequent application of extension cast or brace and early mobilization. The degree of spinal canal stenosis seems to be less important, as most of stenoses significantly regress over period of one year due to resorption of retropulsed bony fragments. The neurological deficits are thought to be a consequence of initial injury rather then later continuous cord compression. Integrity of the posterior ligamentous complex seems to be a positive predictive factor for neurological recovery.
Additional Information
Burst fracture is more severe (assigned 2 points in TLICS classification) than a simple compression fracture (1 point), the differentiating feature being fracture of the posterior vertebral body cortex with retropulsion of fragments into the spinal canal. Distraction fracture (such as Chance fracture) is even more severe (4 points) with disruption of all 3 columns.
References
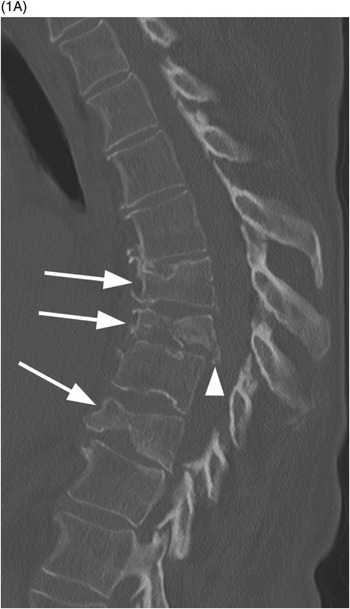
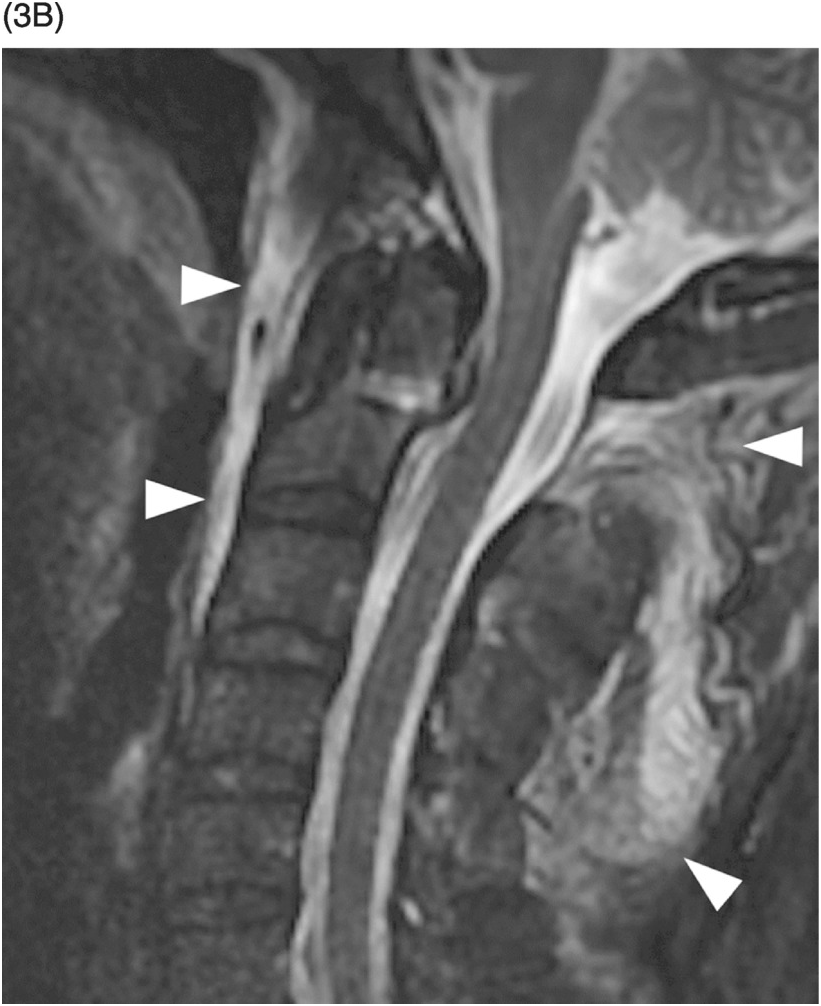
A) Midsagittal reformatted CT image shows a dens fracture type 2 (arrowheads) with mild diastasis.
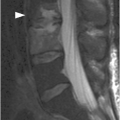
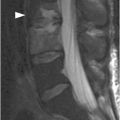
B) Corresponding STIR MR image shows interspinous ligament edema (arrow) and a prevertebral fluid collection (arrowhead) indicating anterior longitudinal ligament injury. Note that there is no evidence of bone marrow edema with this extension injury.
A) Midsagittal CT image shows a dens fracture type 2 with mild angulation and diastasis.
B) Corresponding STIR image confirms the fracture, without signs of spinal cord injury. There is extensive hyperintensity of the prevertebral and interspinous soft tissues (arrowheads), consistent with ligamentous injury. No evidence of bone marrow edema.
Imaging Findings
Odontoid fractures type 2 occur at the base of the dens between the level of the transverse ligament and the C2 vertebral body. On plain radiographs, even on good-quality antero-posterior, lateral, and open-mouth views, the findings may be subtle and lesions may be missed. Multislice CT with multiplanar reconstructions is the modality of choice to demonstrate the fracture, its orientation, and the C1–C2 relationship. Sagittal CT reconstructions are particularly helpful for treatment guidance, as they reveal the angulation of the fractured dens and its anterior or posterior displacement. Coronal and axial CT images are necessary to establish the lateral displacement of the dens from the C1 lateral masses. A thorough search for fracture fragments and associated contiguous and noncontiguous fractures should be performed, as they can change the treatment strategy. CT may depict significant soft tissue abnormalities, but MRI, with T1w and fat-suppressed T2w (STIR or fat-sat T2w) images, is the imaging modality for detection of bone marrow edema, ligamentous injuries, as well as spinal canal hematomas and spinal cord lesions.
Differential Diagnosis
Os Odontoideum
Usually round or oval, smooth and with well-corticated margins, separated from the C2 vertebral body by a wider gap than that of a generally narrow fracture; usually hypertrophic anterior arch of C1 with which it may be fused.
Non-Union of Dens Fracture
Fracture with smooth and sclerotic edges; the gap of the fracture is usually narrow.
Odontoid Fracture Type 1 / 3
The fracture involves the tip of dens above the transverse ligament / extends into the C2 vertebral body, respectively.
Clinical Findings, Implications, and Treatment
Patients with an odontoid fracture typically present with neck pain following trauma. These are the most common fractures of the geriatric cervical spine. The frequency of associated neurologic symptoms is variable and is generally associated with dens displacement. Type 2 odontoid fractures have a high non-union rate due to typical instability and micro-motion at this fracture site and the limited vascular supply at the watershed region of the dens base, which decrease the healing potential. Advanced age and osteoporosis are the two main risk factors for pseudoarthrosis. The treatment of type 2 odontoid fractures is still controversial, especially in elderly patients: nonoperative rigid immobilization generally consists of a collar or halo; operative treatment may be one of the several posterior C1–C2 fusion techniques or anterior screw fixation. It has been proposed that patients with instability and dens dislocation >5 mm should be considered candidates for surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree