Subtrochanteric Femur Fractures
Fractures of the subtrochanteric region of the proximal femur can be especially challenging to manage, and they warrant special consideration to obtain consistently satisfactory results. The subtrochanteric zone of the femur is generally considered to include the area extending 5 cm distally from the inferior border of the lesser trochanter, or the junction of the proximal one third and middle third of the femoral shaft (Fig. 27.1). Fractures that have their major displacement in this area are considered subtrochanteric fractures despite the possibility that some of them may extend into the trochanteric area proximally or the distal femoral shaft. Subtrochanteric fractures occur with a bimodal distribution.1–5 Fractures seen in young patients tend to occur as a result of high-energy trauma and often have significant comminution, whereas fractures occurring in older patients are often caused by low-energy injuries. Subtrochanteric femur fractures suffered by elderly patients after low-energy injuries are considered fragility fractures. As such, the incidence of geriatric subtrochanteric femur fractures is increasing with the aging of the population. Additionally, patients with fragility fractures in the subtrochanteric region of the femur are more likely to be obese or suffer from dementia than are patients with hip fractures.6

Features unique to subtrochanteric fractures that complicate treatment include both anatomic and biomechanical characteristics. The subtrochanteric area of the femur is primarily cortical bone that heals more slowly and tends to fracture with comminution. The femoral medullary canal widens in the intertrochanteric area, which makes intramedullary fixation in this region more difficult because of the possibility of less secure fixation and higher risk of malunion. Intramedullary nails do not fill the capacious proximal canal and therefore do not effect a reduction of the fracture as the nail is passed across the fracture site, as may occur in the midshaft area. If the fracture is malaligned as the nail is passed, it will remain in the malaligned position; therefore, the fracture has to be held in a reduced position as the intramedullary fixation is accomplished. In the subtrochanteric region, special reduction techniques may be needed because there are strong deforming forces across these fractures. Biomechanically, the subtrochanteric area of the proximal femur is an area of high stress concentration, which has led to high rates of implant failures in the treatment of these fractures.7
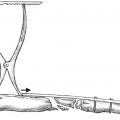
There are large muscles that insert on the proximal femur and create strong deforming forces across the fracture that make fracture reduction difficult. The gluteus medius and gluteus minimus insert on the greater trochanter and function as strong hip abductors. The piriformis, gemellus superior, and gemellus inferior also insert in this area and function as external rotators of the hip. The iliopsoas inserts on the lesser trochanter and acts to flex and externally rotate the hip. These muscles account for the deformity typically seen in these fractures (Fig. 27.2). The proximal fragment is flexed, abducted, and externally rotated, and the distal segment is adducted and shortened by the action of the adductors and hamstrings. Unlike many fractures in which the reduction is accomplished by moving the distal segment into alignment with the stationary proximal fragment, reduction of these fractures requires movement of both segments because it is not possible to move the distal segment alone into satisfactory alignment with the proximal fragment. This understanding is critical to gaining acceptable alignment regardless of the type of fixation selected.

The high mechanical stresses in this area occur as a result of the compressive force of the body′s weight as well as additional forces generated by the muscles that insert upon the fracture fragments. These forces have been studied by numerous investigations. Major compressive stresses in the femur are greatest in the medial cortex 1 to 3 inches below the lesser trochanter and can exceed 1,200 pounds per square inch.7 This area is the most highly stressed area in the body. Tensile stresses of approximately 25% less are experienced at the lateral cortex at the level of the lesser trochanter.7
Classification
There are numerous classification systems for subtrochanteric fractures; a recent review identifying 15 previously described classifications.8 Most of these classification systems are not currently used and will not be discussed in deference to those that are more useful. The Russell-Taylor classification is based on the presence or absence of fracture involvement at the lesser trochanter and posteromedial buttress and the presence or absence of extension into the greater trochanter and piriformis fossa (Fig. 27.3).2 This classification may be of use in selecting a biomechanically appropriate implant for definitive treatment. Two questions are asked: (1) Is there extension into the piriformis fossa? (2) Is the lesser trochanter and posteromedial buttress intact? In this classification, group I fractures do not have extension into the piriformis fossa or greater trochanteric area and thus are considered to be most suitable for treatment with intramedullary nails, with either a standard piriformis fossa or greater trochanteric starting point. Type IA fractures do not involve the lesser trochanter or posteromedial buttress; therefore, standard locking nails can be used for treatment of this fracture pattern. Type IB fractures do involve the area of the lesser trochanter and therefore are not treated with standard locking nails but instead can be treated by nails with cephalomedullary proximal locking (screw or blade up into the femoral head). Group II fractures have extension into the piriformis fossa and greater trochanteric area and are therefore less suitable for intramedullary fixation using an implant with a piriformis fossa starting point. These fractures are best treated with either 95-degree fixed-angle implants or trochanteric entry nails. Group IIA fractures do not have involvement of the lesser trochanteric area and thus have an intact posteromedial buttress. Group IIB fractures have significant involvement of the lesser trochanteric area and lack an intact posteromedial buttress, which has implications for treatment and increases the risk of implant failure. Traditionally, plate fixation was recommended over intramedullary nail fixation in those fractures with extension into the piriformis fossa. This was because greater trochanteric nails were not available. Several variations of greater trochanteric entry cephalomedullary fixation nails are now available. In addition, percutaneous reduction techniques used with nailing have become refined. Thus, utilization of intramedullary fixation for the group II fractures is more common, with restoration of good alignment and good outcomes.

The Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification of fractures considers these fractures as diaphyseal fractures.9 The femoral shaft is represented as bone 3 and segment 2 (diaphyseal segment). The proximal limit of the diaphyseal segment is a transverse line passing through the inferior edge of the lesser trochanter. Although this classification is not used for the general clinical management of these injuries, it is useful in collecting data for descriptive purposes and research.
Atypical subtrochanteric femur fractures are not described by a separate classification, but they are increasing in frequency.10 Although many questions remain regarding these injuries, the existing evidence suggests they are stress or insufficiency fractures that may occur in the setting of bisphosphonate therapy.10–13 The fracture pattern for these injuries is well described and consistent, and has been shown to have decreased healing compared with standard subtrochanteric fractures, which may have implications for the method of treatment selected.11,13,14 These atypical fractures occur in the subtrochanteric region of the femur, have a transverse or short oblique fracture pattern, occur after minimal of no trauma, have a medial spike when the fracture is complete, and have no comminution. Additionally, they often have cortical thickening, a periosteal reaction of the lateral cortex, and bilaterality12 ( Fig. 27.4). Radiographs of the contralateral femur should be obtained because the stress or insufficiency fractures have a high rate of secondary displacement and a low rate of healing with nonoperative management and as such may benefit from fixation when found to be nondisplaced at the time of diagnosis.12

Nonoperative Management
There is little role for the nonoperative management of these injuries in the adult. Nonoperative treatment requires prolonged immobilization with associated significant morbidity and mortality to the patient. High rates of local complications also occur with nonoperative treatment, including nonunions, malunions, and soft tissue complications.15–17 Nonoperative treatment is reserved for the rare case of a nonambulatory patient with a low-energy fracture and minimal pain for whom surgery is deemed to be too risky to the patient from a mortality standpoint.
Surgical Treatment
Indications
Treatment for subtrochanteric fractures in adults is primarily operative. Operative options include plates or intramedullary implants. Intramedullary nails are typically placed with closed methods, although open reduction and nailing of displaced or highly unstable fractures is occasionally necessary. In contrast, plating of femur fractures has been traditionally performed with open techniques, but less invasive techniques of indirect fracture reduction and plate fixation have also been reported.18–25
Intramedullary implants include those designed to enable a trochanteric or piriformis starting point with standard proximal locking or with cephalomedullary proximal locking. Intramedullary hip screw implants with a trochanteric entry point are used also. Plate options include 95-degree fixed-angle implants such as condylar blade plates or dynamic condylar screws, proximal femur locking plates, 135-degree sliding hip screws, and the Medoff sliding plate26 (Medpac, Inc., Valencia, CA). Fixed-angle plates are preferred; higher rates of complications are noted when sliding plates are used to repair subtrochanteric fractures, which is also true for intertrochanteric fractures when the primary fracture line has a reverse obliquity component (Fig. 27.5).27–29 Indications for each of these implants with advantages, disadvantages, and techniques are discussed in this section.

Surviving the Night
Patients with either high- or low-energy injuries require a careful preoperative evaluation, as both types of injury may entail conditions (acute or chronic) that need attention prior to surgery. High-energy subtrochanteric femur fractures rarely occur as isolated injuries, and low-energy subtrochanteric fragility fractures rarely occur in a healthy host. Both of these patient groups require a multidisciplinary approach to care with involvement of the appropriate general surgery and medical teams.
Following high-energy trauma, overall blood loss may be significant, and fracture stabilization aids in minimizing fracture-related bleeding while also reducing pain. This may be accomplished during the prehospital phase of care with the use of commercially available traction devices available to emergency technicians. Once the patient arrives at a hospital, skeletal traction can be instituted by qualified personnel. If significant delay in definitive care is expected due to the patient′s clinical condition, balanced skeletal traction should be considered to accommodate the forces acting on the proximal segment.30 A good understanding of the fracture pattern must be obtained prior to operative stabilization. Specifically, the surgeon should determine if there is extension of the fracture line into the piriformis fossa or if there is a frontal plane split into the greater trochanter fragment. This may often be better delineated with a traction view of the proximal femur or a computed tomography scan.
Once the patient′s condition has been optimized and the appropriate personnel and resources are available, surgical stabilization should be performed expediently. Early surgery may limit ongoing blood loss and pain. Severely injured patients with ongoing resuscitation needs and patients with severe medical illnesses that can be further optimized may not be cleared for surgery for a significant amount of time. These patients generally can be maintained in traction, although certain circumstances may be amenable to external fixation with the potential to incorporate the pelvis into the construct.
As with all major extremity injuries, compartment syndrome, although rare, can occur in patients with femur fractures, resulting in major complications. Recognition of its possible occurrence is imperative, and the treatment is emergent fasciotomy.31,32
Intramedullary Nails
Video 27.1 Unreamed Femoral Nailing
Video 27.2 Trochanteric Nail for Reverse Oblique Subtrochanteric Fracture
Standard interlocking intramedullary nails offer the advantage of familiarity to most surgeons, the biomechanical advantages of an intramedullary implant, the ability to be placed by a closed technique, and good outcomes. Nails with standard proximal interlocking screws are suitable only for subtrochanteric fractures that are completely distal to the lesser trochanter (Fig. 27.6). Cephalomedullary locking (sometimes called second-generation) intramedullary nails offer the same advantages of intramedullary fixation but are technically more demanding because the proximal interlocking screw must be placed in the appropriate position in the femoral head. These implants are suitable for fractures that extend proximal to the lesser trochanter but do not involve the piriformis fossa or greater trochanter (Fig. 27.7). However, with careful technique and great care to obtain the reduction, these implants have been extended to use in fractures extending proximally into the trochanteric and piriformis area (Fig. 27.8). Intramedullary hip screws are also options for those complex fractures with proximal trochanteric extension. Intramedullary hip screws (also referred to as trochanteric nails) are designed to be inserted through a trochanteric starting point, and they incorporate a large hip screw or blade device that is inserted into the femoral head (Fig. 27.9). These implants offer the advantages previously cited for intramedullary devices, and extend the indications for the use of intramedullary implants. However, trochanteric nails have the unique disadvantage of requiring the removal of a significant amount of proximal femoral bone. To accommodate the large femoral head screw and remain biomechanically sound, the proximal portion of the nail must be large, usually on the order of 17 mm. This requires the surgeon to create a large hole in the tip of the greater trochanter, necessitating significant bone removal and loss of a portion of the area of insertion of the hip abductors. Insertion of the locking device into the femoral head also requires removal of significant bone from the lateral cortex of the femur as well as removal of bone from the femoral head and neck for its placement. As a result, abductor dys-function, insertional site pain, and difficulty with later reconstructive options can occur.




Other disadvantages of intramedullary implants include the difficulty with fracture reduction. The fracture has to be reduced prior to passing the guidewire, and the reduction has to be maintained until the nail is fully seated and locked proximally (Fig. 27.10). This often requires manipulation of both the proximal and distal fragments. The nail does not aid with the reduction for reasons previously mentioned. Additionally, the starting point can be more difficult to locate due to the abducted position of the proximal fragment; therefore, a trochanteric starting point may be easier to obtain in these fractures. If a trochanteric starting point is selected, it is important to avoid varus malalignment.


Plates
Video 27.3 Blade Plate
Video 27.4 Proximal Femoral Locked Plating
Video 27.5 ORIF of Femoral Neck and Subtrochanteric Fracture
The 95-degree fixed-angle plate devices can be used for all subtrochanteric fractures but are particularly indicated for those with proximal trochanteric extension and a very short proximal segment, where the use of a nail with a piriformis or trochanteric starting point would be more difficult (Fig. 27.11). The condylar blade plate offers the unique advantage of minimal bone removal and the ability to accomplish an indirect reduction once the blade has been placed in the correct position in the femoral head. Thus, the plate helps reduce the fracture. Its primary disadvantage is biomechanical; the extramedullary position on the lateral cortex of the femur results in increased stresses on the implant and on the implant–bone interface. An additional disadvantage is that many surgeons are unfamiliar with its use.

Our algorithm for the treatment of subtrochanteric femur fractures is as follows: For fractures 2 or 3 cm or more distal to the lesser trochanter, a standard locking piriformis fossa entry intramedullary nail is used. Subtrochanteric fractures that extend proximally into the area of the greater trochanter or trochanteric fossa may be treated with a 95-degree-angle condylar blade plate or cephalomedullary locking intramedullary nail. The choice between these two implants is based on the degree of fracture comminution, the bone quality, the amount of distal extension of the fracture, and the presence of other fractures in the femur. A trochanteric nail is used in older patients with poor bone quality to enable a single large screw to be placed centrally in the head where the highest quality bone is located. For those fractures with extension into the area of the lesser trochanter but no involvement of the piriformis fossa or greater trochanter, either a 95-degree-angle condylar blade plate or a cephalomedullary nail is used; the choice depends on other factors as discussed above.
Surgical Technique
The operative technique for the three common methods of fixation of subtrochanteric fractures will be described: (1) cephalomedullary locking intramedullary nail with a piriformis fossa or trochanteric starting point, (2) a trochanteric nail, and (3) a 95-degree-angle condylar blade plate.
Positioning
Patient positioning may be the same for all three of these fixation techniques. Either supine or lateral positioning may be used depending on the surgeon′s preference, the presence of other injuries, and the patient′s body habitus. Supine or lateral positioning can be achieved either on a flap-top radiolucent table or a fracture table.
Tips and Tricks
Reduction of subtrochanteric femur fractures requires movement of both proximal and distal segments because it is not possible to move the distal segment alone into satisfactory alignment with the proximal fragment. This is because of the flexed, abducted, and externally rotated position of the proximal segment. This understanding is critical to gaining acceptable alignment of the fracture, no matter what of type of fixation is selected.
Lateral positioning facilitates exposure of the proximal femur and reduces the posterior sag that can occur with supine positioning. We prefer to position the patient on a radiolucent table with large bumps located beneath the affected hip and ipsilateral shoulder to maintain the patient somewhere between the supine and lateral position (Fig. 27.12). The arm on the affected side is padded and placed over the chest. The bump must be large enough to roll the patient sufficiently forward so that when the C-arm is in the full lateral position (i.e., X-ray beam parallel to the floor), an unencumbered lateral view of the hip can be seen. If the soft tissue shadow of the contralateral thigh overlaps the image of the hip, then the patient needs to be rolled more toward the lateral position, with a larger bump to raise the affected side even higher. Typically, the patient is positioned at an angle of approximately 40 to 50 degrees to the bed. Because the proximal fragment is externally rotated due to the pull of the short external rotators, this position enables a true lateral view of the hip.

The lower abdominal area, pelvic area, and entire lower extremity are prepped and draped into the field. Prior to positioning and draping, the opposite extremity measurements of rotation and length of this extremity should be determined. Rotational alignment can be clinically measured with medial and lateral thigh rotation, and length is measured with a radiographic ruler for comparison with the affected extremity after fixation for those cases with severe comminution (Fig. 27.13).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree