Abstract
Perimedullary arteriovenous fistulas (PMAVFs) are rare spinal vascular lesions, particularly in pediatric patients. We present a pediatric case of a ruptured cervical PMAVF, successfully treated with endovascular embolization, along with a review of relevant literature. A 10-year-old boy with no significant medical history initially presented with neck pain and fatigue, progressing to paralysis in his upper limbs and eventually all extremities. His condition further deteriorated, leading to impaired consciousness and respiratory distress, necessitating transfer to our pediatric intensive care unit for intubation and management. Head magnetic resonance images revealed medullary edema and dilated veins in the posterior cranial fossa. At the same time, contrast-enhanced computed tomography of the neck showed an intramedullary hematoma centered at C4, with edema extending from the medulla oblongata to T3 and dilated vessels surrounding the lesion. Angiography confirmed a varix rupture of the PMAVF with feeders from the right C4 dorsal root artery and the right ascending cervical artery. Endovascular embolization was performed using 33% n‑butyl‑2-cyanoacrylate through a microcatheter placed just beyond the fistula. The shunt was successfully occluded. Postoperatively, following a tracheotomy, the patient was gradually weaned off the ventilator. With rehabilitation, he showed significant improvement in spinal cord function, including regaining the ability to transfer with a walker. Endovascular embolization is a viable treatment option for pediatric PMAVF, as demonstrated in this case, where a single-stage procedure achieved successful occlusion and significant neurological recovery.
Introduction
Perimedullary arteriovenous fistulas (PMAVFs) are rare spinal vascular diseases classified as type IV spinal cord arteriovenous malformations [ , ], especially in pediatric patients. PMAVFs, first reported in 1977 by Dindjian et al. [ ], are often associated with significant morbidity, involving bleeding due to aneurysmal or varix rupture and progressive spinal cord dysfunction caused by venous hypertension or ischemia [ ]. The etiology of PMAVFs remains unclear, with potential links to both congenital factors and acquired lesions. These fistulas typically form on the ventral or dorsal surface of the spinal cord at the junction between the spinal artery and medullary vein without an intervening nidus. Although the natural history of PMAVFs is not fully understood, most cases present with hemorrhage or progressive myelopathy and require urgent treatment. Both endovascular and surgical approaches are recognized as therapeutic strategies for PMAVFs, each with advantages and risks. This report describes a unique case of a ruptured cervical PMAVF in a child, managed successfully with endovascular embolization. Additionally, we review relevant literature on the diagnosis, therapeutic management, and outcomes of PMAVFs, focusing on endovascular treatment and pediatric cases.
Case description
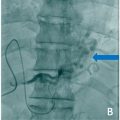
A 10-year-old boy with an unremarkable medical history presented with acute neck pain and fatigue in the morning. By the afternoon, he developed rapidly progressive weakness in his upper limbs, which extended to his lower extremities. Upon arrival at our facility, the patient exhibited significant neurological deterioration, including altered consciousness and respiratory distress, necessitating intubation and transfer to the Pediatric Intensive Care Unit (PICU). Imaging studies revealed extensive findings ( Figs. 1 A-D). A head MRI demonstrated edema in the medulla oblongata and dilated veins in the posterior cranial fossa. A contrast-enhanced CT scan of the neck identified an intramedullary hematoma centered at C4, with extensive edema extending from the medulla oblongata to the thoracic spine (Th3). Additionally, the imaging revealed a contrasted mass in the posterior aspect of the spinal cord at C4, with associated dilated ascending and descending venous drainage pathways ( Figs. 1 E and F). Given the clinical and radiological findings, an urgent spinal angiography was performed under general anesthesia. The angiograms confirmed a diagnosis of PMAVF with feeders from the right C4 dorsal root artery and the right ascending cervical artery ( Figs. 2 A-D). Notably, a ruptured varix was associated with the fistula, contributing to the intramedullary hematoma. The draining vein ascended dorsally from the cervical cord to the posterior fossa, causing intracranial and spinal venous congestion.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree