Abstract
Acute renal infarction is a condition where the blood supply to the kidney is suddenly blocked, leading to tissue damage and potential loss of kidney function. If the patient is not treated promptly, it can lead to severe complications such as permanent kidney damage, acute kidney failure, hypertension and chronic kidney disease. A 52-year-old male patient was admitted to the emergency department with persistent left flank pain within 21 h after onset. A CT scan with contrast of the abdomen showed a renal infarction in the left kidney caused by a clot in the anterior branch of the left renal artery. The patient underwent a thrombectomy and revascularization using the Solumbra technique. After the intervention, the patient’s symptoms significantly improved, and their renal function recovered within 1 month. This result indicates the effectiveness of the Solumbra technique in restoring blood flow in an occluded renal artery, highlighting its potential in managing complex vascular conditions.
Introduction
Acute Renal Infarction (ARI) is a rare but serious condition caused by sudden vascular occlusion, leading to renal parenchymal ischemia. The reported incidence ranges from 0.007% to 1.4% [ ]. Without timely treatment, ARI can result in severe complications such as renovascular hypertension, chronic kidney disease, and end-stage renal failure [ ]. Early diagnosis and prompt intervention are crucial for improving patient prognosis. Traditional treatment approaches, including systemic thrombolysis, surgical thrombectomy, and catheter-directed thrombolysis (CDT), have several limitations, such as a high risk of bleeding, significant invasiveness, and reduced effectiveness beyond 10 hours after symptom onset. In recent years, renal artery thrombectomy has emerged as an effective technique, particularly when performed within 72 hours in symptomatic patients.
Typically, renal artery thrombectomy is performed using large-bore aspiration catheters combined with negative pressure suction to effectively remove the thrombus. However, in cases where thrombi are located in small arterial branches, intervention becomes more challenging due to the small vessel size, tortuous anatomy, and difficulties in navigating the device to the occlusion site. The Solumbra technique, which combines an aspiration catheter with a stent retriever, has demonstrated high efficacy in clot retrieval within small and complex vascular structures, particularly in the treatment of ischemic stroke. This is the first reported case of successful treatment of renal artery thrombectomy using Solumbra technique.
Case report
Patient information
A 52-year-old male patient was admitted to the emergency department with persistent left flank pain, 21 hours after symptom onset. He has a history of heavy smoking (30 pack-years) and chronic gout, currently treated with allopurinol 300 mg/day. The patient has no history of cardiovascular disease or other significant medical conditions. There is no notable family medical history.
Clinical signs
The patient’s blood pressure was 189/100 mmHg, heart rate 103 bpm, with no chest pain or shortness of breath. The abdomen was soft, with left flank tenderness, but no signs of peritoneal irritation or free fluid in the abdominal cavity. Kidney examination showed no enlargement, and urination was normal with clear yellow urine.
Timeline
| Time | Clinical Event |
|---|---|
| 0 h | Onset of left flank pain. |
| 21 h | Admission to the hospital. |
| 22 h | CT scan confirmed a thrombus in the left renal artery. |
| 23 h | First attempt at thrombus aspiration using an Export catheter was unsuccessful. |
| 24 h | Thrombus aspiration initiated with the Solumbra technique. |
| 26 h | Partial recanalization of the renal artery achieved; patient transferred to the cardiology department and commenced on anticoagulants. |
| 3 days | Patient discharged from the hospital. |
| 1 month | Renal function fully restored. |
Diagnosis
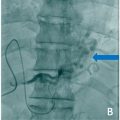
Contrast-enhanced abdominal CT scan results confirmed a left renal infarction caused by a thrombus in the anterior branch of the left renal artery ( Fig. 1 A), establishing the diagnosis at the 21st hour of infarction onset.

Differential diagnoses included renal infarction due to embolism and renal artery dissection; however, both were ruled out based on imaging findings and clinical presentation. The cause of the renal artery thrombus was identified as the patient had no prior history of atrial fibrillation, and thrombus aspiration yielded white plaques from the occlusion site.
Therapeutic intervention
As the patient continued to experience persistent symptoms, we decided to perform emergency revascularization. We established right femoral artery access and performed bilateral renal artery angiography using a JR 4.0 6F catheter (Medtronic, USA). Angiographic imaging confirmed a complete occlusion in the anterior branch ( Fig. 1 B). Initial thrombus aspiration using an Export catheter (Medtronic, USA) was unsuccessful due to the thrombus being located in a distal segment with a tortuous vascular pathway ( Figs. 2 and 3 A and B).