Superficial Femoral Artery Interventions
Ripal T. Gandhi
Jonathan J. Iglesias
James F. Benenati
Technology has rapidly advanced in the last several years, and the endovascular options available to treat superficial femoral artery (SEA) disease have markedly increased. Although percutaneous transluminal (balloon) angioplasty (PTA) was previously considered the initial therapy for treatment of femoropopliteal disease, this therapy is being replaced with bare-metal stents, covered stents, drug-eluting stents, and drug-eluting balloons, which have shown improved patency rates and outcomes. Atherectomy can be performed as an adjunct and may be valuable in
the treatment of in-stent restenosis. As new clinical trials emerge, the precise role of each of these new technologies in the ever-expanding SFA endovascular landscape continues to evolve.
the treatment of in-stent restenosis. As new clinical trials emerge, the precise role of each of these new technologies in the ever-expanding SFA endovascular landscape continues to evolve.
Indications
1. Lifestyle-limiting moderate to severe claudication (Fontaine category IIb, Rutherford stages 2 and 3) in patients who have failed medical management (i.e., cilostazol and/or exercise program)
2. Critical limb ischemia (CLI) characterized by rest pain, nonhealing ulcerations, or gangrene
3. Pre- or post-bypass surgery to increase inflow or outflow
4. Salvage of failing bypass graft with significant flow-limiting stenosis of the anastomosis or outflow vessels
Contraindications
There are no absolute contraindications to endovascular therapy for the SFA. Most of the contraindications listed below are relative.
1. Uncorrectable coagulopathy
2. Severe renal insufficiency (glomerular filtration rate [GFR] <30) in the absence of hemodialysis. Patient should be hydrated, contrast use minimized, and carbon dioxide angiography should be considered.
3. Active phase of vasculitis
4. Nonambulatory critically ill patients with limited life expectancy and/or dementia
5. Patients who have mild claudication symptoms
6. Unfavorable anatomy
a. SFA occlusion with involvement of the popliteal artery and trifurcation vessels
b. Hemodynamically significant common femoral artery (CFA) disease. A combined femoral endarterectomy with endovascular treatment of the SFA or femoropopliteal bypass is recommended. Common femoral angioplasty and/or atherectomy may be considered in patients who are not surgical candidates. Stenting of the CFA is not desirable and may preclude future surgical options.
c. Significant calcification involving a long SFA segment, especially “coral reef” calcification
d. Absent runoff via at least one vessel to the foot
e. Presence of hemodynamically significant inflow disease, which cannot be corrected by endovascular or surgical means
f. Severe aneurysmal disease at intended access site
Preprocedure Preparation
1. Obtain preprocedure physiologic studies with an arterial noninvasive examination with and without exercise (exercise exam not performed in patients with critical limb ischemia) including baseline ankle-brachial index (ABI) values, segmental plethysmography with pulse volume recordings, and toe pressures when appropriate.
a. Preprocedural imaging with computed tomography (CTA) or magnetic resonance angiography (MRA) can be utilized to develop a patient-specific course of treatment. Cross-sectional imaging is valuable in determining access site and to plan the procedure, which may ultimately allow for a safer procedure with reduced contrast and radiation exposure.
2. Preangiography preparation: Verify stable renal function relative to baseline. Emergent or nonpostponable procedures in patients with impaired kidney
function necessitate the use of preventative measures such as aggressive hydration with or without concomitant acetylcysteine. Ascertain allergy history to contrast mediums and treat as needed.
function necessitate the use of preventative measures such as aggressive hydration with or without concomitant acetylcysteine. Ascertain allergy history to contrast mediums and treat as needed.
3. Premedication: All patients should be on antiplatelet therapy with aspirin and/or clopidogrel.
a. Per the Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events (CAPRIE) trial, there was a profound superiority in patients with peripheral arterial disease (PAD) treated with clopidogrel over aspirin in the prevention of stroke, myocardial infarction, and vascular death (1). As a result of this trial, many advocate that clopidogrel be the antiplatelet medication of choice in the PAD population given that the safety profile of this drug is at least as good as aspirin.
b. All patients treated with drug-eluting balloons and drug-eluting stents require dual antiplatelet therapy for a short period of time. Per instructions for use, a minimum duration of dual antiplatelet therapy is 1 month and 2 months for Lutonix drug-eluting balloon (Bard, New Providence, NJ) and Zilver PTX drug-eluting stent (Cook Medical, Bloomington, IN), respectively.
c. In patients who were not previously on antiplatelet mediations, a loading dose of 81 mg of aspirin and 300 mg of clopidogrel can be given at the time of the procedure.
d. Whether all patients should be treated with dual antiplatelet therapy remains controversial and continues to evolve; this decision should be patient-specific, and the risks of vascular occlusion must be balanced with risk of hemorrhage.
Procedure
1. Obtain initial arterial access.
a. A contralateral common femoral approach is the norm for SFA procedures; however, this approach may not be feasible in patients with a steep native aortic bifurcation, prior endovascular aneurysm repair, or aortobifemoral bypass.
b. Ipsilateral antegrade access is advantageous if tibial interventions are also necessary provided the patient’s body habitus and CFA anatomy allow it.
c. If the occlusion involves the origin of the SFA or the very proximal SFA, a contralateral approach is generally required.
d. In patients with proximal SFA occlusion and significant disease in the contralateral CFA, a popliteal or distal SFA access may be considered.
e. At the current time, devices are not of sufficient length to perform mid to distal SFA interventions via an upper extremity brachial or radial access.
f. Tibiopedal arterial puncture may be used in conjunction with antegrade or contralateral common femoral access in recanalizing complex occlusions.
2. Perform initial angiography including distal runoff.
a. Multiple views may be required to establish a vascular map exhibiting the exact location and morphology of some lesions.
b. We generally perform both anteroposterior and lateral views of the foot in patients without renal insufficiency prior to intervention to establish a baseline.
3. Generally, stenoses of more than 50% are considered hemodynamically significant in symptomatic patients.
a. Orthogonal views and correlation with noninvasive imaging and physiologic studies are of paramount importance.
b. Although pressure wires may be utilized to determine the hemodynamic significance of questionable lesions, this is rarely performed in the femoropopliteal segment.
4. Anticoagulation during interventions
a. Patients are generally anticoagulated with either heparin or bivalirudin when performing endovascular intervention to minimize risk of intraprocedural
thrombus. Patients with SFA stenosis are anticoagulated prior to crossing the lesion, whereas patients with chronic occlusions are anticoagulated immediately after successful crossing of lesion.
thrombus. Patients with SFA stenosis are anticoagulated prior to crossing the lesion, whereas patients with chronic occlusions are anticoagulated immediately after successful crossing of lesion.
(1) Typically, a heparin bolus dose of 70 to 100 units per kg is given with approximately 1,000 IU per hour subsequently.
(2) Bivalirudin dosing is as follows: initial bolus of 0.75 mg per kg followed by standard infusion of 1.75 mg/kg/h. Infusion dose is reduced to 1.0 mg/kg/h in patients with renal insufficiency (GFR 10 to 29 mL per minute) and to 0.25 mg/kg/h in patients on dialysis.
b. Activated clotting time >250 seconds is recommended prior to SFA interventions.
c. The unpredictability associated with heparin therapy has popularized the use of direct thrombin inhibitors (bivalirudin) in more extensive lower extremity interventions as these drugs circumvent the pitfalls associated with heparin therapy.
(1) Unlike heparin, bivalirudin cannot be reversed with protamine; however, it does have a short half-life of approximately 25 minutes.
(2) Because bivalirudin is excreted in the urine, it is important to note that its half-life is increased in patients with renal insufficiency. In patients with GFR between 10 and 29, half-life is approximately 57 minutes.
5. Technique for crossing an SFA occlusion
a. Before treatment can be initiated, a guidewire must cross the lesion. In 80% to 85% of SFA occlusions, only a catheter and guidewire are necessary to successfully recanalize the lesion.
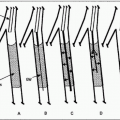
b. Although there are a multitude of guidewires and catheters on the market and every operator has his or her favorites, the technique described here is that preferred by the authors. A.035 system is recommended to cross the majority of SFA occlusions. A.035 Cerebral Newton LLT Guidewire (Cook Medical, Bloomington, IN) in conjunction with a straight or angled catheter is our initial guidewire of choice in crossing SFA occlusions. If this guidewire is not successful in crossing the lesion, hydrophilic guidewires such as an angled GLIDEWIRE (Terumo, Somerset, NJ) or Roadrunner (Cook Medical, Bloomington, IN) are employed. It is desirable to achieve an intraluminal path across the lesion (Fig. 12.1).
c. There are a variety of chronic total occlusion (CTO) crossing devices available on the market; however, there are no randomized clinical studies assessing the safety and efficacy of these devices.
(1) Crossing devices include Viance (Covidien/Medtronic, Mansfield, MA), TruePath (Boston Scientific, Natick, MA), Crosser (Bard, New Providence, NJ), FRONTRUNNER XP (Cordis, East Bridgewater, NJ), Wildcat (Avinger, Redwood City, CA), and Ocelot (Avinger, Redwood City, CA). The latter device utilizes optimal coherence tomography to help direct the device and achieve intraluminal crossing.
(2) Most of the crossing devices require that an occlusion has not been previously manipulated with a catheter and guidewire as the devices have a tendency to follow the same path created by the guidewire.
(3) Because the majority of femoropopliteal occlusions can be crossed successfully with a guidewire and catheter and there is an up-front cost to utilizing CTO devices, we generally do not utilize these devices. A study comparing conventional guidewire techniques to CTO devices, focusing on end points including crossing success, cost, time to recanalization, need for re-entry, and complications would be valuable.
d. If the lesion cannot be crossed intraluminally, a subintimal approach (Bolia technique) will be used.
(1) A guidewire loop (typically with a hydrophilic.035 guidewire) is formed and advanced subintimally with a catheter until reaching or opposite
a patent arterial segment. It is important to limit the extension of the subintimal dissection beyond the occlusion because this may result in loss of important collaterals.
a patent arterial segment. It is important to limit the extension of the subintimal dissection beyond the occlusion because this may result in loss of important collaterals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree