Interventional Radiology is at the forefront of integrating advanced imaging techniques and minimally-invasive procedures to enhance patient care. The advent of Digital Health Technologies (DHTs), including artificial intelligence (AI), robotics, and extended reality (XR), is revolutionizing healthcare, particularly in IR due to its reliance on innovative technology and advanced imaging. Since 2016, the proportion of these DHT-related publications in IR has consistently increased. The proportion of AI-related studies published in IR was 69% higher than in surgery, XR-related studies were 94% higher, and robotics studies were 192% higher, indicating a more rapid growth rate in IR compared to surgery. This article explores the transformative impact of these technologies on IR, emphasizing their potential to enhance precision, efficiency, and patient outcomes. Despite the promising advancements, there is a lack of standardization and clinical consensus on the optimal use of DHTs in IR. The variability in IR procedures and imaging systems across hospitals complicates the standardization of workflows and comparison of studies. This underscores the importance of integrating DHTs as aids to IR practitioners rather than replacement, ensuring that these technologies enhance both clinical and procedural practice.
Introduction
Interventional Radiology (IR) centers on the intersection of advanced imaging techniques, cutting-edge procedures, and minimally-invasive approaches to enhance patient care. Digital health technologies (DHTs), including artificial intelligence (AI), robotics, extended reality (XR), informatics, and telehealth are revolutionizing healthcare. These advancements are poised to impact the field of IR in particular, due to its innate focus on advanced imaging and technical precision.
This article concentrates on 3 pivotal DHTs due to their direct relevance to IR:
- –
Artificial Intelligence : AI is transforming healthcare by improving most aspects of patient care including diagnostic accuracy, predicting outcomes, and personalizing treatment plans.
- –
Extended Reality : XR technologies are enhancing medical training, surgical planning, and patient care through immersive and interactive experiences.
- –
Robotics : Robotic systems are increasingly utilized in surgeries to improve precision, reduce invasiveness, and decrease recovery times.
The emergence and increased accessibility of DHTs suggest that the future of IR will ubiquitously utilize AI or XR-based technologies throughout the clinical workflow. This has raised concern regarding the role of IRs. , However, while there is significant potential for the use of DHT in IR, the current literature consists primarily of case studies and proof-of-concept research. The overall lack of standardization in DHT research underscores the continued need for human interventionalists who can adapt quickly to varying clinical scenarios and demonstrates that the focus should be placed on the integration of DHTs, rather than automation.
This literature review and analysis examines the transformative impact of integrating DHTs into clinical practice. It explores current trends, general applications, and the potential of these technologies to enhance precision, efficiency, and patient outcomes.
Publication trends in IR versus surgery
Methods: Data for this analysis were extracted from the Web of Science, a comprehensive database of research publications. Data were collected from 2005 to 2024, concentrating on publications within IR and Surgery. AI-related articles were identified through a collated search of the terms “artificial intelligence,” “machine learning,” “deep learning,” “neural network,” and “ChatGPT.” Similarly, XR-related articles were obtained using the terms “mixed reality,” “augmented reality,” “extended reality,” and “virtual reality.” For every year, we collected the number of publications for each topic in IR and Surgery. We then calculated the proportion of these topic-related publications relative to the annual number of publications in IR and Surgery, respectively. This standardization allowed for a direct comparison between IR and Surgery despite a much larger number of publications in the latter. This approach provides a comprehensive overview of the trends and highlights the growing impact of these technologies in IR practices.
Findings: Historical data from this database indicate that publications on robotics and XR in IR began in the 1990s, while AI in IR appeared around 2016. The year 2016 marked an unprecedented milestone when AI defeated the world champion in Go, a game even more complex than chess. This achievement catalyzed widespread public interest in AI. Since then, there has been an increase in the proportion of AI, XR, and robotics publications in IR and surgery ( Figs. 1 and 2 ).


For 2 decades, the proportion of XR and robotics studies in IR remained nearly constant ( Fig. 1 A). But since 2016, they have shown linear and nearly-exponential growth rates, respectively. During the early COVID-19 era in 2020, ChatGPT captivated public attention and heightened interest in AI. Consequently, this second surge likely contributed to complementary growth in robotics and XR given their strong intersection with AI ( Fig. 3 ). In IR, AI has shown the fastest growth rate among subgroups, with exponential growth and the highest proportion of published studies since 2019. This growth is likely tied to the direct applicability of machine learning and radiomics in imaging-related aspects of IR including enhanced diagnosis, prognosis, and pre-procedural planning ( Fig. 4 ).


Meanwhile, surgery has also seen exponential growth in the proportion of AI studies published. However, XR and robotic publications in Surgery have grown linearly at the slowest rates among all subgroups over the past 2 decades ( Fig. 1 B). Comparing publication rates between IR and surgery since 2016, the following is observed:
- –
The proportion of AI-related studies published in IR was 69% higher than in surgery, with both fields demonstrating exponential growth ( Fig. 2 B).
- –
XR-related studies published in IR were 94% higher compared to surgery, although both only increased at linear rates ( Fig. 2 C).
- –
Similarly, the proportion of robotics studies in IR was 192% higher compared to surgery, with a more rapid growth rate in IR ( Fig. 2 D).
While growth rates of robotics and AI in IR are expected to eventually plateau, these trends suggest that the percentage of publications will continue to increase during the next decade. This growth will lead to new use-cases that will transform many daily functions of interventionalists.
Extended reality
XR encompasses the technologies of augmented reality (AR), virtual reality (VR), and mixed reality (MR). VR creates a fully immersive and interactive digital environment, while AR overlays 2D/3D images onto real-world structures. MR extends the capabilities of AR by enabling users to interact with digital objects within the physical world. Advancements in IR are driven by new imaging techniques and their innovative use in guiding minimally invasive procedures. As such, IR is uniquely positioned to integrate XR technology into standard clinical practice. The potential applications of XR in IR are vast, ranging from skills-acquisition programs for trainees, pre-procedural planning, and intra-procedural feedback, to workflow improvements.
XR-enhanced training: Medical trainees gain procedural experience by practicing skills on physical phantoms, cadavers, or living patients. The use of XR for skills-based training creates realistic and risk-free learning opportunities, as inexperienced providers are associated with increased patient discomfort and morbidity. Many training programs have been developed using XR to learn anatomy, resulting in improved spatial awareness, 3D understanding, and recall. XR-based training for skills acquisition has been shown to reduce training duration, flatten learning curves, improve trainee confidence, and increase procedural accuracy. One example of this phenomenon includes VR-based training for percutaneous nephrostomy, which decreased fluoroscopic time, puncture attempts, and vascular injury. In a study in which trainees used a 3D spine model to practice fluoroscopy-guided lumbar punctures, all users found the training realistic and effective. A systematic review of the use of XR in IR training demonstrated that most programs improved the acquisition of procedural skills, however, 1 study found that VR training increased the procedure time. , XR can also aid experienced physicians, allowing IRs to practice with new equipment or refine skills in highly complex procedures without introducing additional patient risk.
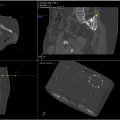
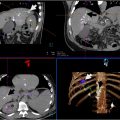
Pre-procedure improvements: Using XR, IRs can reconstruct prior imaging into 3D holograms, allowing them to gain a better depth understanding and immersively view complex anatomy, such as within the liver or vascular trees. This can be used for pre-planning and individualizing their approach. XR has been used to accurately identify ideal fluoroscopy angles, select optimal vessels for catheterization, and map target structures. Additionally, it helps IRs visualize ablation locations for optimal probe placement, increasing the amount of tumor ablated and reducing damage to nearby structures. This improvement is possible since XR removes the physical limitations of patient positioning, such that patient anatomy can be examined from any angle. Pre-planning using XR has improved CT-guided liver biopsies, resulting in less radiation, less indwelling needle time, and fewer manipulations of the needle.
Intra-procedure improvements: The intraoperative use of XR involves 2D/3D or fusion image reconstructions as an intraprocedural reference. These can be projected directly onto the procedural table, or via head-mount displays so IRs can obtain real-time guidance while being scrubbed in. This approach is effective, and a study of AR-enhanced percutaneous vertebroplasty found a 100% clinical success rate. XR-guided percutaneous procedures demonstrate high accuracy and decreased morbidity. Multiple reviews found that XR-enhancement decreased IR procedure time and radiation exposure, and 1 further concluded that live-tracking is accurate to 5 mm in live patients. , Another study found that when a head-mount was used for intraprocedural holographic guidance during percutaneous tumor, the difference between planned AR coordinates and physical anatomic markers was 3.3 mm. Additionally, intraoperative XR guidance was widely found to reduce radiation exposure to both the patient and staff in the IR suite. , ,
While the integration of XR into training, procedure planning, and intraoperative execution is highly promising, there is limited data on this topic. The majority of the literature consists of case studies, proof-of-concept studies, or other small-scale reports. Additionally, there is a lack of standardization in integrating VR into procedures across the literature. ,
Artificial intelligence
AI simulates human intelligence in machines, encompassing technologies like machine learning (ML), neural networks (NNs), and large language models (LLMs). ML uses algorithms to learn from data and make predictions. NNs mimic the brain’s structure to recognize patterns and analyze complex data and are widely used in radiomics to extract quantitative features from medical imaging. LLMs, such as ChatGPT, leverage complex NNs designed for natural language understanding and generation.
The emergence of accessible AI programs has led to increased integration of adaptive technologies into clinical practice. Over the past decade, AI-related publications in IR have seen the most significant growth among DHTs ( Figs. 1 and 2 ). Our analysis estimates that 1-quarter of these publications were general overviews of applying AI in various aspects of IR practice ( Fig. 4 ). The next most common publication types were proof-of-concept studies focused on pre-procedural and intra-procedural applications. These works suggest that AI can enhance IR by improving diagnosis, creating customized treatment plans, and providing real-time procedural support.
Pre-procedure uses: Automating time and labor-intensive tasks using AI reduces the burden on IRs and improves workflow efficiency. For example, AI can be used to rapidly screen the EMR for procedure contraindications. Further, AI significantly reduces the time needed for image segmentation with accuracy equal to a board-certified radiologist in some cases. Indeed, we estimate 38% of publications discuss the use of radiomics in some capacity to increase the accuracy of diagnostician and prognostication ( Figs. 3 and 4 ). AI can also be used to streamline pre-charting and documentation. LLMs can aggregate and summarize large amounts of text, similar to medical scribes, or aid radiologists in more rapidly assessing the EMR. Additionally, text-prediction programs such as ChatGPT have advanced communication abilities and can interact with patients to provide information regarding procedures, schedule appointments, and answer questions in accessible language.
Intra-procedure uses: Intraprocedural feedback with AI can guide radiologists in real-time, improving patient outcomes. It has been found that the use of ML algorithms to optimize probe placement during ablations increases the amount of tumor removed and decreases damage to healthy tissues. Another study found that AI-based image fusion improved tumor visualization and subsequent localization.
Post-procedure uses: Studies have shown that AI is effective for post-procedure prognostication across many pathologies. One study developed a deep learning model using CT images to accurately predict the response of hepatocellular carcinoma to chemoembolization with 85% accuracy. , It has also been successfully studied for prognostication after uterine fibroid treatment, earlier detection of complications following endovascular abdominal aortic aneurysm repair, and survivability of patients with adrenal metastases using CT radiomics.
Robotics
The concept of robotics in medical procedures emerged in the 1980s with the introduction of the PUMA 560 robotic system for stereotactic neurosurgical biopsies and was later popularized by the Da Vinci Surgical System in urology and general surgery. Initially developed for endovascular procedures in Cardiology, these robotic systems have been adapted for IR. Robotic systems like CorPath GRX enable remote control during peripheral vascular interventions, improving accuracy and reducing radiation exposure. Another system, the Magellan robot is particularly beneficial for complex endovascular interventions and provides enhanced stability and catheter control.
Robotics-enhance training: Training programs for robotic systems in IR typically include simulation tools and hands-on workshops, providing physicians with experience in system operation, troubleshooting, and maintenance. A primary focus is the development of technical skills, particularly in mastering catheter control and adhering to ALARA protocols, minimizing radiation exposure for both patients and practitioners during robotic procedures.
Intra-procedure uses: Benefits of robotics in IR include enhancing precision in catheter placement for embolization, standardizing procedures, decreasing operator variability, improving technical outcomes, and alleviating operator fatigue and strain. Techniques like fluoroscopy expose providers to higher radiation levels; robotic assistance helps mitigate this risk by guiding needle placement while significantly lowering exposure. The Magellan robot, for example, improved needle placement precision and reduced physician radiation exposure by approximately 80% in chemoembolization cases. A multicentric clinical trial of the R-One robotic system demonstrated similar exposure reduction while maintaining a 95% technical success rate.
Per-procedure uses: Notable integrations include hybrid imaging that combine modalities like CT and ultrasound to improve visualization and targeting, particularly for difficult-to-access tumors. Further advancements in AI integration aid in intraprocedural and peri-procedural decision-making by analyzing imaging data to define ablation zones and predict patient responses. Furthermore, these systems can be operated remotely, enabling patients in rural or underserved areas to receive advanced care without seeking specialized centers.
Challenges: Technical issues such as potential malfunctions can disrupt procedures and pose risks to patients. The complexity of setting up and operating these systems requires specialized training, leading to longer preparation time and potential workflow disruptions. Additionally, the lack of haptic feedback in current systems makes it difficult to gauge the force applied during procedures, increasing the risk of injury.
Conclusion
Cutting-edge imaging techniques and enhanced precision are central to advancement in the field of IR. As such, IR is uniquely positioned to be revolutionized by integration with DHTs, as evidenced by its greater growth compared to surgery. The use of DHTs in medical training has become commonplace over the past 5 years, and there are many pilot programs utilizing XR and AI to help trainees acquire or hone procedural skills. The literature also demonstrates that the use of DHT in both pre-procedural planning and intra-procedural optimization is safe, effective, and improves outcomes. Finally, the use of DHT in the IR suite has been shown to improve ergonomics and streamline workflows.
Despite its vast potential, there is a lack of standardization and clinical consensus regarding how best to use DHT in the practice of IR. This lack of standardization in the literature is due to 2 phenomena. First, IR procedures have an innate degree of variability in approach. Even commonplace procedures in IR are complicated by individual patient features such as challenging anatomy, body habitus, or challenges with patient movements and respirations. Second, a significant degree of IR literature is composed of case studies. Innately complex procedures do not have significant amounts of published data. Further, there is variability in imaging systems and protocols across hospitals, making it difficult to standardize workflow and compare studies.
This lack of standardization introduces challenges when it comes to advancing and integrating DHTs in IR. There is insufficient data to train DHT programs to the degree of full automation. Instead of automation, there should be a focus on integrating DHTs as valuable aids alongside IRs, enhancing both clinical and procedural practice.
Declaration of competing interest
All authors declare that they have no conflicts of interest that pertain to this submission.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree