Abstract
Objective
To analyze Necrotic Area Features of subpleural pulmonary lesions (SPLs) demonstrated by contrast-enhanced ultrasound (CEUS) and investigate their value in differentiating between malignant and benign SPLs.
Methods
Patients with SPLs who underwent CEUS at our hospital from January to May 2021. The following patient information was recorded: (i) age, (ii) sex, (iii) lesion size, (iv) lesion location, (v) size of necrotic areas and (vi) necrotic area morphology, including sieve-like necrosis, necrotic area with septal enhancement, necrotic area with annular enhancement margins, and necrotic area with burr-like enhancement margins. These parameters were analyzed using univariate and multivariate logistic regression. Subgroup analyses based on lesion size were further conducted using the collected data.
Results
A total of 212 patients with 212 SPLs were enrolled, comprising 99 benign and 113 malignant cases. Significant differences were observed between malignant and benign groups in terms of age, sex, lesion size and necrotic area morphology (all, p < 0.05).
Conclusion
Necrotic area’s features observed on CEUS were valuable for distinguishing between benign and malignant SPLs. Age, sex, lesion size and the presence of burr-like enhancement margins are identified as independent predictors of malignant lesions.
Introduction
It remains challenging to differentiate between benign and malignant lung lesions, and CT remains the principal diagnostic approach [ ]. With the extensive application of contrast-enhanced ultrasound (CEUS), its diagnostic value in lung diseases has been reported in numerous literatures, making CEUS a significant supplement in the diagnosis of benign and malignant lung diseases [ ].
As a novel diagnostic method, CEUS possesses its distinctive characteristics: real-time dynamic display of microcirculation. Numerous literatures have investigated the quantitative and qualitative indicators of CEUS [ ]. In our previous research, we found that Quantitative indicators such as the ultrasonic contrast agent arrival time difference ratio (ATDR) were used in the differential diagnosis of benign and malignant. The accuracy was greater than 90% [ ], which outperformed other research results [ , ].
Previous studies only focused on the puncture to avoid the necrotic area, rather than observing the difference between benign and malignant lesions, so we conducted this study to clarify the value of the characteristics of the necrotic area in the diagnosis of lung cancer [ , ].
The necrotic area reflects the damage degree of the blood supply and blood vessels inside the lesion, which holds a certain value in the differentiation of benign and malignant. More studies have confirmed that the pathological changes of the lesions constitute the basis of imaging performance, and the necrotic features of the lesions often reflect their unique pathological properties [ , ]. Nevertheless, previous studies have merely focused on avoiding necrotic areas through puncture rather than observing the differences in necrotic areas between benign and malignant lesions [ , ]; thus, we conducted this study to clarify the value of necrotic area features in the diagnosis of lung cancer.
Methods
Study population
We retrospectively collected patients with subpleural pulmonary lesions (SPLs) who underwent CEUS at our hospital from January to May 2021 and were confirmed to have necrosis by CEUS. The necrotic area should refer to the area where the whole ultrasound contrast process is not enhanced, and the attention time is the whole process.
Inclusion criteria: (i) the lung lesion was subpleural and could be clearly visualized by ultrasound; (ii) CEUS demonstrated necrosis within the lesion; (iii) The clips of CEUS images are stored, including the enhancement period, peak period and regression period, and the duration is not less than 120 s.
Exclusion criteria: (i) ultrasound images of the lesion were obscured by gas or bone artifacts; (ii) lack of a definitive final diagnosis; (iii) the lesion had undergone an invasive examination within 1 wk before CEUS, (iv) the patient had an allergy to the ultrasound contrast agent.
This study was approved by the Institutional Review Board (No. K18-197Y), and all patients provided informed consent for the CEUS examination. Due to the retrospective design of this study, the requirement for informed consent for patient participation in clinical research was waived.
Instruments, examination method
Patients with SPLs at our institution underwent a standardized procedure. Using the LOGIQ E9 diagnostic ultrasound equipment (GE Healthcare, Milwaukee, WI, USA) and a 3.5–5 MHz convex array probe for ultrasound examinations. The focus is located in the mid-lower 1/3 region of the lesion. The conventional ultrasound frame frequency is not less than 40; patients were positioned appropriately to ensure full exposure of the lesion. If there were multiple lesions in the same patient, priority was given to selecting the largest volume lesion with the clearest ultrasound image. During B-mode ultrasound, the probe was positioned parallel to the intercostal space and perpendicular to the skin to identify the most significant section of the lesion as the target area. Lesions were categorized based on their maximum diameter, with those <3 cm classified as small, and≥3 cm as large [ ]. We selected the best acoustic window to fully display the lesions and surrounding tissue. Probe movement was avoided, and the equipment was then switched to low mechanical index (MI ≤ 0.1) CEUS mode, and the gain was adjusted to display only the surface of air-filled lungs (20 dB). The CEUS frame frequency is not less than 9. Then, 2.4 mL of ultrasound contrast agent (SoneVue, Bracco company, Italy) was injected into the median cubital vein as a 2 s bolus via a 20-gauge needle, followed by a rapid injection of 5 mL of saline, while recording clips continuously for 3 min. The lesion area that was consistently free of CEUS enhancement from the onset of enhancement to fading was defined as the necrotic area, and a frame when the enhancement of the lesion peaked was selected as a representative image.
Image analysis
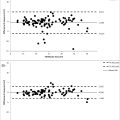
Two radiologists (Y.C., Y.Z.), each with over 5 y of experience in pulmonary ultrasound, visually analyzed the CEUS image segments to identify specific characteristics of necrotic areas: (i) necrotic area size, categorized as small necrotic areas (necrotic area/lesion area ≤20%), medium necrotic areas (necrotic area/lesion area between 20% and 50%), large necrotic areas (necrotic area/lesion area >50%); (ii) morphological features of necrotic areas, including (a) sieve-like necrosis, (b) necrotic area with septal enhancement, (c) necrotic area with annular enhancement margins, (d) necrotic area with burr-like enhancement margins. The pattern diagrams illustrating these necrotic area features are displayed in Figure 1 . In cases where the two radiologists did not reach an agreement, a third radiologist (Y.W.) with more than 8 y of experience in pulmonary ultrasound was consulted to achieve consensus through discussion. All radiologists underwent standardized training before this study and were blinded to all clinical information except for the lesion location.

Pathological diagnosis
Tissue specimens were obtained from all lesions by puncture or surgery, fixed in 10% formalin, and examined for histopathology. All tissues were paraffin-embedded and sectioned. Staining was done with hematoxylin and eosin. Further immunohistochemical examination was performed to clarify the pathologic subtype if malignancy was suspected or diagnosed. Benign lesions were defined as (i) lesions with histopathologic findings that were benign, (ii) lesions with histopathologic findings that showed nonmalignancy and disappeared or shrunk with or without anti-infective, antituberculosis or antifungal therapy or those that remained unchanged in size during 2 y of follow-up.
Statistical processing
Statistical analyses were performed using SPSS statistical software version 22.0 (IBM, Chicago, IL, USA). Continuous variables were reported as mean ± standard deviation, and statistically analyzed using t -tests. Categorical variables were reported as numbers and percentages, Pearson’s chi-squared test, Fisher’s exact test or Kruskal–Wallis H test was used to compare whether there was a difference between groups. The Bonferroni method was used for multiple comparisons. The significance level for all statistical analyses was set at p < 0.05. Logistic regression analysis was used to screen the characteristics of malignant lesions ( p < 0.05). Screened variables were used as input variables for multivariate logistic regression analysis using the backward stepwise method ( p < 0.1), to identify independent predictors of malignant lesions.
Results
Patient characteristics and US findings
A total of 228 patients were enrolled in this study, of which 16 of these cases were excluded for the following reasons: Ten of these cases, who had undergone an invasive examination within 1 wk before CEUS, four of these cases did not obtain a final diagnosis, and in two cases, the ultrasonographic images of the lesions were interfered with by artifacts of gas or bone. Finally, 212 patients were included in the study, of which 161 (75.94%) were male and 51 (24.06%) were female, and of the 212 lesions, 99 (46.7%) were benign and 103 (53.3%) were malignant. The pattern of no perfusion zone (necrotic zone) is shown in Figure 1 and patient enrollment procedures are shown in Figure 2 . Patient Characteristics are presented in Table 1 .

| Variables | Total | Malignant Group | Benign Group | X 2 / t Value | p Value |
|---|---|---|---|---|---|
| No. of participants | 216 | 113 (53.3) | 99 (46.7) | ||
| Age (y x ± s ) | 59.95 ± 15.38 | 65.37 ± 11.08 | 53.77 ± 17.22 | 5.744 | <0.001 |
| Gender | 10.758 | 0.01 | |||
| Male | 161 (75.94) | 96 (84.96) | 65 (65.66) | ||
| Female | 51 (24.06) | 17 (15.04) | 34 (34.34) | ||
| Lesion size (cm) | 4.66 ± 2.43 | 5.51 ± 2.38 | 3.69 ± 2.11 | 5.863 | <0.001 |
| Tumor location | 7.887 | 0.096 | |||
| Right upper lobe | 52 (24.53) | 28 (24.78) | 24 (24.24) | ||
| Right middle lobe | 23 (10.85) | 8 (7.08) | 15 (15.15) | ||
| Right lower lobe | 50 (23.58) | 24 (21.24) | 26 (26.26) | ||
| Left upper lobe | 52 (24.53) | 35 (30.97) | 17 (17.17) | ||
| left lower lobe | 35 (16.51) | 18 (15.93) | 17 (17.17) | ||
| Necrotic areas | 0.049 | 0.477 | |||
| Small area | 40 (18.87) | 21 (18.58) | 19 (19.19) | ||
| Moderate area | 64 (30.19) | 38 (33.63) | 26 (26.26) | ||
| Large area | 108 (50.94) | 54 (47.79) | 54 (54.55) | ||
| Perfusion pattern of nonenhancing area | 45.703 | <0.001 a | |||
| Perforation enhancement seen in necrotic areas | 34 (16.04) | 18 (15.93) | 16 (16.16) | ||
| Sieve-like necrosis | 40 (18.87) | 10 (8.85) | 30 (30.3) | ||
| Necrotic areas with annular enhancement margins | 29 (13.68) | 5 (4.42) | 24 (24.24) | ||
| AT | 10.36 ± 3.79 | 11.1 ± 4.02 | 9.51 ± 3.32 | 3.136 | 0.002 |
| TTP | 22.85 ± 9.01 | 23.68 ± 9.2 | 21.91 ± 8.72 | 1.433 | 0.153 |
| Necrotic areas with burr-like enhanced margins | 109 (51.42) | 80 (70.8) | 29 (29.29) | ||
| Definitive diagnosis | Squamous carcinoma 52 (46.02) | Pneumonia 48 (48.48) | |||
| Adenocarcinoma 44 (38.94) | Tuberculosis 47 (47.47) | ||||
| Small cell carcinoma 9 (7.96) | Abscess 1 (1.01) | ||||
| Lymphoma 1 (0.88) | Fungal infections 1 (1.01) | ||||
| Malignant mesothelioma 1 (0.88) | Isolated fibrous tumor 2 (2.02) | ||||
| Нуро-differentiated carcinoma 4 (3.54) | |||||
| Malignant nerve sheath tumor 1 (0.88) | |||||
| Uncategorized neuroendocrine tumor 1 (0.88) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree