The Whitaker Test
David W. Hunter
The Whitaker test is used to differentiate residual or recurrent upper renal collecting system obstruction from dilatation secondary to permanent changes in musculature, when other less invasive imaging tests are equivocal (1). It remains a useful test today, particularly in the evaluation of renal obstruction following percutaneous or surgical intervention, often in transplant kidneys. Adaption of a similar concept to the biliary system for the evaluation of benign strictures expands its role (2).
Urinary Whitaker—Ureteral Perfusion Challenge
The Whitaker test involves an injection of dilute contrast into the collecting system, combined with intermittent measurement of pressures in the bladder and collecting system. An increase of pressure in the collecting system to a value greater than 15 cm of water above the bladder pressure indicates obstruction. The site of the obstruction can usually be determined by careful fluoroscopic analysis. An increase of pressure in the bladder that is transmitted to the collecting system indicates reflux, and the degree of elevation is a rough measure of lack of bladder compliance.
Indications
1. A patient with a dilated collecting system, dilated ureter, or both in whom it is unclear if there is an obstruction or in whom the location, anatomy, and severity of the obstruction has not been adequately defined
2. A patient with a percutaneous nephrostomy catheter in place after stricture dilation and for whom a determination needs to be made whether the stricture is resolved and the nephrostomy tube can be removed
Contraindications
1. Uncorrectable coagulopathy if a new puncture into the collecting system is required
2. Urinary tract infection—untreated or unresponsive to treatment
Preprocedure Preparation
1. Urinary obstruction is first evaluated by one or more noninvasive tests including ultrasound, computed tomography (CT), and a diuresis renogram. In children in whom vesicoureteral reflux may be present, a voiding cystogram should be performed prior to the Whitaker procedure.
2. Obtain informed consent.
3. Testing in adults can be performed with conscious sedation. Pediatric patients may require general anesthesia. Follow institutional guidelines in preparation for sedation and anesthesia.
Procedure
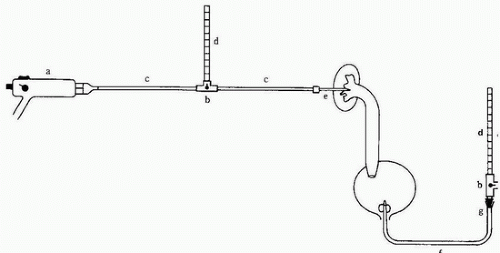
1. Set up the pressure measurement equipment as demonstrated in Figure e-88.1 (3). Measurements are faster and easier when made with two channel hemodynamic
monitoring equipment rather than manometers. For pressure conversion, 1 cm H2O = 0.736 mm Hg.
monitoring equipment rather than manometers. For pressure conversion, 1 cm H2O = 0.736 mm Hg.
2. Establish intravenous (IV) access for the administration of sedation if needed.
3. Using sterile technique, place a catheter into the urinary bladder and empty it. An appropriately sized Foley balloon catheter (10 to 16 Fr.) can be used in an adult or older child, and a pediatric feeding tube can be used in an infant. After the bladder is empty and the study is ready to begin, the end of the bladder catheter is connected to a manometer or pressure transducer through a threeway stopcock, which can be used to empty the bladder if needed.
4. Place the patient prone to establish access to the renal collecting system. There are three methods that can be used to perfuse and monitor pressures in the collecting system.
a. A single 22-gauge needle, or the 3 Fr. catheter from a triaxial set in which 3 to 4 extra side holes have been created near the tip, is placed in the collecting system. The needle tip should not touch the wall. Smooth rise and fall of the pressure tracing with breathing is a good indicator that the needle tip is free in the collecting system. A three-way stopcock is attached to the hub of the needle with one channel attached to the infusion pump and one to the pressure-measuring device. Every 2 minutes, the infusion is interrupted by rotation of the stopcock to allow a pressure measurement.
b. Two 22-gauge needles, or a double-lumen needle or catheter, are placed within the renal collecting system. One lumen is used to measure pressures and the other is used for a continuous, uninterrupted infusion.
c. In patients with a nephrostomy tube, the tube can be used in the same manner as a single needle system.
5. Position the transducers or manometers so that the “0” point is at the level of the collecting system for the renal monitor and the level of the bladder for the bladder monitor.
6. Record the resting (empty) bladder and collecting system pressures, which are normally below 10 cm of water (7 mm Hg) and should be roughly equal.
7. Begin the infusion of dilute contrast (contrast:saline ratio, 1:2 or 1:3) at 10 mL per minute in adults or older children and 5 mL per minute in infants and children less than 5 years of age. The infusion requires an infusion pump.