Thoracic Duct Embolization for Chylothorax
Mikhail C.S.S. Higgins
Maxim Itkin
Chylous leaks are the leakage of intestinal lymph (chyle) from the lymphatic system. They may occur at any point along the course of chyle transit, beginning in the intestinal lymphatic ducts, through the cisterna chyli (CC) and finally within the thoracic duct (TD) (Fig. 48.1). Primary thoracic manifestations include chylothorax and chylopericardium. Injury of the branches of the TD during neck surgery can result in chylous leak from the surgical wound.
Chylous leaks may be traumatic or, less commonly, nontraumatic in etiology. Traumatic causes include iatrogenic injury of the TD or its branches during thoracic, cardiac, or neck surgery and secondary to blunt or penetrating chest trauma.
Nontraumatic causes include idiopathic, malignancy (e.g., lymphoma), congenital, lymphatic vessel disease (e.g., Gorham disease, lymphangiomyomatosis), systemic diseases (e.g., sarcoidosis, systemic lupus erythematosus, and Behçet disease), and infection (e.g., tuberculosis) (1). In cases of nontraumatic chylothorax, the anatomic cause of the chylous leaks can be occlusion of the TD, presence of lymphatic malformations, and chylous ascites. In chylous ascites, chylothorax is a result of migration of the lymphatic fluid through diaphragmatic fenestrations due to negative pressure in the chest cavity.
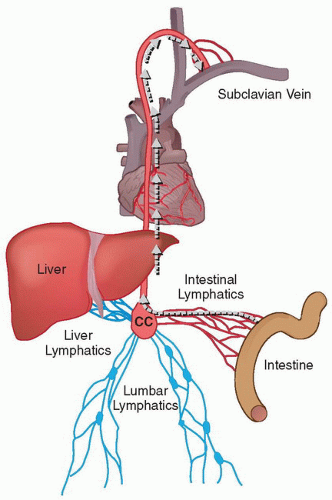 FIGURE 48.1 • Schematic representation of the chyle path (arrows). Chylous fluid originates in the intestinal lymphatics and then it passes through intestinal lymphatic vessels into the CC and then in the TD. Interruption of this flow can result in chylous effusions (chylous ascites, chylothorax, chylopericardium, etc.). In rare cases, this path can be altered (lymphatic malformations) and the chyle can be redirected outside the usual path, for example, into the perineum or lower extremities. |
Thoracic duct embolization (TDE) is a percutaneous, image-guided, minimally invasive alternative to surgical interventions for treating chylous leaks above the diaphragm. This technique comprises two steps: first, the lymphangiogram followed by transabdominal access and embolization of the TD. A lymphangiogram is performed in order to visualize the access point into the lymphatic system and the location of the chylous leak. Compared to the “blind” surgical method, visualization of the leak and lymphatic anatomy significantly improves the outcome (2).
Indications
In the setting of failed initial conservative management
1. Lifestyle-altering chylothorax
2. Chylopericardium
3. Chyle leak post neck surgery
Initial conservative management includes treatment of the underlying disease (e.g., lymphoma), repeated thoracentesis, and dietary modification.
Contraindications
Absolute
1. Uncorrectable coagulopathy
Relative
1. Pregnancy
2. Prior severe anaphylactic reaction to iodinated contrast media
Preprocedure Preparation
1. History and physical exam should be conducted with an emphasis on the lymphatic system and assessment for prior thoracic trauma or intervention.
a. An assessment of American Society of Anesthesiologists’ (ASA) classification for conscious sedation should be performed.
b. Contrast allergy and reaction should be carefully documented with appropriate preprocedural treatment prescribed.
2. Laboratory analysis of the fluid is performed.
a. Chylothorax is assessed for a significantly elevated triglycerides level in patients on a regular diet. In patients on a fat-free diet or nil per os (NPO), the triglycerides level can be low (3).
b. In addition, the lymphatic fluid is assessed for a significant level of lymphocytes in the cell differential (more than 60%) (4).
c. Presence of chylomicrons is diagnostic for chyle unless the fluid contains blood.
3. Obtain informed consent with comprehensive discussion of possible complications.
4. Imaging
a. In cases of nontraumatic chylothorax, heavily T2-weighted magnetic resonance imaging (MRI) of the chest and abdomen is initially performed (5). The goal is to exclude ascites and lymphatic malformations as well as to define the anatomy of the TD.
(1) If noninvasive imaging demonstrates free fluid in the abdomen, chylous ascites with chyle transmigration into the chest through diaphragmatic fenestrations should be suspected. Abdominal fluid sampling and analysis for chyle is advised.
(2) If lymphatic malformation is identified on the MRI, and TD is found to be patent on conventional lymphangiogram, TDE should not be attempted. Instead, sclerotherapy or direct injection of the lymphatic malformation with embolization performed.
5. Coagulation profile should be within acceptable limits—international normalized ratio (INR) <1.5. In case of coagulopathy, blood products are administered to correct coagulopathy.
6. Conscious sedation is managed by nursing staff with incremental administration of midazolam and fentanyl.
a. Oral intake should be appropriately restricted for at least 6 hours preprocedure with the exception of normal medications taken with a sip of water.
b. For insulin-dependent diabetics fasting preprocedure, morning insulin doses should be halved.






