Abstract
Thoracic SMARCA4 -deficient undifferentiated tumor ( SMARCA4 -UT) is characterized by an undifferentiated rhabdoid morphology and SMARCA4 deficiency pathologically. In the 2021 revision of the WHO classification, it was categorized as an epithelial tumor because of its shared genetic background with smoking-related lung cancer.
We describe the case of a 44-year-old man with a rapidly enlarging mediastinal mass observed on chest radiography and CT. The tumor was resistant to radiation therapy, chemotherapy, and immune checkpoint inhibitors, and the patient’s survival time was approximately 5 months. Familiarity with the clinical background and imaging findings of thoracic SMARCA4 -UT is crucial for early diagnosis and treatment planning.
Introduction
Thoracic SMARCA4 -UT is a rare disease first reported by Le Loarer et al. [ ]. It is considered a disease that predominantly affects young male heavy smokers. Compared with typical lung cancer, it progresses extremely rapidly and is often associated with multiple metastases at the time of diagnosis. Approximately 100 cases of SMARCA4 -UT have been reported to date. Although there is a paucity of imaging-focused reports, it is frequently described as a large invasive tumor with intense FDG uptake, involving the superior/middle mediastinum, hilum, lung, or pleura [ ].
Herein we report the case of a 44-year-old man with a rapidly enlarging mediastinal tumor.
Case report
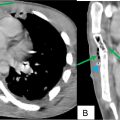
A 44-year-old man with a 24-year smoking history and no significant medical history was noted to have an enlarged shadow in the right upper mediastinum on chest radiography during physical examination. Two months later, a CT scan revealed a mediastinal mass ( Figs. 1 A and B). Eleven days after the initial CT scan, the patient visited the emergency department at our hospital because of cough, dyspnea, and throat pain.

Chest radiography at admission showed further enlargement of the right upper mediastinal shadow ( Fig. 2 ). Dynamic CT identified a weakly enhanced tumor in the superior-to-middle mediastinum, which had grown from 5.0 × 5.0 cm to 9.0 × 7.0 cm over 2 weeks compared with the initial CT scan. The right brachiocephalic vein and superior vena cava were highly compressed and narrowed by the mass, and the trachea was left-deviated. Multiple enlarged mediastinal lymph nodes, including those at the right hilum and contralateral regions, were observed ( Figs. 3 A-E). Laboratory tests revealed slightly elevated LDH (296 IU/L) and CRP (3.29 mg/dL) levels but no other abnormalities. Tumor markers (CYFRA, pro-GRP, CEA, CA19-9) and sIL-2R were all negative.


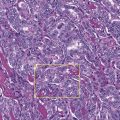
Mediastinal lung cancer was the primary differential diagnosis, with malignant lymphoma also considered. On the first day of admission, a CT-guided biopsy was performed. Pathology revealed extensive necrosis and clusters of large pleomorphic cells with prominent nucleoli and nuclear atypia ( Fig. 4 A). Immunostaining revealed positivity for the epithelial markers EMA and AE1/AE3 ( Figs. 4 B and C), with some low-molecular-weight keratin-positive cells, suggesting an epithelial tumor origin. However, tumor markers that commonly test positive in lung cancer (TTF-1, p40, CK7, ALK) and lymphoma markers (CD3, CD5, CD117) tested negative. Finally, SMARCA4 deficiency was confirmed immunohistochemically ( Fig. 4 D), leading to a definitive diagnosis of Thoracic SMARCA4 -UT on day 12.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree