Thyroid
Key Points
Thyroid carcinomas are classified into four histologic types. Papillary and follicular carcinomas are often grouped together as well-differentiated cancers. Medullary and particularly anaplastic carcinomas have more aggressive behaviors but are, fortunately, much less common.
Surgery is the primary therapy for thyroid carcinomas.
There are two reasons to use radioactive iodine (RAI) after surgery for well-differentiated thyroid carcinoma. The first objective is to ablate residual thyroid tissue to allow more effective detection of the presence of metastatic deposits that take up iodine. The second objective is to ablate “functional” metastatic disease using higher doses (100 to 150 mCi) of RAI.
Adjuvant external beam radiation has a limited role for the treatment of well-differentiated carcinomas. In general, it is only recommended for elder patients with invasive tumors, for example, extensive infiltration of the neck soft tissues; adherence to the perichondrium of the thyroid, cricoid, tracheal cartilages; or extensive extracapsular extension of nodal disease, etc. It is also recommended for patients who have undergone surgery for recurrent disease.
Because of a higher risk for local-regional recurrence, adjuvant external beam radiation is often recommended for the treatment of medullary thyroid carcinoma. Due to lack of any randomized clinical trials, it is difficult to estimate the magnitude of effect of adjuvant radiotherapy in improving the local-regional tumor control and the impact of radiation on overall survival for patients with medullary carcinoma.
Anaplastic carcinoma is one of the most aggressive human cancers. The median survival of patients presenting with this cancer is measured in months. Radiation, often with concurrent chemotherapy, is recommended for inducing local tumor regression as these patients can rapidly develop airway obstruction and severe dysphagia.
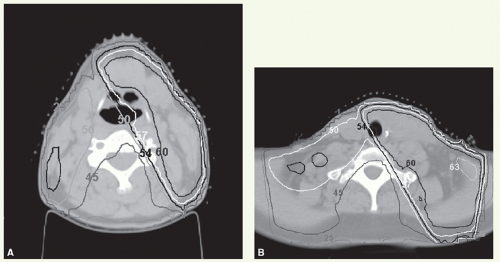
The horseshoe-shaped geometry of the target volumes, which often include the laryngeal inlet, tracheoesophageal grooves, and superior paratracheal nodal basins, coupled with significant changes in depth, width, and curvature from the neck to the mediastinum, makes treatment planning with conventional radiation technique very complex. Fortunately, the introduction of intensity-modulated radiation therapy technology greatly facilitates treatment planning and delivery.
TREATMENT STRATEGY
The primary treatment for thyroid cancers is surgery. RAI is a generally accepted adjuvant therapy to surgery for most functioning papillary or follicular carcinomas.
Relative indications for postoperative external beam radiotherapy depend on tumor histology. For differentiated (follicular/papillary) cancers that do not take up RAI, the indications include incomplete resection, direct invasion of adjacent structures (trachea, nerve, muscle, etc.),
extracapsular extension of nodal disease, extensive mediastinal nodal involvement, and resection of recurrent disease at the primary site.
extracapsular extension of nodal disease, extensive mediastinal nodal involvement, and resection of recurrent disease at the primary site.
Medullary carcinoma has the same indications as that of differentiated cancer plus persistent elevation of calcitonin levels after surgery, without demonstrable distant metastatic disease.
For anaplastic carcinoma, all patients receive irradiation, if possible, after maximal surgical debulking. Patients with locally advanced anaplastic carcinoma are generally enrolled into ongoing Phase II protocols testing combination of chemotherapy and, more recently, targeted agents (varies with protocol) with local-regional treatment.
Case Study 14-1
A 64-year-old woman was found to have a thyroid nodule on routine physical examination. She had no family history of thyroid cancer and had never received radiotherapy. CT scan showed a mass in the right lobe of the thyroid gland. There was no evidence of associated lymphadenopathy or disease in the mediastinum. Fineneedle aspiration showed medullary thyroid carcinoma. Serum calcitonin levels were elevated. Carcinoembryonic antigen level was normal. Metastatic workup results were negative. The patient underwent a thyroidectomy and right neck dissection. Histologic examination showed a 2-cm medullary carcinoma of the right lobe. Eight right paratracheal nodes and four jugular nodes were positive, the largest measuring 1.2 cm. Postoperatively, serum calcitonin levels remained elevated. Because of extensive nodal involvement and persistent elevated serum calcitonin level, it was decided to deliver postoperative radiotherapy.
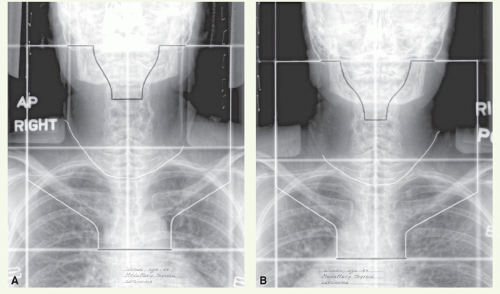
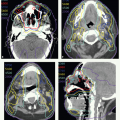
Figure 14.1 shows opposed AP-PA portals, with a compensating filter for the anterior field, used to treat the initial target volume (Fig. 14.1A,B). The wire indicates the surgical scar. A dose of 44 Gy was delivered in 22 fractions following which the left anterior-oblique and right posterioroblique fields (Fig. 14.1C,D) were used to boost the tumor bed and right neck. After reaching a tumor dose of 50 Gy, the length of the oblique fields was reduced to encompass the areas of known tumor involvement for an additional 10 Gy. Therefore, the primary tumor bed and involved nodal areas received a total dose of 60 Gy, the right neck received a dose of 50 Gy, and the contralateral neck and mediastinum received a dose of 44 Gy, all delivered in 2 Gy per fraction. This patient was alive without evidence of disease and without complications 6 years after completion of therapy.
POSTOPERATIVE RADIOTHERAPY
Target Volume
The initial target volume encompasses the surgical bed, TE grooves, neck nodes at risk, upper mediastinum, and midmediastinal area when upper mediastinum is involved (see Case Study 14-1). The boost volume encompasses the area of known disease locations with 1- to 2-cm margins.
Setup and Field Arrangement for Conventional Technique
Marking of surgical scar facilitates portal design. The patient is immobilized with thermoplastic mask in a supine position, with the head hyperextended to minimize inclusion of oral cavity in the portal. If the patient is unable to hyperextend the neck, a cephalad gantry tilt can be used to achieve the same goal. Opposed anterior and posterior (AP-PA) photon fields are used for the initial target volume:
Superior border: at the level of the mastoid processes. It can be lower on the side of the neck that has a low risk for microscopic nodal involvement to spare the ipsilateral submandibular gland.
Lateral borders: covering the medial two-thirds of the clavicles.
Inferior border: just below the carina (when upper mediastinum is involved, it is 3 to 4 cm below the mediastinal component).
The use of missing tissue compensating filter or field-in-field technique (see Chapter 3) minimizes dose heterogeneity, and therefore potential overdose to a segment of the spinal cord, because of the large differences in the diameter of the patient at different anatomic levels.
The oral cavity and oropharynx can be shielded to the extent possible without compromising on the coverage of the tumor bed and neck.
The boost dose is usually delivered through opposed anterior-oblique and posterior-oblique off-cord photon fields encompassing the tumor bed and the side of the neck with nodal involvement. A planning computed tomography (CT) scan is obtained to determine the angle and width of these fields. The superior and inferior borders are chosen according to the extent of the disease.
If the contralateral neck or thyroid bed is also at high risk, it can receive boost dose through an appositional electron field with a gantry angle corresponding to that of the anterior-oblique photon field to avoid overlap (see Case Study 14-2).
Intensity-Modulated Radiation Therapy
Intensity-modulated radiation therapy (IMRT) generally offers better coverage of the rather complex anatomy and geometry. An example of the former is the difference in tissue thickness between the neck and mediastinum, and the target is often a horseshoe-shaped tumor bed.
With IMRT, the patient is immobilized with an extended head and shoulder thermoplastic mask in a supine position. Extending the head aids in minimizing exposure to oral cavity. Thin-slice CT scan is obtained for delineation of target volumes (see Case Studies 14-3, 14-4, 14-5 and 14-6).
Virtual Gross Target Volume
There is no actual gross target volume (GTV) after complete surgical tumor resection. However, it can be useful to formulate a virtual GTV (vGTV) to facilitate target volume definition. The vGTV is the best approximation of the tissues having high likelihood of harboring microscopic tumor reconstructed based on findings of preoperative clinical examination, imaging studies, and surgical-pathologic assessment.
Case Study 14-2
A 48-year-old woman underwent a total thyroidectomy for papillary carcinoma followed by postoperative RAI ablation. A year later, she represented with a 2-cm left neck mass. Fine-needle aspiration confirmed recurrence, and she underwent a left neck and central compartment dissection. Histologic examination revealed recurrent thyroid carcinoma in the connective tissues of the neck. A postoperative iodine scan was negative. She received postoperative external beam radiation.
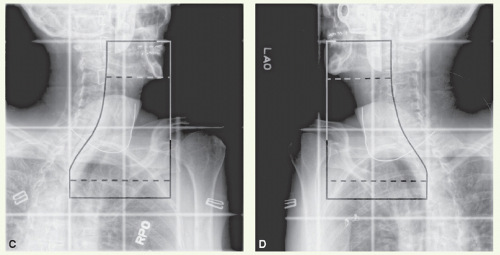
The radiation treatment commenced with parallelopposed anterior (6-MV photons) and posterior (18-MV photons) fields. The portals covered the entire neck and upper mediastinum. After a dose of 42 Gy, the fields were reduced off-spinal cord by using parallel-opposed right anterior-oblique and left posterior-oblique fields. At 50 Gy, a reduction was made off the superior and inferior borders, and the areas felt to be at the highest risk were irradiated to 60 Gy. The right neck was supplemented with 12-MeV electron beam to bring the dose to the mid and lower right neck to 50 Gy.
Figure 14.2 shows representative axial isodose distribution through the mid (Fig. 14.2A) and lower (Fig. 14.2B) neck.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree