Type II endoleaks are common benign complications that occur following endovascular aneurysm repair (EVAR). When traditional transarterial embolization fails in the management of these endoleaks, alternative approaches such as the transcaval approach can be attempted. The transcaval approach can be performed from either right internal jugular or common femoral vein access sites. The technique utilizes intravascular ultrasound or landmark fluoroscopy to visualize direct needle access into the aneurysm sac. Once access is obtained, the source of the endoleak can be embolized with either coils, liquid embolics, or thrombin. The technique is well tolerated by the vast majority of patients. Technical challenges include the need for a capable assistant and approach vectors. Possible complications include iatrogenic type III endoleaks, graft and/or coil pack infections, and persistent or recurrent type II endoleaks. This article will review indications and evaluation of patients for transcaval endoleak embolization, describe the procedure in a step-by-step fashion, and discuss potential technical challenges and complications.
Introduction and clinical background
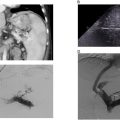
An 85-year-old male with a past medical history significant for hypertension, peripheral arterial disease, renal artery stenosis, and abdominal aortic aneurysm status post endovascular aneurysm repair (EVAR) 5 years prior presents for evaluation of a type II endoleak. At the time of the initial EVAR, the patient’s aneurysm sac measured 5.5 cm. The patient’s course was complicated by a type II endoleak which was previously treated with coil and liquid embolization 3 years prior to presentation. Routine follow-up ultrasound examinations demonstrated progressive enlargement of the aneurysm sac. Subsequent computed tomography angiography (CTA) of the abdomen and pelvis confirmed enlargement of the sac to 6.8 cm with evidence of a type IIb endoleak ( Fig. 1 ). Additionally, the patient was found to have an enlarging right internal iliac artery aneurysm measuring up to 2.9 cm. At the time of evaluation, the patient was in his usual state of health and denied new chest, abdominal, and back pain. On physical examination, the patient was hemodynamically stable with no abdominal tenderness. Given evidence of endoleak with sac enlargement, the decision was made to proceed to the angiography suite for arteriogram with embolization.

Type II endoleaks occur in approximately 10%-20% of EVAR cases. , Most commonly, type II endoleaks are due to collateral contribution from the inferior mesenteric artery (IMA) or lumbar arteries. In these cases, transarterial embolization of the culprit artery is the preferred management strategy. However, this is not always technically feasible, or the contributing artery may not confidently be identified. Therefore, alternative approaches must be employed. This article seeks to describe the technical aspects of the transcaval approach in the management of type II endoleaks.
Clinical evaluation of the patient
As with all procedures, thorough evaluation of the patient is necessary prior to proceeding with a transvenous approach in the management of aortic endoleak. Knowledge of the size and morphology of the initial aneurysm and the immediate poststent graft appearance of the aneurysm sac is critical for determining when to intervene. Imaging is the primary mode of surveillance following EVAR. Abdominal ultrasound examinations can provide a cost effective and efficient method for monitoring the size of the aneurysm sac. Evidence of sac enlargement should prompt evaluation with triple phase CTA of the abdomen and pelvis, including noncontrast, arterial, and delayed venous phases.
When interpreting the CTA, there are several key features that should be evaluated. First and foremost, sac enlargement should be confirmed with direct comparison to prior imaging, ensuring similar planes of measurement are used. Next, contrast enhancement of the sac should be seen on either the arterial or the delayed venous phase of the study. Not only is this indicative of the presence of a potentially treatable endoleak, but the location and morphology of the contrast enhancement can suggest possible sources. The spatial relationship of the aneurysm sac to adjacent venous structures, most commonly the inferior vena cava, is of utmost importance. Naturally, direct apposition of the sac and vein is preferred for the transvenous approach to enable ease of access. Additional anatomic factors include the presence of interposed vertebra or visceral structures, vessel tortuosity, and the presence of calcifications on the aneurysm sac wall. Special attention should also be paid to the relation of the endograft and the planned access site. Close approximation of the endograft to the planned access site risks inadvertent puncture of the graft and creation of a type III endoleak.
Preoperative evaluation of the patient’s health status is also critical. Recent laboratory studies should be available including a CBC, CMP, and type and screen. Additionally, the operator should determine whether anesthesia support is necessary. While this procedure can be performed under moderate sedation, length of table time and potential for complications such as hemorrhage are reasons to consider anesthesia engagement.
When to utilize the transcaval approach
A transcaval approach for endoleak management should not be considered first line for the management of type II endoleaks. Direct embolization of the feeding arteries should be attempted prior to committing to the transvenous approach. Direct embolization is often technically less challenging with a lower risk profile and a high chance of successful treatment. However, the transcaval approach is reasonable when direct embolization is not technically feasible, when prior embolization fails to prevent sac enlargement, or if an occult endoleak is present. The primary contraindication for the transcaval approach is unfavorable anatomic relation between the aneurysm sac and the vein.
Equipment needed
The standard armamentarium of the endovascular interventionalist should be available including vascular access kits, vascular sheaths, and standard wires and catheters. In addition to this, access to an intracardiac echocardiography (ICE) machine is recommended. ICE provides a higher degree of directionality, image quality, and needle visualization compared with 360-degree intravascular ultrasound machines. The ICE catheter requires a 9 French vascular sheath, preferably at least 35 cm in length. A coaxial needle-catheter access system is also required for this approach. A transjugular intrahepatic portosystemic shunt (TIPS) kit provides a robust platform for access into the sac. While the exact TIPS kit used is operator dependent, the authors use a Rösch-Uschida access kit. Once the aneurysm is accessed, an 0.035-inch stiff guidewire and a 6 French flexible vascular sheath is utilized to allow for better articulation within the aneurysm sac. An array of microcatheters should be available for use following access of the sac to successfully select any identifiable feeding arteries. Embolic materials should also be available. Our practice prefers the combination of a liquid embolic such as Onxy 34 (Medtronic, Minneapolis, USA) and both 0.018- and 0.035-inch coils.
Procedure description
The patient is brought into the angiography suite and placed in the supine position. General anesthesia is then induced, and the patient is prepped and draped in sterile fashion. Initial venous access is obtained either using the right common femoral vein or the right internal jugular vein. The right internal jugular vein is preferred as many endoleaks requiring transcaval treatment are from the lower lumbar or median sacral arteries. By utilizing the internal jugular vein, the angle of approach into the sac and subsequent navigation within the sac becomes more in-line with the operator. Ultrasound is used to identify the internal jugular vein and a dermatotomy is made overlying the vein. Using ultrasound guidance, a micropunture needle is advanced into the right internal jugular vein. An 0.018-inch wire is then introduced into the SVC. Traditional exchanges and dilations are then performed until an 0.035-inch wire and a 9 French by 35 cm vascular sheath can be placed into the IVC. Initial diagnostic venography with iodinated contrast can then be performed of the IVC. The ICE catheter is then introduced into the 9 Fr sheath and endovascular ultrasound examination of the vein and aneurysm sac is then performed, focusing on identifying a suitable transvenous access site into the sac.
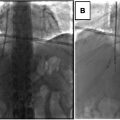
A second site of access in the right internal jugular vein is then obtained in identical fashion as above. The 10 French sheath that is parceled with the Rösch-Uschida kit is then introduced into the IVC ( Fig. 2 ). The coaxial 18-gauge needle and 5 Fr Teflon catheter are then transitioned into the Rösch-Uschida sheath and introduced into the IVC ( Fig. 3 ). Under direct ultrasound and fluoroscopic visualization, the Rösch-Uschida needle is advanced into the aneurysm sac ( Figs. 4 and 5 ). Once the needle is within the sac, advance the catheter over the needle to establish access within the sac ( Figs. 6 and 7 ). Remove the needle from the catheter and introduce a stiff guidewire into the sac, ensuring enough wire is looped within the sac to maintain access. Next, exchange the Teflon catheter for a 6 French flexible sheath. A 4 or 5 French angled tip diagnostic catheter such as a Berenstein catheter is then advanced towards the suspected source of the endoleak ( Fig. 8 ). Through this catheter, diagnostic digital subtraction angiography (DSA) can be performed to identify the source of the endoleak ( Fig. 9 ).