Trauma
SKULL FRACTURES
KEY FACTS
Linear fractures or sutural diastases with no underlying brain injury are generally not clinically significant; formation of leptomeningeal cysts and/or herniated brain (“growing fracture”) is very rare (does not require follow-up radiographs).
Fractures through the base of skull or paranasal sinuses may produce pneumocephalus, cerebrospinal fluid (CSF) leaks, and meningitis.
Fracture through the temporal bone may give origin to gas in the temporomandibular joint.
Depressed fracture = fragments are displaced by more than 0.5 cm; most depressed fractures have underlying contusions, and contrecoup injuries are present in 30% of patients.
Most depressed fractures are considered “open” and require debridement and antiobiotic treatment.
Most skull fractures have no underlying brain injuries, and most severe brain injuries have no skull fractures; plain radiographs are not useful in suspected cerebral trauma.
Skull radiographs may be helpful to document fractures (which may be missed by CT if oriented parallel to slices) for legal purposes as in non-accidental trauma.
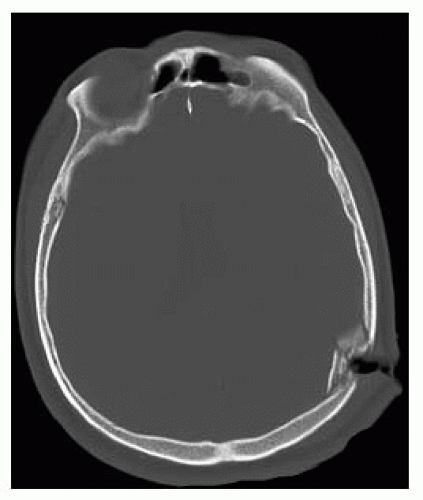
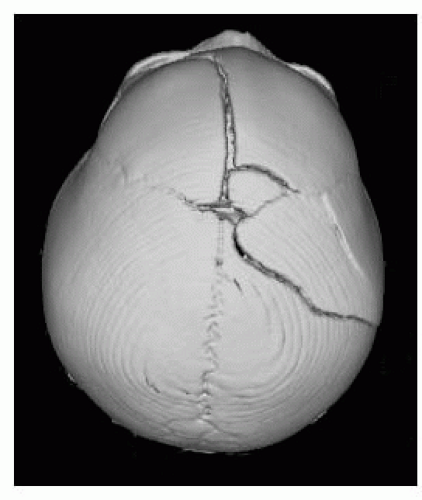 FIGURE 8-2. Top view from a shaded-surface display, in a different patient, shows a comminuted left temporofrontal fracture and diastasis of the metopic suture. |
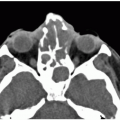
 FIGURE 8-3. Axial CT, shows a depressed left frontal fracture with underlying hemorrhagic contusion and pneumocephalus. |
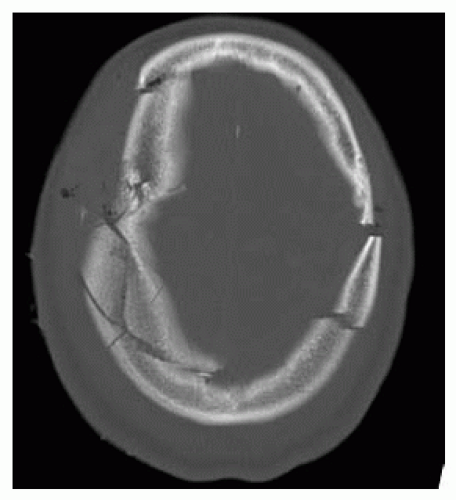
 FIGURE 8-5. Axial CT in a patient hit with baseball bat shows large significantly depressed fracture. |
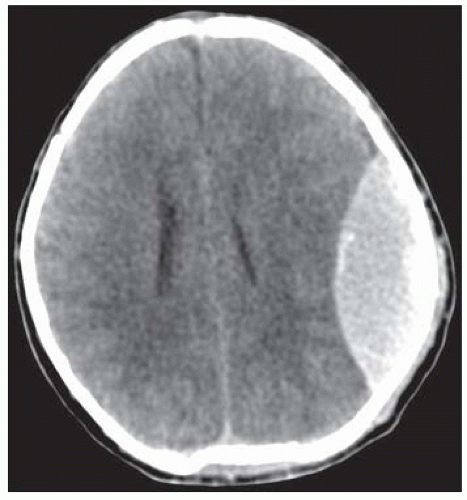
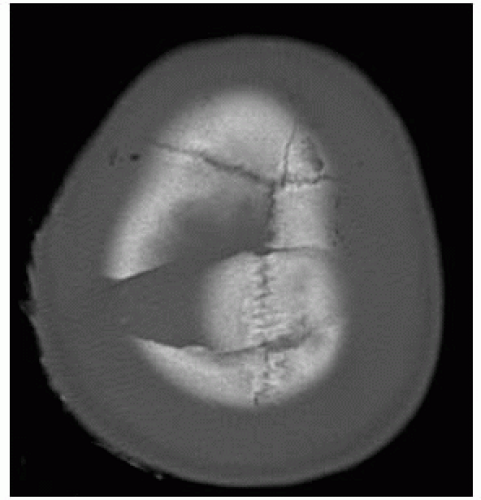 FIGURE 8-6. Axial CT, showing fractures crossing midline which risk damaging the superior sagittal sinus. |
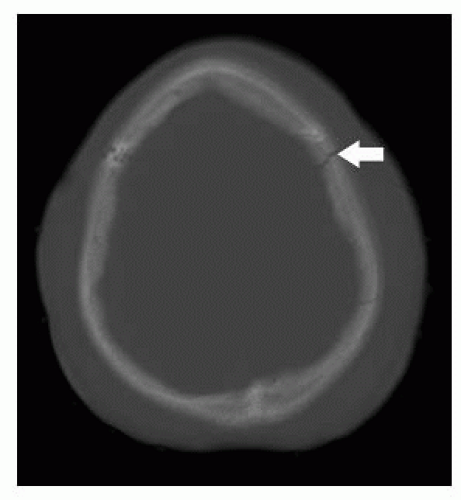
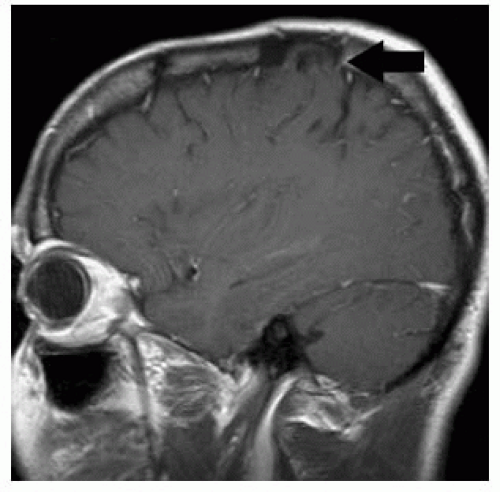 FIGURE 8-8. Parasagittal T1 image in a patient with a growing fracture shows herniation of brain (arrow) into expanded fracture site. |
SUGGESTED READING
Sun JK, LeMay DR. Imaging of facial trauma. Neuroimaging Clin N Am 2002;12:295-309.
EPIDURAL HEMATOMA
KEY FACTS
50% to 75% of severe head trauma victims will have an epidural hematoma.
About 70% to 75% of epidural hematomas occur in the temporoparietal region secondary to laceration of the middle meningeal artery.
CT identifies underlying fracture in 85% to 95% of epidural hematomas.
“Lucid” interval seen in 50% of patients and precedes clinical deterioration; overall mortality = 5%; delayed enlargement of hematoma occurs in 10% to 30% of patients.
95% of epidural hematomas are supratentorial and unilateral.
“Vertex” hematomas are always epidural, cross the superior sagittal sinus, and displace it inferiorly.
In children, epidural hematomas may arise from laceration of venous sinuses.
A venous sinus origin should be suspected when the hematoma abuts both sides of the tentorium or is adjacent to a dural venous sinus.
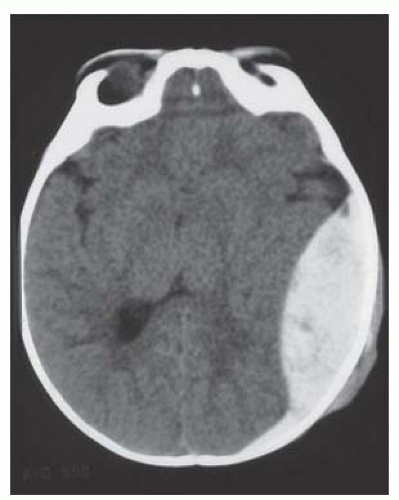 FIGURE 8-9. Axial CT shows a biconvex acute (dense) epidural hematoma in the left posterior temporal region in a child. |
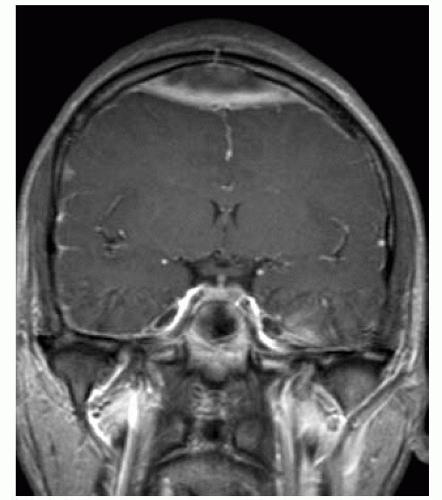 FIGURE 8-12. Coronal T1, in a different patient, shows a convexity (vertex) epidural hematoma typically crossing the midline venous structures. |
SUGGESTED READING
Hardman JM, Manoukian A. Pathology of head trauma. Neuroimaging Clin N Am 2002;12:175.
SUBDURAL HEMATOMA AND HYGROMA
KEY FACTS
Subdural hematomas are found in 10% to 20% of severe head trauma victims. Overall mortality rate for patients with subdural hematomas is 60% to 90%.
95% occur in the frontoparietal regions due to tearing of bridging veins.
10% to 15% are bilateral; interhemispheric location in children suggests abuse.
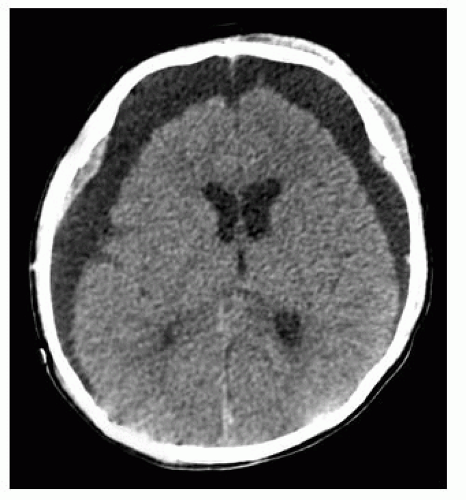
CT: acute (<3 days) are hyperdense; subacute (3 to 21 days) are isodensity; chronic (>3 weeks) are hypodense.
Both isodense and hypodense (subacute and chronic) subdural hematomas may have inner membrane contrast enhancement.
Visualization of small subdurals requires the use of intermediate CT window settings (width: 250; level: 40); generally, these hematomas are small and not clinically significant.
Cerebral contusions are seen in 50% of patients with subdural hematomas.
Subdural hematomas may follow ventricular shunting.
Hygromas are collections of nonbloody CSF in the subdural space caused by a tear in the arachnoid membrane. Most occur in older persons. Hematohygromas have both blood and CSF and are seen in child abuse.
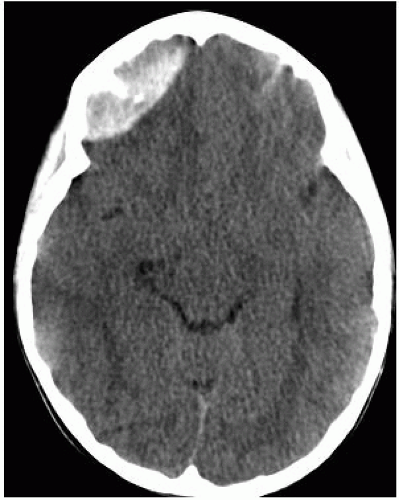
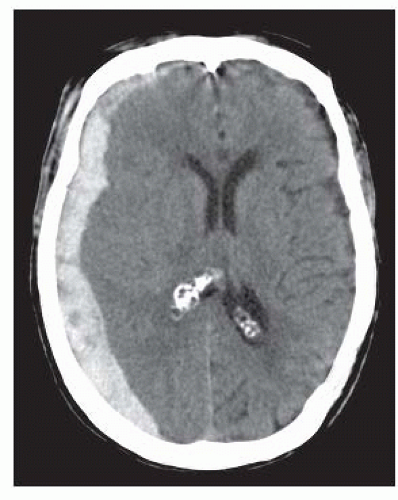 FIGURE 8-13. Axial CT shows an acute dense right hemispheric subdural hematoma with mass effect and midline shift to the left. |
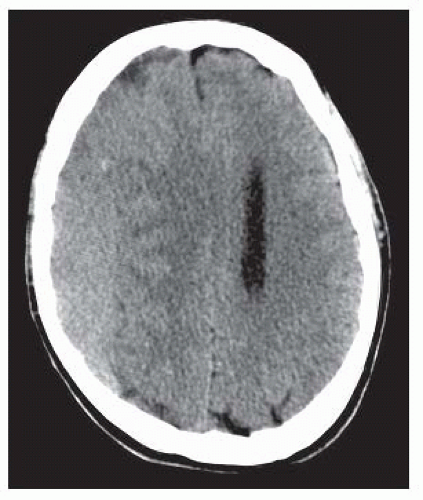 FIGURE 8-14. Axial CT, shows the subacute right subdural hematoma that is nearly isodense to brain; the left lateral ventricle is effaced due to mass effect. |
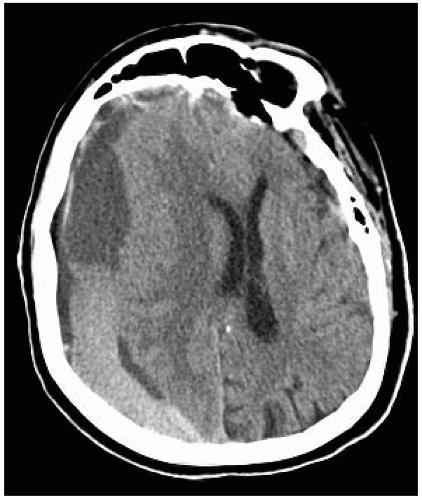 FIGURE 8-15. Superimposed acute bleed is seen as dense fluid level in the dependent portion of a right chronic (supernatant is hypodense) that has significant mass effect. |
SUGGESTED READING
Young RJ, Destian S. Imaging of traumatic intracranial hemorrhage. Neuroimaging Clin N Am 2002;12:189.
DIFFUSE AXONAL INJURY AND INTERMEDIARY INJURIES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree