Abstract
Purpose
To describe the overall treatment patterns of follicular lymphoma (FL) in a single tertiary institution, with a focus on the outcomes of radiotherapy treatment in this group of patients.
Methods and materials
Retrospective analysis on 177 patients with FL registered from 1996 to 2011 and followed up to October 2017. Diagnosis was confirmed by histology and staging by clinical examination and imaging with positron emission tomography (PET) or computed tomography (CT) scan. Demographics, clinicopathological characteristics, treatment details and clinical outcomes were reviewed.
Results
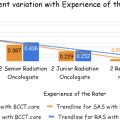
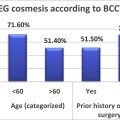
Fifty-five patients (31%) had early stage and 122 (69%) had advanced stage FL. Median follow-up was 7 years and 7.5 years for early and advanced FL respectively. For advanced stage, median overall survival (OS) was 12.9 years, 5-year and 10-year OS were 77% and 63%, and 5-year and 10-yr PFS were 57% and 40% respectively. In multivariable model, moderate FLIPI, palliative RT and anti-CD20 targeted therapy were significantly associated with OS when comparing with those with high FLIPI score, no RT and no anti-CD20 targeted therapy respectively. For early stage, median OS has not reached, 5-year and 10-year OS were 79% and 74% and 5-year and 10-year progression free survival (PFS) were 64% and 52% respectively. Stage 2 non-contiguous disease had significantly poorer survival than stage 1 patients in multivariable (HR 8.19, 95%CI 1.86 – 35.98) analysis. Overall, 49 of 177 patients (27.7%) had any form of radiotherapy as part of their treatment for FL. There were no in-field alone relapses seen in all cases treated with RT. 10% in early FL had G3-4 acute toxicities with RT whilst there was no G3-4 late toxicities. In advanced FL, there were no G3-4 acute toxicities with consolidation RT and 1 G3 with salvage RT.
Conclusion
FL has effective response rates to RT both in early and advanced FL. We demonstrated that: 1) stage 2 disease has poorer outcomes than stage 1 disease with stage 2 non-contiguous disease having the poorest outcomes, indicating the need for more aggressive treatment strategies for this group of patients; 2) there were no in-field alone relapses seen in all cases treated with RT; 3) overall, there is a general under-utilization of RT concurring with the literature. New prospective studies are therefore warranted to shed light on improving the utility of RT for patients with FL. With advances in molecular medicine, imaging and treatment approaches, there is potential for better stratification of different patient groups for more localized versus systemic treatments.
Highlights
- •
Both early and advanced follicular lymphomas (FL) have effective response to RT.
- •
There were no in-field alone relapse and low incidence of toxicities with RT.
- •
Non-contiguous stage 2 FL have poorer outcomes than other early FL.
- •
More aggressive treatment approach is needed for non-contiguous stage 2 disease.
- •
Better disease stratification needed in view of imaging and treatment advances.
1
Introduction
Follicular lymphoma (FL) is the most common indolent Non-Hodgkin Lymphoma (NHL) [ ]. Majority of patients present with advanced stage (stage 3 and 4) disease whilst early stage (stage 1 and 2) accounts for 22–33% of cases [ , ].
In early stage FL, radiotherapy (RT) can be curative with local control rates of more than 90%, 40–50% relapse free survival and 60–80% overall survival (OS) at 10 years [ ]. Despite this, RT has generally been underused in favour of other treatments such as chemotherapy, combined treatment modalities or initial observation [ , ]. For advanced stage FL, its indolent course and the lack of curative therapy means a watch-and-wait strategy is an option for asymptomatic patients with low tumour burden. For symptomatic and bulky tumours, symptom control becomes the main focus and multimodality treatment including immunotherapy, chemotherapy and RT are usually recommended [ ]. RT may also be considered for consolidation after systemic therapy in either incomplete or complete responders with initial bulky disease or in the palliative setting [ ]. The treatment of stage 2 disease is still controversial whereby some are treated as localized and others as advanced disease.
With modern imaging techniques, improved staging of patients and better volume delineation for more conformal RT treatment with reduced toxicity can be achieved [ ]. Furthermore, with recent studies such as the FORT trial showing efficacy with low dose radiotherapy, RT can be given with less toxicity [ , ]. Thus, RT is not only particularly valuable in treating early stage disease upfront but also as an excellent salvage and palliative option particular in the elderly with poor tolerance to systemic treatment [ ].
In this study, we aim to describe the overall treatment patterns of FL in a single tertiary institution, with a focus on the outcomes of radiotherapy treatment in this group of patients.
2
Patients and methods
2.1
Patients
177 patients with FL registered between 1996 and 2011 were included in this analysis. 180 patients were first identified. Three patients with incomplete information were excluded from the analysis. 10 patients with advanced stage disease were lost to follow up but included and censored at date of last visit.
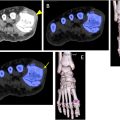
Diagnosis of FL was confirmed by histology. Staging was confirmed with clinical examination and imaging with either Positron Emission Tomography – Computed Tomography (PET-CT) or CT scan. Demographics (age, gender), clinicopathological characteristics, treatment details (surgery, chemotherapy, RT) and clinical outcomes were collected from clinical notes. Ann Arbor stage I and II were categorized as early stage and III and IV as advanced stage. Follicular Lymphoma International Prognostic Index (FLIPI score) was calculated from age, number of involved nodal site, lactate dehydrogenase (LDH), haemoglobin (Hb) and Ann Arbor stage and categorized as low risk group (FLIPI 0–1), intermediate risk group (FLIPI 2) and high risk group (FLIPI 3–5) [ ]. Radiation dose was described as Equivalent total dose calculated in 2Gy per fraction (EqD2).
2.2
Outcomes
OS was defined as time from diagnosis to date of death, alive or lost to follow-up. Progression-free survival (PFS) was defined as time from diagnosis until disease relapse or death. Surviving patients without relapse or lost to follow-up were censored at their date of last follow-up. Disease relapse was determined by histological confirmation. Toxicity of treatment was graded according to the Common Terminology Criteria for Adverse Events (CTCAE).
2.3
Statistical methods
Patient characteristics and treatments were summarized using frequency and percentages for categorical variables, and median with inter-quartile range (IQR) and range for continuous variables. Median follow-up time was calculated using the observation time method. Survival curves were estimated using the Kaplan-Meier Method. Differences in survival curves between groups of patients were assessed using the log-rank test. Univariable and multivariable cox regression analyses were performed to assess the association between patient characteristics and survival outcomes. Variable selection for multivariable analysis was performed using the backward elimination method by optimizing AIC. The proportional hazards assumption for cox regression was checked using statistical tests and graphs based on the scaled Schoenfeld residuals. Statistical significance was assessed by two-sided p-value less than 0.05. All statistical analyses were performed using R software (version 3.6.0).
3
Results
177 patients were included in the study. Patient characteristics are summarized in Table 1 . The median age was 58.3 years (range: 22.5–91.8 years). The ratio of male and female patients was balanced. Majority of patients had advanced stage disease (n = 122 (69%)) whilst 55 patients (31%) had early stage disease. None of stage 1, 2 (7.7%) of stage 2, 32 (55.2%) of stage 3 and 36 (56.2%) of stage 4 had high FLIPI at time of diagnosis. Median follow up was 7.43 years (IQR: 3.25–10.48 years). 49 of 177 patients (27.7%) had any form of radiotherapy as part of their treatment for FL. Further treatment characteristics and outcomes are described in Table 1 according to early and advanced stage disease.
| Stage 1 (N = 29) | Stage 2 (N = 26) | Stage 3 (N = 58) | Stage 4 (N = 64) | Total (N = 177) | |
|---|---|---|---|---|---|
| Age | |||||
| Median (IQR) | 60.2 (51.0, 64.9) | 51.9 (48.4, 60.7) | 60.6 (54.3, 73.3) | 56.8 (51.8, 64.7) | 58.3 (51.4, 66.2) |
| Range | 22.9–84.7 | 22.5–87.5 | 36.8–91.8 | 29.9–75.9 | 22.5–91.8 |
| Age group | |||||
| ≤60yrs | 14 (48.3%) | 19 (73.1%) | 27 (46.6%) | 37 (57.8%) | 97 (54.8%) |
| >60yrs | 15 (51.7%) | 7 (26.9%) | 31 (53.4%) | 27 (42.2%) | 80 (45.2%) |
| Gender | |||||
| Female | 15 (51.7%) | 9 (34.6%) | 34 (58.6%) | 28 (43.8%) | 86 (48.6%) |
| Male | 14 (48.3%) | 17 (65.4%) | 24 (41.4%) | 36 (56.2%) | 91 (51.4%) |
| Abnormal LDH | |||||
| No | 25 (86.2%) | 20 (76.9%) | 30 (51.7%) | 38 (59.4%) | 113 (63.8%) |
| Yes | 2 (6.9%) | 6 (23.1%) | 24 (41.4%) | 24 (37.5%) | 56 (31.6%) |
| Unknown | 2 (6.9%) | 0 (0.0%) | 4 (6.9%) | 2 (3.1%) | 8 (4.5%) |
| Abnormal Hb | |||||
| No | 25 (86.2%) | 21 (80.8%) | 39 (67.2%) | 46 (71.9%) | 131 (74.0%) |
| Yes | 4 (13.8%) | 5 (19.2%) | 17 (29.3%) | 18 (28.1%) | 44 (24.9%) |
| Unknown | 0 (0.0%) | 0 (0.0%) | 2 (3.4%) | 0 (0.0%) | 2 (1.1%) |
| FLIPI | |||||
| High (≥3) | 0 (0.0%) | 2 (7.7%) | 32 (55.2%) | 36 (56.2%) | 70 (39.5%) |
| Moderate (2) | 1 (3.4%) | 7 (26.9%) | 20 (34.5%) | 20 (31.2%) | 48 (27.1%) |
| Low (0–1) | 28 (96.6%) | 17 (65.4%) | 2 (3.4%) | 7 (10.9%) | 54 (30.5%) |
| Unknown | 0 (0.0%) | 0 (0.0%) | 4 (6.9%) | 1 (1.6%) | 5 (2.8%) |
| Affected nodal regions | |||||
| <5 | 29 (100.0%) | 15 (57.7%) | 13 (22.4%) | 12 (18.8%) | 69 (39.0%) |
| ≥5 | 0 (0.0%) | 11 (42.3%) | 44 (75.9%) | 52 (81.2%) | 107 (60.5%) |
| Unknown | 0 (0.0%) | 0 (0.0%) | 1 (1.7%) | 0 (0.0%) | 1 (0.6%) |
| Surgery | |||||
| No | 20 (69.0%) | 23 (88.5%) | 57 (98.3%) | 61 (95.3%) | 161 (91.0%) |
| Yes | 9 (31.0%) | 3 (11.5%) | 1 (1.7%) | 3 (4.7%) | 16 (9.0%) |
| Chemotherapy | |||||
| No | 22 (75.9%) | 11 (42.3%) | 6 (10.3%) | 3 (4.7%) | 42 (23.7%) |
| Yes | 7 (24.1%) | 15 (57.7%) | 50 (86.2%) | 60 (93.8%) | 132 (74.6%) |
| Unknown | 0 (0.0%) | 0 (0.0%) | 2 (3.4%) | 1 (1.6%) | 3 (1.7%) |
| Radiotherapy | |||||
| No | 10 (34.5%) | 12 (46.2%) | 51 (87.9%) | 55 (85.9%) | 128 (72.3%) |
| Yes | 19 (65.5%) | 14 (53.8%) | 7 (12.1%) | 9 (14.1%) | 49 (27.7%) |
| RT doses | |||||
| Median (IQR) | 31.8 (30.0, 36.0) | 36.0 (34.5, 39.0) | 33.2 (30.2, 35.0) | 32.5 (30.0, 36.0) | 34.4 (30.0, 36.0) |
| Range | 6.0–46.0 | 30.0–46.0 | 28.6–40.0 | 24.0–50.0 | 6.0–50.0 |
| Early stage (N = 55) | Advance stage (N = 122) | |
|---|---|---|
| Surgery | ||
| No | 43 (78.2%) | 118 (96.7%) |
| Yes | 12 (21.8%) | 4 (3.3%) |
| Chemotherapy | ||
| No | 33 (60.0%) | 9 (7.4%) |
| Yes | 22 (40.0%) | 110 (90.2%) |
| Unknown | 0 (0.0%) | 3 (2.5%) |
| Radiotherapy | ||
| No | 22 (40.0%) | 106 (86.9%) |
| Yes | 33 (60.0%) | 16 (13.1%) |
| RT doses | ||
| Median (IQR) | 36.0 (30.0, 36.0) | 32.5 (29.7, 36.0) |
| Range | 6.0–46.0 | 24.0–50.0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree