Treatment of Local-Regional Recurrence
Key Points
Up to recently, reirradiation for recurrent local or regional disease has been widely discouraged because of concerns of inducing very severe complications, particularly neurologic deficits and carotid injury.
Relatively favorable outcome of reirradiation in selected patients with recurrent nasopharyngeal carcinoma along with progress in conformal radiation technique and emergence of radiobiological data have increased enthusiasm for adopting reirradiation in selected patients who are poor candidates for surgical salvage.
Special attention is given to minimize the dose to the spinal cord, brain stem, and, in patients with nasopharyngeal cancer, the temporal lobes to prevent devastating complications.
Concurrent chemotherapy is recommended with reirradiation unless medically contraindicated. Phase II experiences of concurrent chemo-reirradiation suggest this approach is feasible in carefully selected patients and can yield modest long-term control rate, but complications can be severe.
The role of adjuvant reirradiation is controversial. Relative indications for postoperative radiation in the unirradiated patient do not apply when considering reirradiation. Only patients with a very high risk of recurrence (i.e., positive margins or extensive soft-tissue disease) are selected for adjuvant postoperative reirradiation.
In addition to the general indications for radiation, the interval from the first radiation course and the health of the tissues to be irradiated should be considered in the decision-making process. Reirradiation is strongly discouraged if the interval between the two courses is <6 months.
REIRRADIATION FOR LOCAL RECURRENCE
Because of the technical complexity and high morbidity, surgical salvage for local recurrence of nasopharyngeal carcinoma has been attempted in a few specialized centers and in highly selected patients. Due to the lack of other options, many centers have resorted to treating patients with localized local recurrence with reirradiation. In our center, retreatment with curative intent after previous high-dose irradiation is offered to patients with relapse that is confined to the nasopharynx or with a limited extension to the adjacent parapharyngeal space, skull base, or both (see Case Study 17-1). Conformal radiotherapy, particularly intensity-modulated radiotherapy (IMRT) (see Case Studies 17-2 and 17-3), is now used to minimize the volume of normal tissues exposed to reirradiation and thereby reduce the acute and late morbidity. Recurrences above the skull base are often difficult to reirradiate due to the proximity to the brain stem and temporal lobes. Intracranial disease may be amenable to reirradiation if the initial fields did not encompass the cranial tissues (see Case Study 17-4).
Case Study 17-1
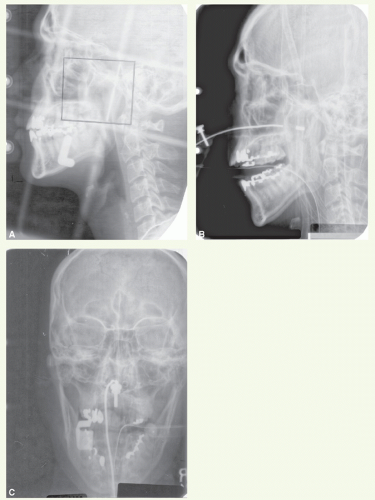
A 34-year-old man underwent radiation treatment for a T1 N0 M0 lymphoepithelioma of the nasopharynx. He received 64.8 Gy in 36 fractions to the primary tumor and 45 Gy in 25 fractions to the cervical nodes. He did well until a year later when he presented with epistaxis. Physical examination showed a small lesion in the left lateral wall, biopsy of which revealed a lymphoepithelioma. He was referred to our center for workup and treatment.
Examination at this time revealed a superficial lesion confined to the left lateral wall. There was no palpable lymphadenopathy Workup for metastatic disease was negative. He received external beam irradiation with 25-MV x-rays through lateral-opposed portals (Fig. 17-1A) to a dose of 25 Gy in 12 fractions. This was followed by an intracavitary insertion of 137Cs source (18.75 mg radium equivalent) into a Teflon ball (Fig. 17-1B,C) for 35.6 hours to deliver a dose of 50 Gy to the mucosal surface (23 Gy at 0.5-cm depth). This patient was alive without evidence of disease and without late complications from this treatment 10 years later.
Case Study 17-2
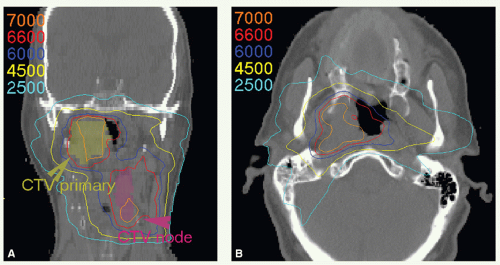
A 67-year-old man was diagnosed with WHO type 3 nasopharynx carcinoma. He received a combination of chemotherapy and radiation, but discontinued treatment at 50 Gy due to toxicity J He developed a recurrence in the right nasopharynx and left neck. He was reirradiated with IMRT and received concurrent cisplatin. A total dose of 66 Gy was administered in 33 fractions to the gross tumor with 1-cm margin.
Figure 17-2 shows isodose distributions on a coronal (Fig. 17-2A) and axial (Fig. 17-2B) image. The maximum dose to the spinal cord was 20 Gy in 33 fractions. He remains without disease 2 years from his retreatment.
Case Study 17-3
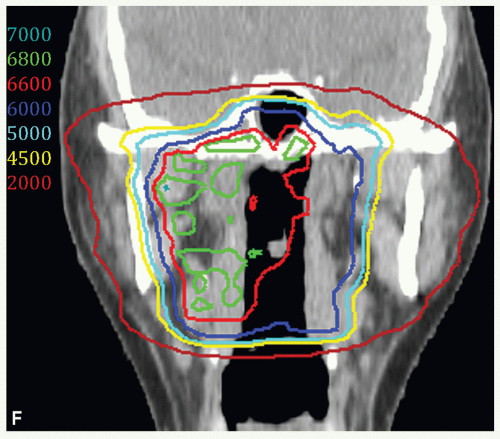
A 36-year-old man was treated in Asia with radiation for undifferentiated carcinoma. Treatment records were unavailable. He was found to have recurrent disease on routine follow-up evaluation 4 years later.
The restaging workup included a PET-CT scan (Fig. 17-3A), which revealed the recurrent disease confined to the right nasopharynx. Stage rT1 N0.
He was reirradiated with IMRT delivered with concurrent cisplatin.
As shown in Figure 17-3, two targets were defined. CTVHD (66 Gy, maroon colorwash) encompassed the gross disease in the right nasopharynx with margin and CTVED (60 Gy, blue colorwash) encompassed the left nasopharynx. Treatment was delivered in 33 fractions. Figure 17-3 also shows isodose distributions in axial views, with target volumes delineated, at the level of the tumor epicenter (Fig. 17-3B), inferior (Fig. 17-3C) and superior (Fig. 17-3D) nasopharynx, a sagittal view through midline (Fig. 17-3E), and a coronal view through the nasopharynx (Fig. 17-3F). As the previous records were unavailable, doses to the brain stem and spinal cord were limited to 20 Gy. The patient has no evidence of disease 4 years after reirradiation.
Case Study 17-4
A 43-year-old woman was treated for stage T1 Nl nasopharyngeal carcinoma with induction chemotherapy followed by hyperfractionated radiation regimen delivering 74 Gy in 69 fractions. Five years later, she presented with facial numbness and was found to have a mass in the left cavernous sinus. Review of her portals revealed that the recurrent tumor was located at the superior edge of the original portals (marginal recurrence) and much of the disease in the cavernous sinus was unirradiated.
She was treated with three cycles of taxane-platin-based induction chemotherapy achieving a partial response. Both the initial and postchemotherapy MRIs were used for planning of reirradiation by fusing them onto the retreatment planning CT scan.
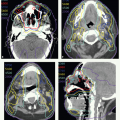
Figure 17-4A shows an axial slice on the pretreatment MRI. The gross disease was contoured in two separate volumes. The red contour surrounds the disease in the cavernous sinus, and the aqua contour surrounds the disease in the brain stem (brown contour). Figure 17-4B shows the postchemotherapy volume. The red and aqua contours represent pretreatment volumes fused onto this MRI and the green contour delineates the residual abnormality on the postchemotherapy scan. Figure 17-4C demonstrates the contours fused onto the CT planning scan. Doses were prescribed to these targets without expansion. Daily setup was verified with CT guidance. The residual disease was treated to 64 Gy, the prechemotherapy volume outside the brain stem to 60 Gy, and the prechemotherapy volume abutting the brain stem to 46 Gy. Treatment was delivered in 32 fractions, with concurrent weekly carboplatin. Figure 17-4 also shows isodose distributions on an axial (Fig. 17-4D) and on coronal views through the cavernous sinus (Fig. 17-4E) and brain stem (Fig. 17-4F




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree