Tumors and Tumor-like Lesions
SYNOVIAL (OSTEO)CHONDROMATOSIS
Synovial (osteo)chondromatosis (also known as synovial chondromatosis or synovial chondrometaplasia) is an uncommon benign disorder marked by the metaplastic proliferation of multiple cartilaginous nodules in the synovial membrane of the joints, bursae, or tendon sheaths. It is almost invariably monoarticular; rarely, multiple joints may be affected. The disorder is twice as common in men as in women and is usually discovered in the third to fifth decade. The knee is a preferential site of involvement, with the hip, shoulder, and elbow accounting for most of the remaining cases. Patients usually report pain and swelling. Joint effusion, tenderness, limited motion in the joint, and a soft tissue mass are common clinical findings, occasionally mistaken for arthritis.
Three phases of articular disease have been identified: an initial phase, characterized by metaplastic formation of cartilaginous nodules in the synovium; a transitional phase, characterized by detachment of those nodules and formation of free intra-articular bodies; and an inactive phase, in which synovial proliferation has resolved but loose bodies remain in the joint, usually with variable amounts of joint fluid.
Gross pathologic findings consist of multiple blue/white ovoid nodules within synovial tissue (Fig. 11.1). By microscopy, these nodules are covered by fibrous tissue with synovial lining and are highly cellular, and the cells themselves may exhibit a moderate pleomorphism, with occasional plump and double nuclei (Figs. 11.2 and 11.3). The cartilaginous nodules, which often are undergoing calcification and endochondral ossification, may detach and become loose bodies. The loose bodies continue to be viable and may increase in size as they receive nourishment from the synovial fluid.
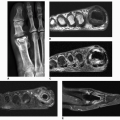
The imaging findings depend on the degree of calcification within the cartilaginous bodies, ranging from merely joint effusion to visualization of many radiopaque joint bodies, usually small and uniform in size (Figs. 11.4, 11.5, 11.6). The best proof that the bodies are indeed intraarticular is achieved by arthrography or computed tomography (CT) (Figs. 11.7 and 11.8). These modalities can visualize even noncalcified bodies. Magnetic resonance imaging (MRI) may also be helpful, although MRI appearance is variable and depends on the relative preponderance of synovial proliferation, loose bodies formation, and extent of calcification or ossification. Unmineralized hyperplastic synovial masses exhibit high signal intensity on T2-weighted images, whereas calcifications can be seen as signal void against the high-signal intensity fluid (Figs. 11.9 and 11.10). In addition to revealing loose bodies in the joint, CT and MRI may demonstrate bone erosion.
 Figure 11.1 ▪ Gross pathology of synovial (osteo)chondromatosis. Multiple blue/white ovoid nodules of cartilage are scattered within the synovial tissue. |
Synovial (osteo)chondromatosis should be differentiated from the secondary osteochondromatosis caused by osteoarthritis, particularly in the knee and hip joints. Distinguishing primary from secondary osteochondromatosis usually presents no problems. In the latter condition, there is invariably radiographic evidence of osteoarthritis with all of its typical features, such as narrowing of the radiographic joint space, subchondral sclerosis, and, occasionally, periarticular cysts or cystlike lesions (see Figs. 5.44, 5.45, 5.46 and 5.48 and 5.50). The loose bodies are fewer, larger, and invariably of different sizes (see Fig. 5.36). Conversely, in primary synovial (osteo) chondromatosis the joint is not affected by any degenerative changes. In some cases, however, the bone may show erosions secondary to pressure of the calcified bodies on the outer aspects of the cortex. The intra-articular bodies are numerous, small, and usually of uniform size (see Figs. 11.4, 11.5, 11.6).
The other conditions that can radiologically mimic synovial chondromatosis include pigmented villonodular
synovitis (PVNS), synovial hemangioma, and lipoma arborescens. In pigmented villonodular synovitis (discussed in detail later in this chapter), the filling defects in the joint are more confluent and less distinct. MRI may show foci of decreased intensity of the synovium in all sequences because of the paramagnetic effects of deposition of hemosiderin (see Figs. 11.15, 11.16, 11.17). Synovial hemangioma usually presents as a single soft tissue mass. On MRI, T1-weighted images show that the lesion is either isointense or slightly higher (brighter) in signal intensity than surrounding muscles, but much lower in intensity than subcutaneous fat. On T2-weighted images, the mass is invariably much brighter than fat (see Figs. 11.22, 11.23, 11.24, 11.25, 11.26). Phleboliths and fibrofatty septa in the mass are common findings that show low-signal characteristics. Lipoma arborescens is a villous lipomatous proliferation of the synovial membrane. This rare condition usually affects the knee joint but has occasionally been reported in other joints, including the wrist and ankle. The disease has been variously reported to have a developmental, traumatic, inflammatory, or neoplastic origin, but its true cause is still unknown. The clinical findings include slowly increasing but painless synovial thickening as well as joint effusion with sporadic exacerbation. Imaging studies reveal a joint effusion occasionally
accompanied by various degrees of osteoarthritis (see Figs. 11.28, 11.29, 11.30). Histologic examination demonstrates complete replacement of the subsynovial tissue by mature fat cells and the formation of proliferative villous projections (see text below).
synovitis (PVNS), synovial hemangioma, and lipoma arborescens. In pigmented villonodular synovitis (discussed in detail later in this chapter), the filling defects in the joint are more confluent and less distinct. MRI may show foci of decreased intensity of the synovium in all sequences because of the paramagnetic effects of deposition of hemosiderin (see Figs. 11.15, 11.16, 11.17). Synovial hemangioma usually presents as a single soft tissue mass. On MRI, T1-weighted images show that the lesion is either isointense or slightly higher (brighter) in signal intensity than surrounding muscles, but much lower in intensity than subcutaneous fat. On T2-weighted images, the mass is invariably much brighter than fat (see Figs. 11.22, 11.23, 11.24, 11.25, 11.26). Phleboliths and fibrofatty septa in the mass are common findings that show low-signal characteristics. Lipoma arborescens is a villous lipomatous proliferation of the synovial membrane. This rare condition usually affects the knee joint but has occasionally been reported in other joints, including the wrist and ankle. The disease has been variously reported to have a developmental, traumatic, inflammatory, or neoplastic origin, but its true cause is still unknown. The clinical findings include slowly increasing but painless synovial thickening as well as joint effusion with sporadic exacerbation. Imaging studies reveal a joint effusion occasionally
accompanied by various degrees of osteoarthritis (see Figs. 11.28, 11.29, 11.30). Histologic examination demonstrates complete replacement of the subsynovial tissue by mature fat cells and the formation of proliferative villous projections (see text below).
Treatment of synovial chondromatosis usually consists of removal of the intra-articular bodies and synovectomy, but local recurrence is not uncommon.
PIGMENTED VILLONODULAR SYNOVITIS (PVNS)
PVNS is a locally destructive fibrohistiocytic proliferation, characterized by many villous and nodular synovial protrusions, which affects joints, bursae, and tendon sheaths. Jaffe, Lichtenstein, and Sutro first described PVNS in 1941 and used this name to identify the lesion because of its yellow-brown, villous, and nodular appearance. The yellow-brown pigmentation is caused by excessive deposits of lipid and hemosiderin. This condition can be diffuse or localized. When the entire synovium of the joint is affected, and when there is a major villous component, the condition is referred to as diffuse pigmented villonodular synovitis. When a discrete intra-articular mass is present, the condition is called localized pigmented villonodular synovitis. When the process affects the tendon sheaths, it is called localized giant cell tumor of the tendon sheaths. The diffuse form usually occurs in the knee, hip, elbow, or wrist and accounts for 23% of cases. The localized nodular form is often regarded as a separate entity. It consists of a single polypoid mass attached to the synovium. Nodular tenosynovitis is most often seen in the fingers and is the second most common soft tissue tumor of the hand, exceeded only by the ganglion. In the new (2002) revised classification of soft tissue tumors, the World Health Organization (WHO) classifies localized intra-articular and extra-articular lesions as giant cell tumor of tendon sheath, whereas diffuse intra-articular and extra-articular forms are categorized as diffuse-type giant cell tumor (keeping PVNS as a synonym).
Both the diffuse and the localized form of villonodular synovitis usually occur as a single lesion, mainly in young and middle-aged individuals of either gender, with peak incidence in the third and fourth decades. One of the most characteristic findings in PVNS is the ability of the hyperplastic synovium to invade the subchondral bone, producing cysts and erosions. Although the cause is unknown and is often controversial, some investigators have suggested an autoimmune pathogenesis. Trauma is also a suspected cause, because similar effects have been produced experimentally in animals by repeated injections of blood into the knee joint. Some investigators have suggested a disturbance in lipid metabolism as a causative factor. It has also been postulated by Jaffe and colleagues that these lesions may represent an inflammatory response to an unknown agent. Ray, Stout, and Lattes contended that they are true benign neoplasms. Although the latter theory was presumed to be supported by pathologic studies indicating that the histiocytes present in PVNS may function as facultative fibroblasts and that foam cells may derive from histiocytes, thus relating PVNS to a benign neoplasm of fibrohistiocytic origin, these findings do not constitute definite proof that PVNS is a true neoplasm. They are rather indicative of a special form of a chronic proliferative inflammation process, as has already been postulated by Jaffe and colleagues.
Gross pathologic examination shows tan-colored or reddish-brown synovial mass with hypertrophic villi (Fig. 11.11). On histopathologic examination, PVNS reveals a tumor-like proliferation of the synovial tissue. A dense infiltration of mononuclear histiocytes is observed, accompanied by plasma cells, xanthoma cells, lymphocytes, and variable numbers of giant cells (Fig. 11.12). Long-standing lesions show fibrosis and hyalinization.
Clinically, PVNS is a slowly progressive process that manifests as mild pain and joint swelling with limitation of motion, mimicking arthritis. Occasionally, increased skin temperature is noted over the affected joint. The knee joint is most commonly affected and 66% of patients present with a bloody joint effusion. In fact, the presence of a serosanguinous synovial fluid in the absence of a history of recent trauma should strongly suggest the diagnosis of PVNS. The synovial fluid contains elevated levels of cholesterol, and fluid reaccumulates rapidly after aspiration. Other joints may be affected, including the hip, ankle, wrist, elbow, and shoulder. There is a 2:1 predilection for females. Patients range from 4 to 60 years of age, with a peak incidence in the third and fourth decades. The duration of symptoms can range from 6 months to as long as 25 years.
Recently, attention has been drawn to the extra-articular form of diffuse PVNS, also referred to as diffuse-type giant cell tumor. This condition is characterized by the presence of an infiltrate and extra-articular mass with or without involvement of the adjacent joint. This presentation of PVNS
creates a real diagnostic challenge for both radiologist and pathologist because its extra-articular location, invasion of the osseous structures, and more varied histologic infiltrative pattern may suggest malignancy.
creates a real diagnostic challenge for both radiologist and pathologist because its extra-articular location, invasion of the osseous structures, and more varied histologic infiltrative pattern may suggest malignancy.
Radiography reveals a soft tissue density in the affected joint, frequently interpreted as joint effusion. However, the density is greater than that of simple effusion, and it reflects not only a hemorrhagic fluid but also lobulated synovial masses (Fig. 11.13). A marginal, well-defined erosion of subchondral bone with a sclerotic margin may be present (incidence reported from 15% to 50%), usually on both sides of the affected articulation. Narrowing of the joint space has also been reported. In the hip, multiple cystlike or erosive areas involving non-weight-bearing regions of the acetabulum, as well as the femoral head and neck, are characteristic. Calcifications are encountered only in exceptional cases.
Arthrography reveals multiple lobulated masses with villous projections, which appear as filling defects in the contrast-filled suprapatellar bursa (Fig. 11.14). CT effectively demonstrates the extent of the disease. The increase in iron content of the synovial fluid results in high Hounsfield values, a feature that can help in the differential diagnosis. MRI is extremely useful in making a diagnosis, because on T2-weighted images the intra-articular masses demonstrate a combination of high-signal intensity areas,
representing fluid and congested synovium, interspersed with areas of intermediate-to-low signal intensity, secondary to random distribution of hemosiderin in the synovium (Fig. 11.15). In general, MRI shows a low signal on T1- and T2-weighted images because of hemosiderin deposition and thick fibrous tissue (Figs. 11.16, 11.17, 11.18). In addition, within the mass, signals consistent with fat can be noted, which are caused by clumps of lipid-laden macrophages.
Other MRI findings include hyperplastic synovium and occasionally bone erosions (see Figs. 11.15A,B and 11.16C). Administration of gadolinium in the form of Gd-DTPA leads to a notable increase in overall heterogeneity, which tends toward an overall increase in signal intensity of the capsule and septae. This enhancement of the synovium allows it to be differentiated from the fluid invariably present, which does not enhance (Fig. 11.18D). Apart from its diagnostic effectiveness, MRI is also useful in defining the extent of the disease.
representing fluid and congested synovium, interspersed with areas of intermediate-to-low signal intensity, secondary to random distribution of hemosiderin in the synovium (Fig. 11.15). In general, MRI shows a low signal on T1- and T2-weighted images because of hemosiderin deposition and thick fibrous tissue (Figs. 11.16, 11.17, 11.18). In addition, within the mass, signals consistent with fat can be noted, which are caused by clumps of lipid-laden macrophages.
Other MRI findings include hyperplastic synovium and occasionally bone erosions (see Figs. 11.15A,B and 11.16C). Administration of gadolinium in the form of Gd-DTPA leads to a notable increase in overall heterogeneity, which tends toward an overall increase in signal intensity of the capsule and septae. This enhancement of the synovium allows it to be differentiated from the fluid invariably present, which does not enhance (Fig. 11.18D). Apart from its diagnostic effectiveness, MRI is also useful in defining the extent of the disease.
The most common differential diagnostic possibilities include hemophilic arthropathy, synovial chondromatosis, synovial hemangioma, and synovial sarcoma. MRI is very effective in distinguishing these entities because it can reveal hemosiderin deposition in PVNS. Although this feature may also be present in hemophilic arthropathy, detection of diffuse hemosiderin clumps, synovial irregularity and thickening, and distention of the synovial sac favors the diagnosis of PVNS. In addition, hemophilia, unlike PVNS, commonly affects multiple joints and is associated with growth disturbance at the articular ends of the affected bones. Synovial chondromatosis may manifest with pressure erosions of the bone similar to those of PVNS. However, it can be distinguished by the presence of multiple joint bodies, calcified or uncalcified. Synovial hemangioma is commonly associated with the formation of phleboliths. Synovial sarcoma tends to have a shorter T1 and longer T2 on MRI compared with PVNS, and when calcifications are present, the latter diagnosis can be excluded.
Treatment usually consists of surgical open or arthroscopic synovectomy. Occasionally, intra-articular radiation synovectomy is used when the abnormal synovial tissue is <5 mm thick. Recently, reports appeared of postsynovectomy adjuvant treatment with external beam radiation therapy or intraarticular injection of radioactive material such as yttrium-90 (90Y). Local recurrence is not uncommon and is reported in ˜50% of cases.
SYNOVIAL HEMANGIOMA
Synovial hemangioma is a rare benign lesion that most commonly affects the knee joint, usually involving the anterior compartment. This lesion has also been found in the elbow, wrist, and ankle joints, as well as in tendon sheaths. Most cases affect children and adolescents. Almost all patients with synovial hemangioma are symptomatic, frequently presenting with a swollen knee or with mild pain or limitation of movement in the joint. Sometimes, patients report a history of recurrent episodes of joint swelling and various degrees of pain of several years’ duration. Synovial hemangioma is
often associated with an adjacent cutaneous or deep soft tissue hemangioma. For this reason, some investigators classify knee joint lesions as intra-articular, juxta-articular, or intermediate, depending on the extent of involvement. Synovial hemangioma is frequently misdiagnosed. According to one estimate, a correct preoperative diagnosis is made in only 22% of cases.
often associated with an adjacent cutaneous or deep soft tissue hemangioma. For this reason, some investigators classify knee joint lesions as intra-articular, juxta-articular, or intermediate, depending on the extent of involvement. Synovial hemangioma is frequently misdiagnosed. According to one estimate, a correct preoperative diagnosis is made in only 22% of cases.
Originating in the subsynovial layer mesenchyme of the synovial membrane, synovial hemangioma is a vascular lesion that contains variable amounts of adipose, fibrous, and muscle tissue, as well as thrombi in the vessels. When the lesion is completely intra-articular, it is usually well circumscribed and apparently encapsulated, attached to the synovial membrane by a pedicle of variable size, and adherent to the synovium on one or more surfaces by separable adhesions. Grossly, the tumor is a lobulated soft, brown, doughy mass with overlying villous synovium that is often stained mahogany brown by hemosiderin (Fig. 11.19). On microscopic examination, the lesion exhibits arborizing vascular channels of different sizes and a hyperplastic overlying synovium, which may show abundant iron deposition in chronic cases with repeated hemarthrosis (Fig. 11.20).
Until recently, synovial hemangiomas were evaluated by a combination of conventional radiography, arthrography, angiography, and contrast-enhanced CT. Although radiographs appear normal in at least half of the patients, they may reveal soft tissue swelling, a mass around the joint, joint effusion, or erosions (Fig. 11.21). Phleboliths, periosteal thickening, advanced maturation of the epiphysis, and arthritic changes are also occasionally noted on conventional radiographs. Arthrography usually shows nonspecific filling defects with a villous configuration. Angiograms yield much more specific information than radiography. They can often reveal a vascular lesion and can demonstrate pathognomonic features of hemangioma. Contrast-enhanced CT of the joint typically reveals a heterogeneous-appearing soft tissue mass that displays tissue attenuation approximating that of skeletal muscle and containing areas of decreased attenuation, some approaching that of fat. CT is effective for demonstrating phleboliths and revealing patchy enhancement around them, as well as enhancement of tubular areas and contrast pooling within the lesion. In some cases, CT reveals enlarged vessels feeding and draining the mass, as well as enlarged adjacent subcutaneous veins.
At present, MRI has become the modality of choice for the evaluation of hemangiomas because, with this modality, a presumptive diagnosis can be made. The soft tissue mass typically exhibits an intermediate signal intensity on T1-weighted sequences, appearing isointense with or slightly brighter than muscle but much less bright than fat. The mass is usually much brighter than subcutaneous fat on T2-weighted images and on fat suppression sequences (Figs. 11.22, 11.23, 11.24) and shows thin, often serpentine, low-intensity septa within it (Fig. 11.25). In general, the signal intensity characteristics of hemangiomas appear to be related to a number of factors, including slow flow, thrombosis, vessel occlusion, and stagnant blood that pools in larger vessels and dilated sinuses, as well as to the variable amounts of adipose tissue in the lesion. After intravenous
injection of gadolinium, there is evidence of enhancement of the hemangioma. In patients with a cavernous hemangioma of the knee, fluid-fluid levels are also observed (Fig. 11.26), a finding recently reported also in soft tissue hemangiomas of this type.
injection of gadolinium, there is evidence of enhancement of the hemangioma. In patients with a cavernous hemangioma of the knee, fluid-fluid levels are also observed (Fig. 11.26), a finding recently reported also in soft tissue hemangiomas of this type.
The differential diagnosis of synovial hemangioma includes PVNS and synovial chondromatosis. All proliferative chronic inflammatory processes, such as rheumatoid arthritis, tuberculous arthritis, and hemophilic arthropathy, should also be considered in the differential diagnosis, but these conditions, when involving the knee, can usually be distinguished clinically. Because it is extremely uncommon, lipoma arborescens is rarely included in the differential diagnosis. MRI is diagnostic for the latter condition, showing typical frondlike projections of the lesion and fat characteristics (bright on T1- and intermediate on T2-weighted images). In PVNS, radiography commonly reveals findings similar to those of synovial hemangioma, such as joint effusion and a mass in the suprapatellar bursa or popliteal fossa region. Radiographs may also demonstrate bone erosions on both sides of the joint. MRI, however, is usually diagnostic for PVNS, demonstrating that the synovium exhibits nodular thickening and masses of heterogeneous signal intensity. Most of the lesion will display a higher signal intensity than muscle on both T1- and T2-weighted sequences, with other portions exhibiting a low signal intensity on all sequences, reflecting the hemosiderin content of the tumor. Synovial chondromatosis can be distinguished from synovial hemangioma if radiography shows calcified bodies. Intra-articular osteochondral fragments of uniform size are almost pathognomonic for this condition. CT may be helpful in demonstrating faint calcifications not otherwise seen.
LIPOMA ARBORESCENS
Lipoma arborescens, also known as villous lipomatous proliferation of the synovial membranes, is a rare intra-articular disorder characterized by nonneoplastic lipomatous proliferation of the synovium. The term “arborescens” (from the Latin word arbor, meaning tree) describes the characteristic treelike morphology of the hypertrophied
synovium, which exhibits a frondlike appearance. The term “lipoma” is a misnomer, because there is no focal mass. It has been suggested that a more appropriate term for this condition would be synovial lipomatosis. Lipoma arborescens may be monoarticular or polyarticular. The cause of this disorder remains uncertain, although association with osteoarthritis, rheumatoid arthritis, psoriasis, and diabetes mellitus has been postulated. This lesion most commonly affects the knee joint, although involvement of other joints, such as shoulder, hip, wrist, elbow, and ankle, has been sporadically reported by various authors. Occasionally, this condition may affect multiple joints. There have been also sporadic reports of bursae and tendon sheaths involvement. It is more prevalent in males, usually between the fourth and seventh decades. These patients present with slowly increasing but painless joint effusion accompanied by synovial thickening.
synovium, which exhibits a frondlike appearance. The term “lipoma” is a misnomer, because there is no focal mass. It has been suggested that a more appropriate term for this condition would be synovial lipomatosis. Lipoma arborescens may be monoarticular or polyarticular. The cause of this disorder remains uncertain, although association with osteoarthritis, rheumatoid arthritis, psoriasis, and diabetes mellitus has been postulated. This lesion most commonly affects the knee joint, although involvement of other joints, such as shoulder, hip, wrist, elbow, and ankle, has been sporadically reported by various authors. Occasionally, this condition may affect multiple joints. There have been also sporadic reports of bursae and tendon sheaths involvement. It is more prevalent in males, usually between the fourth and seventh decades. These patients present with slowly increasing but painless joint effusion accompanied by synovial thickening.
Histopathologically, lipoma arborescens is characterized by hyperplasia of subsynovial fat, formation of mature fat cells, and the presence of proliferative villous projections (Fig. 11.27). Osseous and chondroid metaplasia can occur.
Imaging studies, particularly MRI, are very characteristic and allow definite diagnosis of this condition. Joint effusion is invariably present, associated with frondlike masses arising from the synovium that have the signal intensity of fat on all imaging sequences (Figs. 11.28, 11.29, 11.30). Occasionally, a chemical shift artifact is present at the fat-fluid interface.
Differential diagnosis should include PVNS, synovial chondromatosis, synovial hemangioma, hemophilic arthropathy, and a variety of intra-articular inflammatory conditions.
Treatment usually consists of surgical open or arthroscopic synovectomy.
 Figure 11.27 ▪ Histopathology of lipoma arborescens. Synovial villi are distended by mature adipocytes located in subsynovial connective tissue (H&E, original magnification ×50).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|