Abstract
Objective
No clinical standard exists for intraoperative fetal cardiac monitoring during maternal-fetal surgery for fetal myelomeningocele (fMMC). This pilot study explores the feasibility of using speckle tracking echocardiography (STE)-derived functional measurements to characterize cardiac performance throughout fetoscopic fMMC and compares these measures with other common intraoperative cardiac function parameters.
Methods
Continuous fetal echocardiography was performed during fetoscopic fMMC repair with fetal heart rate assessment every 2 minutes and a 4-chamber cine clip and mitral and tricuspid Doppler inflow patterns captured every 5 minutes. Offline postprocessing was used to measure functional data during fetal surgery including left ventricle (LV) global longitudinal strain (GLS), right ventricle (RV) GLS, LV ejection fraction (EF), and RV fractional area of change (FAC). Interrater agreement was determined for all measurements.
Results
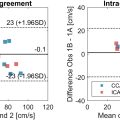
Intraoperative fMMC echocardiograms were successfully obtained and analyzed for twenty patients. LV and RV GLS remained stable with a population average of -25.9±2.6% and -23.1±2.0% respectively during fMMC, and comparable to published normative ranges. Cardiac systolic and diastolic function was preserved at all surgical stages as demonstrated by LV EF, RV FAC, and spectral Doppler measurements. Interrater agreement for the spectral Doppler measurements was high, whereas STE agreement was low.
Conclusion
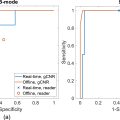
Fetal cardiac image acquisition for STE analysis was feasible during all stages of fetoscopic fMMC repair. Poor interrater agreement and offline post-processing limit the utility of STE for real-time clinical assessment, yet with experienced operators it could serve as a useful tool for scientific innovation to better understand modifiers of intraoperative fetal cardiac function.
Introduction
In-utero surgical repair of fetal myelomeningocele (fMMC) aims to improve patient outcomes, but intraoperative fetal distress and rare incidences of delivery and loss have been reported [ , ]. Surgical teams currently rely on real-time changes in ultrasound-observed fetal heart rate (FHR) to anticipate fetal distress and initiate resuscitative interventions [ – ]. Fetal bradycardia and spectral Doppler abnormalities are common intraprocedural ultrasound findings, particularly in fetoscopic fMMC procedures [ ]. However, FHR fluctuations are typically transient and the sensitivity of FHR to detect clinically significant cardiac dysfunction is poorly characterized with limited evidence that FHR predicts early fetal distress [ ]. To date, no evidence-based standard exists for intraoperative fMMC surveillance, and anesthesia management and fetal monitoring techniques vary widely between centers [ ].
Two-dimensional speckle tracking echocardiography (STE) is a noninvasive imaging method for quantifying cardiac function [ – ]. STE-measured global longitudinal strain (GLS) parameterizes cardiac performance and has been hypothesized to detect subclinical cardiac dysfunction before the FHR is affected [ ]. STE has been incorporated into clinical cardiology practice in select adult and pediatric populations, but fetal cardiac strain assessment has yielded mixed results due to the heightened complexity of fetal imaging, in-utero cardiac maturational changes, and variability in reader training and experience [ , , ]. While transabdominal fetal STE is feasible [ , ], it can be difficult to acquire a high-quality, high-frame-rate 4-chamber cine clip depending on the fetus’ orientation and positioning [ ], and the maternal abdominal wall is signal attenuating [ ]. Fetal movement reduces image quality and strain analysis accuracy, and strain characteristics evolve throughout gestation with high variability between patients [ , – ]. These factors collectively impact the practical clinical use of strain analysis for fetal monitoring, but the controlled setting of an fMMC procedure (reduced fetal movement due to anesthesia, improved transuterine imaging, narrow gestational age at surgery) provides a unique opportunity to explore the utility of STE-based intraprocedural fetal cardiac assessment [ , ].
In this pilot study, we primarily sought to determine the feasibility of reliably acquiring quality fetal cardiac images during fetoscopic fMMC repairs and performing offline measures of STE-based cardiac performance using previously acquired fMMC fetal echo images. Secondly, we aimed to perform a comparison of STE-based and traditional fetal cardiac performance parameters and evaluate interrater reproducibility.
Methods
This observational study included fetoscopic patients who underwent fMMC repair between 23 and 26 weeks estimated gestational age (EGA) at the Midwest Fetal Care Center between December 1, 2020 and September 30, 2022. The study protocol was approved with a waiver of consent by the Institutional Review Board (IRB) at both Allina Health (#1708950) and Children’s Minnesota (#2021-014).
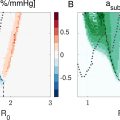
The fMMC procedure used a three-port (5 mm) fetoscopic closure technique including fetal placode dissection, creation and closure of a myofascial flap, and skin closure. Amnioreduction followed by CO 2 insufflation (6–8 mmHg) was performed in all cases. The anesthesia protocol for all cases included maternal propofol induction with inhaled sevoflurane and intravenous magnesium sulfate administration for uterine tocolysis. A minimum alveolar concentration (MAC) of 1.5 was set at uterine exposure and maintained until the fMMC repair was complete. Throughout each procedure, maternal systolic blood pressure was maintained above 120 mmHg with a phenylephrine infusion and/or ephedrine administration as needed, and the fraction of inspired oxygen (FiO 2 ) was maintained above 40%.
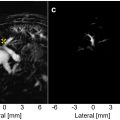
Continuous ultrasonography was performed during all fMMC procedures by a maternal-fetal medicine specialist dedicated to holding the probe and an on-site pediatric cardiologist who captured and interpreted the images in real-time. To optimize image quality, the probe was positioned directly on the uterus with the imaging window adjusted for fetal/uterine/placental position and surgical field. Probe movement and pressure were minimized to not interfere with placental or fetal blood flows. The clinical protocol for fetal cardiac monitoring included FHR every 2 minutes, a 4-chamber clip (goal frame rate >70 frames per second (fps)) and tricuspid valve (TV) and mitral valve (MV) spectral Doppler inflow tracings every 5 min. The cardiac function and anesthesia parameters were analyzed at each of the five fMMC surgical stages: (i) baseline at anesthesia induction, (ii) uterine entry (iii) port entry and placement, (iv) fetal surgical repair, (v) and port closure. A Philips Epiq 7 (Philips Healthcare, Andover, MA, USA) ultrasound machine was used in the first 7 operative cases and a GE Voluson Expert 22 (GE Healthcare Ultrasound, Milwaukee, WI, USA) was used for the remaining 13 cases. A 2-9 MHz curvilinear transducer was used for all procedures.
Using the acquired intraoperative 4-chamber cine clips, a fetal cardiac sonographer (TG) performed offline speckle tracking measurements of left ventricular (LV) and right ventricular (RV) GLS, LV ejection fraction (EF), and RV fractional area of change (FAC) using TomTec software (Image Arena version 51.00, Germany). The same 4-chamber clips were also used for calculating LV EF by Simpson’s single plane method. Indexed MV and TV inflow durations were calculated (inflow duration/cardiac cycle duration, 3 measurement averages) and FHRs throughout the procedure were measured and recorded offline by a fetal cardiologist (LH).
Interrater reproducibility of both STE and spectral Doppler parameters were tested, measuring one of each parameter per patient, by a second blinded fetal cardiologist (CP). Descriptive statistics were used to describe the study population demographics, surgical characteristics, and fetal cardiac function and anesthesia throughout the procedure. LV and RV GLS values were compared to normative ranges in the literature for healthy fetuses at a similar gestation range. We describe the interrater reproducibility of the cardiac performance parameters using interclass correlation coefficients (ICC) and a Bland Altman Analysis for two raters.
Results
A total of 20 fetoscopic fMMC closures occurred during the study period. Table 1 summarizes the maternal-fetal demographics and surgery characteristics. The mean patient age was 32 years (range 18–41 years) with a wide BMI range (21.6–47.4). Sixty percent of patients were nulliparous, and 15% (3/20) had a history of prior uterine surgery (two Caesarean sections, one endometrial ablation). The average EGA at the time of the surgery was approximately 25 weeks (24.9 ± 0.6 weeks, range 23 wk 2 d to 26 wk 1 d).
| Characteristic | Patients n = 20 |
|---|---|
| Age, years | 30.7 ± 7.0 |
| Gravity | 2.6 ± 2.4 |
| Nulliparous | 12 (60) |
| BMI | 31.7 ± 7.3 |
| Maternal race | |
| White | 17 (85) |
| Black | 3 (15) |
| EGA at surgery | 24.9 ± 0.6 |
| Lesion Type, myeloschisis | 7 (35) |
| Lesion level, highest | |
| L1-L2 | 3 (15) |
| L3-L4 | 10 (50) |
| L5-S1 | 7 (35) |
| Placenta Location, anterior | 9 (45) |
| Procedure length, min | |
| Total operative time, min | 236 ± 36 |
| Port-in time, min | 187 ± 33 |
| Fetal fMMC closure time, min | 124 ± 30 |
Ultrasound acquisition of high-quality echo images, including 4-chamber cine clips at adequate frame rates for cardiac performance analysis was possible in all 20 cases (example Fig. 1 ). A total of 542 cine clips were collected and analyzed for strain with 91.5% acquired at > 70 fps (overall median 84 fps). A median of 27 clips were analyzed per patient (range 10–62 clips, median of 93% of clips > 70 fps).

Table 2 presents the cardiac function and anesthesia parameter values for each stage of the fetoscopic fMMC procedure. LV and RV GLS remained stable across each stage of the procedure, ranging from -27.6% through -24.0% for the LV ( p = 0.684) and -25.1% through -23.1% for the RV ( p = 0.234) despite significant changes in FHR (p < 0.001) and indexed MV and TV inflow durations (both p < 0.001) during the procedure. The LV and RV GLS measurements for all patients during the fetal repair are plotted in Figure 2 . Overall, these values were consistent with the ranges published for healthy fetuses at similar gestational ages [ – ].
| Parameter | Baseline b | Uterine access | Port entry | Fetal surgery | Port closure | p -value |
|---|---|---|---|---|---|---|
| Cardiac function | ||||||
| FHR, bpm | 136.8 ± 6.3 | 122.4 ± 7.4 | 119.7 ± 9.7 | 121.5 ± 10.2 | 119.7 ± 8.4 | <0.001 a |
| LV GLS, % | −27.6 ± 3.8 | −27.3 ± 4.8 | −26.5 ± 3.5 | −25.9 ± 2.6 | −24.0 ± 6.4 | 0.684 |
| RV GLS, % | −25.1 ± 2.9 | −25.0 ± 3.8 | −23.6 ± 2.4 | −23.1 ± 2.0 | −24.8 ± 1.6 | 0.234 |
| LV GLS EF, % | 65.5 ± 2.2 | 65.2 ± 4.4 | 64.1 ± 2.5 | 63.9 ± 2.7 | 66.0 ± 6.2 | 0.318 |
| LV single plane EF, % | 66.1 ± 2.1 | 64.8 ± 2.1 | 64.4 ± 2.1 | 63.5 ± 2.5 | 67.0 ± 0.1 | 0.011 a |
| RV FAC, % | 42.6 ± 6.6 | 47.7 ± 7.9 | 43.0 ± 3.3 | 42.7 ± 3.1 | 42.6 ± 4.8 | 0.157 |
| Indexed MV | 0.437 ± 0.038 | 0.502 ± 0.036 | 0.508 ± 0.039 | 0.510 ± 0.051 | 0.478 ± 0.031 | <0.001 a |
| Indexed TV | 0.407 ± 0.040 | 0.473 ± 0.028 | 0.493 ± 0.042 | 0.498 ± 0.041 | 0.473 ± 0.022 | <0.001 a |
| Anesthesia | ||||||
| MAC | 0.07 ± 1.36 | 1.01 ± 0.27 | 1.46 ± 0.09 | 1.48 ± 0.09 | 1.21 ± 0.27 | − |
| Sevo expired | 0.25 ± 0.38 | 2.19 ± 0.62 | 3.11 ± 0.21 | 3.18 ± 0.21 | 2.62 ± 0.58 | − |
| Sevo inspired | 0.40 ± 0.62 | 3.12 ± 0.86 | 3.91 ± 0.38 | 3.73 ± 0.30 | 2.81 ± 0.79 | − |
| Inspired O 2 | 57.8 ± 15.1 | 58.2 ± 13.8 | 62.2 ± 16.0 | 63.1 ± 17.0 | 61.2 ± 16.5 | − |
| Systolic BP | 125.1 ± 9.8 | 126.1 ± 7.8 | 127. 7 ± 5.2 | 124.5 ± 6.4 | 125.7 ± 7.0 | − |
| Diastolic BP | 61.2 ± 4.8 | 63.4 ± 5.7 | 64.2 ± 5.9 | 60.0 ± 6.0 | 61.0 ± 7.8 | − |
| Mean ABP | 79.4 ± 6.5 | 82.2 ± 6.8 | 83.5 ± 6.8 | 79.1 ± 6.7 | 80.0 ± 9.2 | − |
| Maternal HR | 78.6 ± 12.9 | 76.3 ± 11.7 | 86.1 ± 12.2 | 87.7 ± 11.5 | 88.8 ± 9.6 | − |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree