Ultrasound
Susan J. Ackerman
Abid Irshad
Amy S. Campbell
Abbie Cluver
The authors and editors acknowledge the contribution of the Chapter 4 author from the second edition: Sunil Kini, MD and from the 3rd edition: Angelle Harper, MD.
Case 4.1
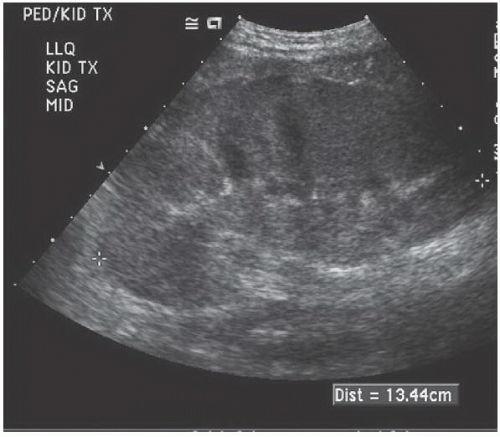
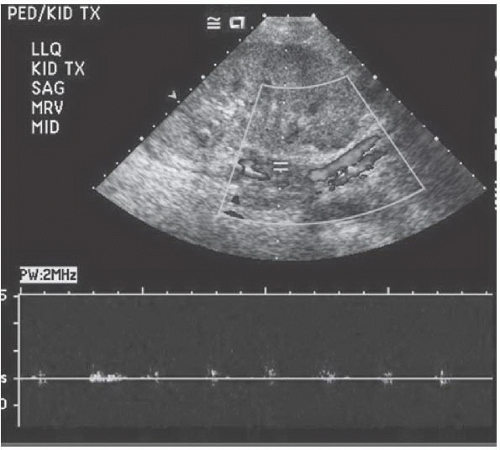
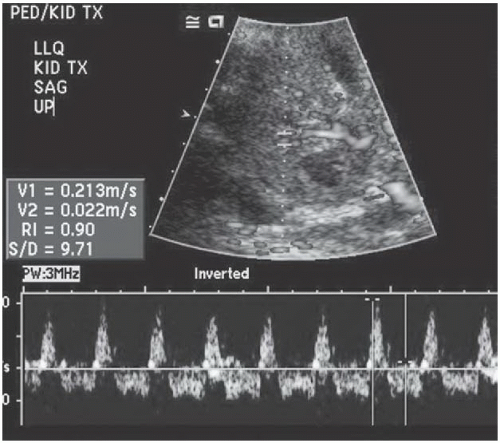
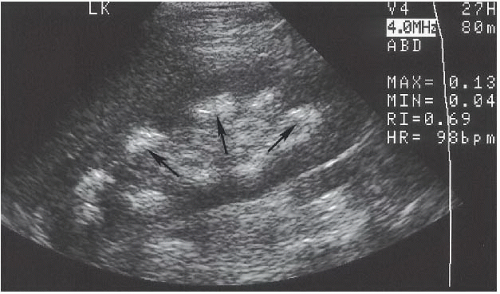
HISTORY: New kidney transplantation with pain and anuria
FINDINGS: Echogenic thrombus is noted in the main renal vein (Fig. 4.1.1). In addition, there is no flow on color and spectral Doppler waveforms (Fig. 4.1.2). Reversal of flow is noted in the intrarenal artery (Fig. 4.1.3).
DIAGNOSIS: Renal vein thrombosis in kidney transplantation
DISCUSSION: Renal vein thrombosis usually occurs in the acute postoperative period. It causes acute pain and swelling, in addition to anuria. The diagnostic criteria include gray-scale findings of thrombus within the main renal vein and absence of flow noted in the transplant vein with color Doppler (1). In addition, there is reversal of diastolic flow within the main renal artery and the intrarenal arteries. Rapid diagnosis and intervention such as thrombectomy are important to salvage the kidney. A nephrectomy may be the end point.
Aunt Minnie’s Pearls
The predominant symptom is anuria with pain.
Color Doppler ultrasound shows absence of flow in the main renal vein and reversal of diastolic flow in the main renal artery.
Case 4.2
HISTORY: Palpable thyroid nodule
FINDINGS: A well-defined hypoechoic solid mass with diffuse microcalcifications is noted (Fig. 4.2.1).
DIAGNOSIS: Papillary thyroid cancer
DISCUSSION: Papillary thyroid cancer is an epithelial cell cancer that accounts for approximately 80% of all thyroid cancers.
It is most prevalent in young females. The sonographic characteristics include hypoechogeniticity, microcalcifications, and hypervascularity.
The “snowstorm” appearance or diffuse microcalcifications in a hypoechoic nodule has been specifically described with papillary thyroid cancer. It commonly spreads to the cervical lymph nodes. The cervical lymph node metastasis may contain echogenic foci representing microcalcifications or cystic degeneration.
The mortality rate from papillary thyroid cancer after 20 years is approximately 6%.
Aunt Minnie’s Pearls
Papillary thyroid carcinoma is the most common type of thyroid cancer.
The classic appearance is a hypoechoic nodule with diffuse microcalcifications or “snowstorm” appearance.
Case 4.3
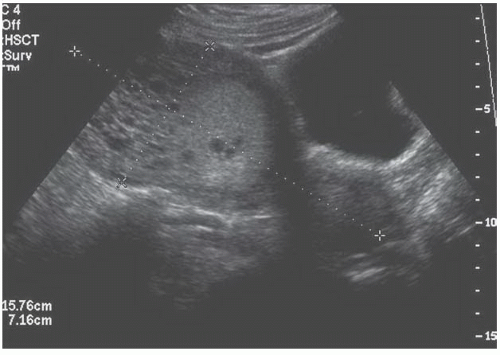
HISTORY: A 16-week pregnancy with hyperemesis and vaginal bleeding
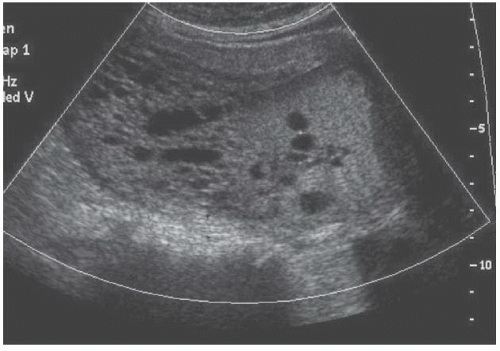
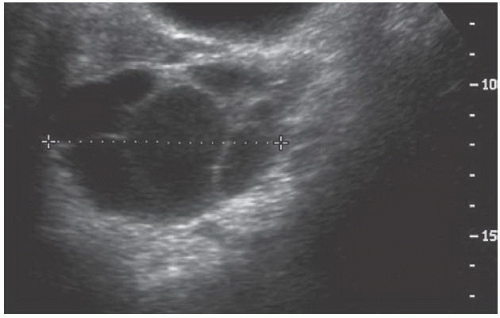
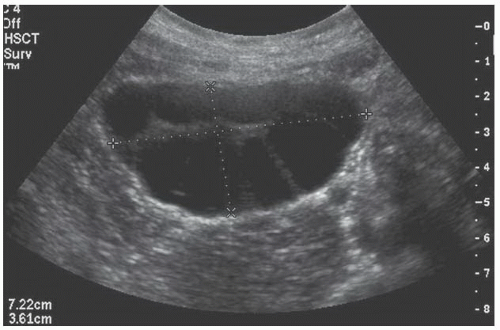
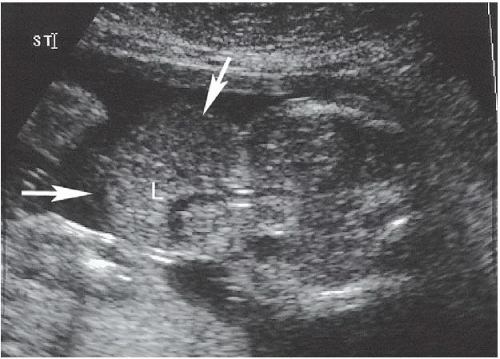
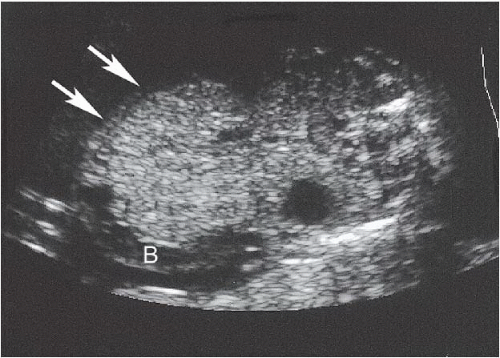
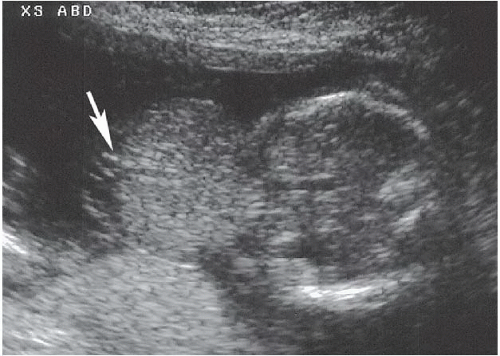
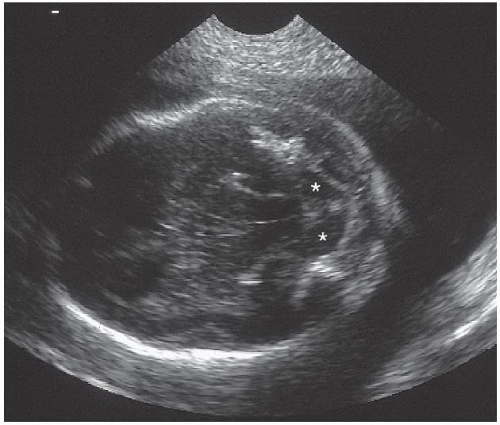
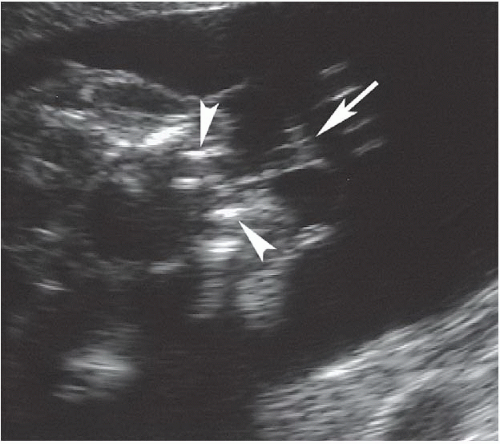
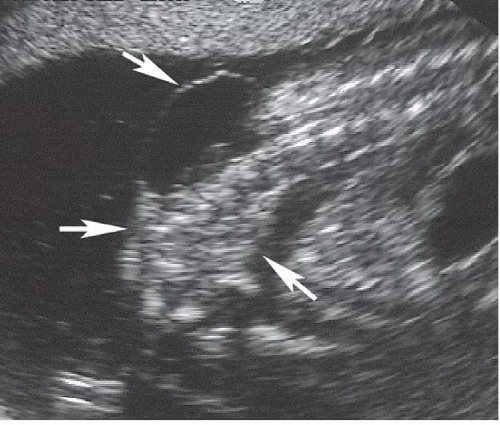
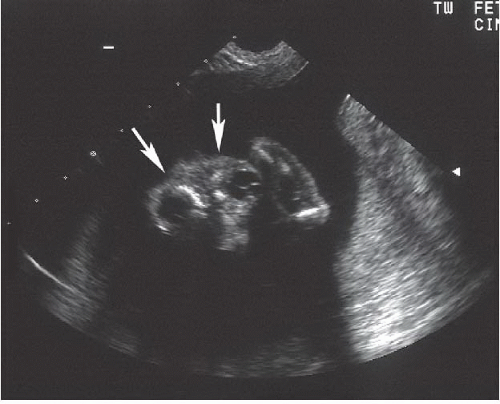
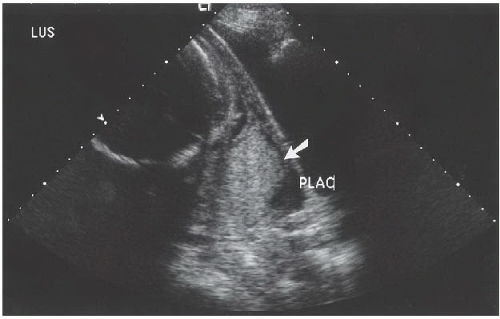
FINDINGS: Transabdominal evaluation of the gravid uterus reveals an echogenic, heterogeneous mass with multifocal small cystic spaces filling the endometrial canal (Figs. 4.3.1 and 4.3.2). In conjunction with this, the ovaries demonstrate frank enlargement with essential replacement by multiple, large cysts (Figs. 4.3.3 and 4.3.4).
DIAGNOSIS: Complete molar pregnancy with bilateral theca lutein cysts
DISCUSSION: Complete molar pregnancy is most often associated with a 46,XX karyotype supplied by all paternal chromosomes. At pathological evaluation, there is no associated fetal development, with only abnormal villi seen. Markedly elevated hCG resulting from excessive trophoblastic proliferation causes characteristic symptoms, including hyperemesis gravidarum. The most frequent presenting symptom is vaginal bleeding, seen in >90% of cases. Characteristic imaging features of complete molar pregnancy are as above with an echogenic mass containing multiple tiny cystic spaces representing hydropic villi within the abnormal tissue. Theca lutein cysts are an associated finding in 15% to 30% of complete moles as a result of hyperstimulation of the ovaries owing to excessive amounts of circulating serum hCG.
Aunt Minnie’s Pearls
Twenty percent of complete molar pregnancies will develop persistent gestational trophoblastic disease. This includes invasive mole, choriocarcinoma, and placental site trophoblastic tumor.
Theca lutein cysts are a result of hyperstimulation and are seen in the setting of molar pregnancy and assisted fertility. These can undergo hemorrhage, rupture, and torsion.
Case 4.4
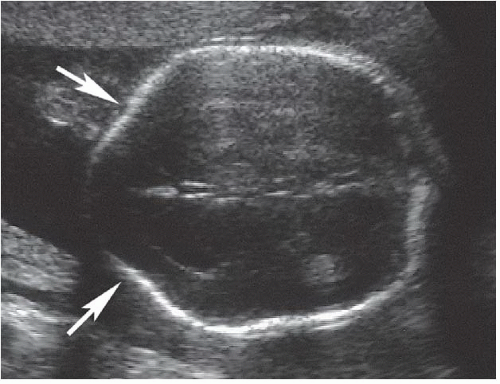
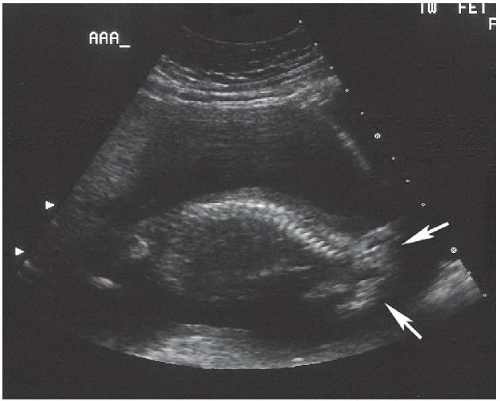
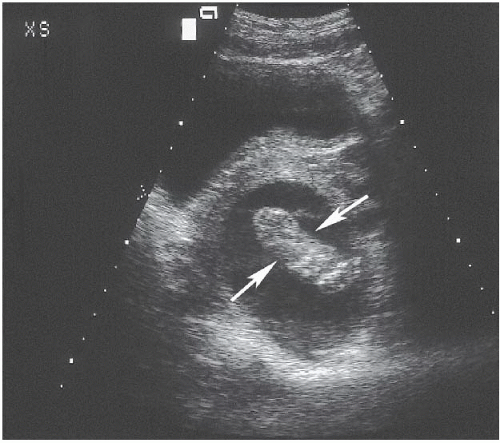
HISTORY: A 30-week pregnancy with suspected twin gestation and no prior prenatal care
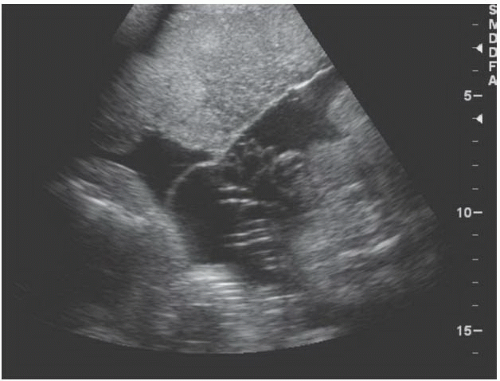
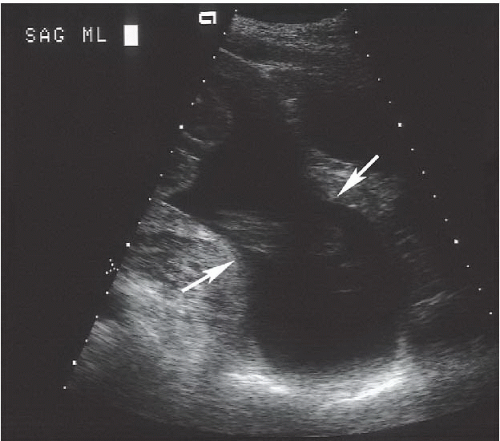
FINDINGS: Sonographic evaluation of the gravid uterus demonstrates two fused anteriorly located placentas with a thick intertwin membrane. A triangular piece of placental tissue can be seen to extend into this membrane where it tapers sharply (Fig. 4.4.1).
DIAGNOSIS: Dichorionic twin pregnancy (the twin peak sign)
DISCUSSION: Determination of chorionicity and amnionicity is a primary goal of obstetric ultrasound in multiple gestations as this dramatically effects prognosis (2). Best seen at approximately 10 to 14 weeks’ gestational age, the “twin peak” or “lambda” sign is an extremely specific sign of dichorionicity, regardless of the stage at which it is detected (3). However, as the pregnancy progresses, the interdigitating placental villi will regress, and this becomes progressively less evident, with variable persistence and visibility into the later stages of pregnancy (4).
Aunt Minnie’s Pearls
An easily seen intertwin membrane with extension of chorion/placenta into it = dichorionic pregnancy.
Absence of twin peak sign is not helpful in late second and third trimester as it is inconsistently seen later in pregnancy.
Case 4.5
HISTORY: A 45-year-old male presents with history of chronic scrotal discomfort
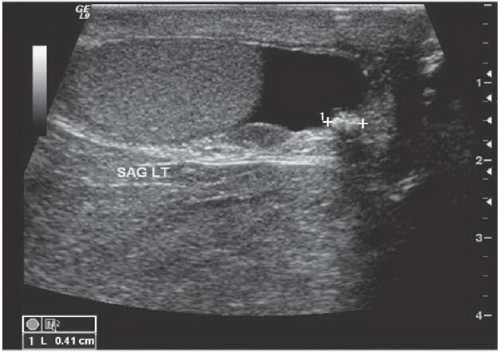
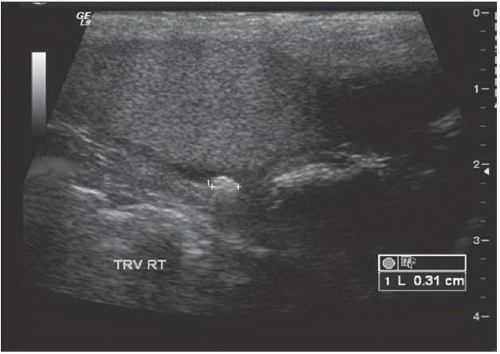
FINDINGS: A transverse image through the left scrotum (Fig. 4.5.1) and a longitudinal image through the right scrotum (Fig. 4.5.2) show normal appearance to the testicles. Both sides show an echogenic focus in the tunica vaginalis cavity outside the testicle that demonstrates posterior acoustic shadow suggesting a calcified lesion. Presence of fluid makes it easily visible.
DIAGNOSIS: Scrotoliths or scrotal pearls
DISCUSSION: Scrotoliths occur as calcifications within the layers of tunica vaginalis that are usually seen as an incidental finding. This is a benign entity and has no association with testicular cancer as opposed to testicular microlithiasis, which has been associated with testicular malignancy. The scrotoliths may be associated with previous trauma or inflammation and have been more commonly seen in mountain bikers, likely from repetitive scrotal trauma. There are various theories regarding their formation. These may form by deposition of calcium on a nidus that may result either from inflammation or torsion of the appendix testis or epididymal appendage (5,6). Macroscopically, these masses are usually seen as rubbery, white, rounded loose bodies. Microscopically, these are a mixture of fibrinoid material and calcium and usually contain a central nidus.
Clinically, these patients are usually asymptomatic; however, they may occasionally feel these as palpable nodules. These are usually seen as an incidental finding on ultrasound. Ultrasound usually demonstrates single or multiple extra-testicular stones within the layers of the tunica vaginalis that may be freely mobile, especially in the presence of hydrocele. These are frequently seen in association with hydrocele, and presence of fluid also makes it easy to identify these stones. The diagnosis is usually straightforward as these usually have a typical appearance. Other causes of extra-testicular calcifications include epididymal calcification seen in chronic epididymitis, tuberculosis, and schistosomiasis.
Aunt Minnie’s Pearls
Single or multiple extra-testicular, usually mobile, calcified masses (scrotoliths) occur between the layers of tunica vaginalis.
These are not associated with testicular neoplasms and are usually of no clinical significance.
Case 4.6
HISTORY: A 34-year-old gravid woman (estimated gestational age of 22.5 weeks) with maternal serum alpha-fetoprotein level of 5.3 multiples of the median
FINDINGS: A 3.5-cm defect of the ventral aspect of the fetal anterior abdominal wall can be seen on these transverse views of the fetal abdomen. Through this defect protrudes a solid mass of approximately 4 cm in diameter (Fig. 4.6.1, arrows). This mass contains liver (L) and bowel (B) and is covered by a thin membrane (Fig. 4.6.2, arrows). Figure 4.6.3 reveals that the umbilical cord inserts into the mass (arrow).
DIAGNOSIS: Omphalocele
DISCUSSION: Omphaloceles (exomphalos) occur in 1 of 4,000 live births and are usually detected during routine sonographic examination of the fetal abdomen or in the workup for elevated alpha-fetoprotein levels. The defect consists of herniation of abdominal contents into the base of the umbilical cord. The cord inserts into the apical-caudal aspect
of the mass, unlike gastroschisis, in which the cord inserts normally into the abdominal wall. Although the delineating peritoneal—amniotic membrane is not always easily visible, its presence can be inferred from the smooth surface of the herniated mass. This should be contrasted to gastroschisis, in which there is no delineating membrane and the loops of bowel float freely within the amniotic cavity. The presence of liver within an omphalocele can be inferred by the homogeneous appearance of the herniated mass, the presence of intrahepatic vessels, and the large size of the defect (789).
of the mass, unlike gastroschisis, in which the cord inserts normally into the abdominal wall. Although the delineating peritoneal—amniotic membrane is not always easily visible, its presence can be inferred from the smooth surface of the herniated mass. This should be contrasted to gastroschisis, in which there is no delineating membrane and the loops of bowel float freely within the amniotic cavity. The presence of liver within an omphalocele can be inferred by the homogeneous appearance of the herniated mass, the presence of intrahepatic vessels, and the large size of the defect (789).
Associated anomalies have been reported in 67% to 88% of fetuses with omphalocele identified prenatally. These anomalies include karyotype abnormalities and nonchromosomal structural anomalies. Chromosome abnormalities have been more strongly associated with small omphalocele sacs that do not contain liver.
Aunt Minnie’s Pearls
Herniation of abdominal contents into the base of the umbilical cord = omphalocele.
Small omphaloceles that do not contain liver have a stronger association with chromosomal abnormalities than larger omphaloceles.
Associated anomalies have been reported in up to 88% of fetuses with omphalocele.
Case 4.7
HISTORY: A 32-year-old gravid woman with maternal serum alpha-fetoprotein of 2.6 multiples of the median
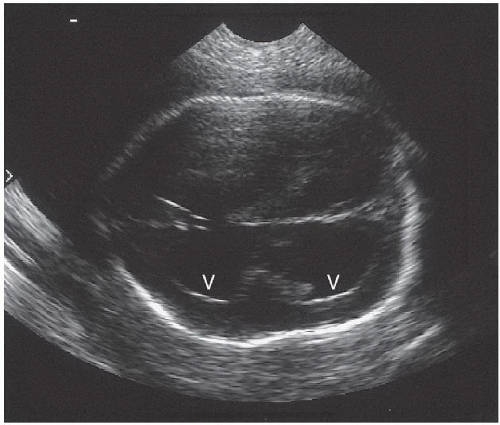
FINDINGS: Classic “banana sign” (i.e., obliteration of posterior fossa and curved appearance of the herniated cerebellum; Fig. 4.7.1, asterisks) and “lemon sign” (i.e., abnormal bifrontal concavity; Fig. 4.7.2, arrows) are seen in the cranium of this fetus of 20 weeks’ gestation. Mild ventriculomegaly (V) is present (Fig. 4.7.3), and the lateral ventricles measure 13 mm (up to 10 mm is normal). Axial (Fig. 4.7.4) and sagittal (Fig. 4.7.5) views of the spine demonstrate the flared laminae (Fig. 4.7.4, arrowheads), which are diagnostic of spina bifida and the associated meningomyelocele (Figs. 4.7.4 and 4.7.5, arrows) extending from approximately L3 through S3. Bilateral clubfeet were also present (only the right foot is shown; Fig. 4.7.6).
DIAGNOSIS: Chiari II (Arnold-Chiari) malformation and associated meningomyelocele
DISCUSSION: Open neural tube defects are the most common central nervous system malformations (10,11). Direct visualization of a meningomyelocele may be difficult, however, and even the most skilled examiner may worry about false-negative results. Fortunately for the sonographer, meningomyeloceles are almost always accompanied by the
Arnold-Chiari malformation, which has more easily recognizable cranial findings. They include obliteration of the cisterna magna, the lemon sign, ventricular dilatation, and a disproportionately small biparietal diameter.
Arnold-Chiari malformation, which has more easily recognizable cranial findings. They include obliteration of the cisterna magna, the lemon sign, ventricular dilatation, and a disproportionately small biparietal diameter.
Posterior fossa abnormalities, including obliteration of the cisterna magna and banana-shaped cerebellum are almost diagnostic of associated open meningomyelocele. Conversely, a normal cisterna magna virtually eliminates the possibility of spina bifida. The “lemon sign,” although quite useful, is not specific for meningomyelocele (12,13). Resolution of the lemon sign in fetuses with meningomyelocele invariably occurs by the 34th week of gestation.
The presence of these characteristic cranial findings serves as a marker for a meningomyelocele. The bony spinal defect should be imaged as should the associated soft-tissue findings (i.e., myelomeningocele sac, disruption of the overlying skin, or both). The level and extent of the defect should be reported.
As with all detected prenatal abnormalities, the remainder of the fetus should be carefully examined for associated abnormalities. The neuromuscular anomalies, in particular, caused by the spinal defect lead to the development of clubfoot. Meningomyelocele also may be associated with an increased risk of karyotype abnormality (14).
Neural tube defects are usually accompanied by abnormally high levels of maternal serum alpha-fetoprotein. The rate of neural tube defects and the risk of recurrence can be decreased by maternal folate supplementation around the time of conception (15).
Aunt Minnie’s Pearls
“Lemon” and “banana” signs imply meningomyelocele.
Neural tube defects are commonly associated with abnormally high levels of maternal serum alpha-fetoprotein.
Case 4.8
HISTORY: A 30-year-old woman had a fetus imaging at 21 weeks’ gestation. Prior sonography was performed in Australia at 8 weeks’ gestation (a routine study was requested as part of initial patient evaluation in the United States)
FINDINGS: Transabdominal sagittal view of the fetal spine does not demonstrate a normal head (Fig. 4.8.1, arrows). Transvaginal coronal view of the face confirms absence of the calvarium and brain cephalad to the orbits (Fig. 4.8.2, arrows).
DIAGNOSIS: Anencephaly
DISCUSSION: Anencephaly, which results from failure of the rostral neuropore to close by the 24th day of fetal life, is the most common type of neural tube defect; it is reported in 1 of 1,000 births (10,11). A distinct female predominance is seen in anencephaly; the female-to-male ratio is 4:1. Elevated alpha-fetoprotein levels can be detected early in pregnancy, and polyhydramnios is seen in up to one-half of cases after 26 weeks’ gestation. Symmetric loss of both brain tissue and calvarium cephalad to the bony orbits is the most reliable feature of this anomaly and is best demonstrated on a coronal image of the fetal face.
Angiomatous stroma may be seen above the fetal orbits (i.e., area cerebrovasculosa); in such cases, it may be difficult to distinguish this disorder from congenital absence of the calvarium (i.e., exencephaly), in which some brain tissue is present above the orbits. Because the bony calvarium cannot be identified with transvaginal sonography before 11.5 weeks’ gestation, anencephaly should not be diagnosed before this time.
Up to one-third of cases of anencephaly may have additional anomalies, most commonly spina bifida. If identified, the spinal dysraphism can help to distinguish anencephaly from exencephaly in difficult cases (16). This distinction is important, because the risk of neural tube defects in future pregnancies is greater in mothers of anencephalic children. Periconceptional folate acid supplementation decreases the risk of anencephaly.
Aunt Minnie’s Pearls
Anencephaly = loss of brain tissue and calvarium in a fetus older than 11.5 weeks’ gestation.
Elevated alpha-fetoprotein levels and polyhydramnios are associated findings in anencephaly.
Up to one-third of anencephalic babies have additional anomalies; the most common is spina bifida.
Case 4.9
HISTORY: A 33-year-old woman with a history of polysubstance abuse at 33 weeks’ gestation underwent cesarean section for persistent vaginal bleeding
FINDINGS: A sagittal image (Fig. 4.9.1, arrow) of the lower uterine segment shows the placenta completely covering the cervical os.
DIAGNOSIS: Complete placenta previa
DISCUSSION: Placenta previa is defined as the implantation of the placenta over the cervical os. There are three recognized variations of placenta previa: complete, partial, and marginal.
In complete placenta previa, the placenta is implanted on both sides of the internal cervical os, bridging the os. This type presents the most serious maternal risk because it is associated with greater blood loss than with marginal or partial previa. The frequency of total placenta previa has been reported as low as 20% and as high as 43%. As a leading cause of third-trimester hemorrhage, patients with placenta previa classically present with painless bleeding. Massive vaginal bleeding can result in fetal and maternal death if vaginal delivery is attempted. Complete placenta previa always requires cesarean section (17). Potential sources of false-positive diagnosis include an overdistended urinary bladder, contraction in the lower uterine segment, and subchorionic hematoma (18).
Significant risk factors are maternal age older than 35 years and African American or other minority race.
Aunt Minnie’s Pearls
In complete placenta previa, the placenta covers the entire cervix.
Placenta previa is a major cause of third-trimester bleeding.
Complete placenta previa always requires cesarean section.
Significant risk factors are maternal age older than 35 years and African American or other minority race.
Case 4.10
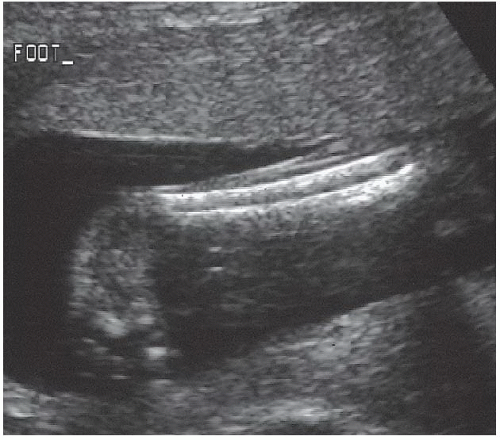
HISTORY: A 27-year-old gravid woman with a history of a second-trimester spontaneous abortion
FINDINGS: A sagittal image reveals that the cervix is dilated to 3 cm, and the classic hourglass, bulging membranes protrude into the vagina (Fig. 4.10.1, arrows). The fetal foot is seen on a transverse image of the cervix (Fig. 4.10.2, arrows).
DIAGNOSIS: Cervical incompetence
DISCUSSION: Cervical incompetence is a functional condition in patients who often present with a history of recurrent, usually painless second-trimester spontaneous abortions. Sonographic findings of a cervix <3 cm long, a gaping internal os, and funneling or tunneling of the patient’s membranes into the endocervical canal can be associated with preterm delivery (19). The shorter the cervix, the more likely the patient will deliver prematurely. Cervical cerclage is the treatment of choice.
The cervix can change, often dramatically, during the sonographic examination. The cervix may appear completely normal at one point in the examination and grossly abnormal at another. For high-risk patients, the cervix should be imaged more than once and observed continuously for several minutes (20).
Aunt Minnie’s Pearls
Hourglass membranes gaping through cervical os = severe cervical incompetence.
In high-risk patients, the cervix should be imaged more than once and continuously for several minutes.
Case 4.11
HISTORY: Repeated bouts of urinary colic
FINDINGS: A longitudinal view of the kidney (Fig. 4.11.1) demonstrates markedly increased echogenicity in the renal pyramids (arrows). The renal cortex is normal in echogenicity, and no hydronephrosis is identified. The kidneys are normally shaped and are otherwise unremarkable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree