Abstract
Atretic cephaloceles, grey matter heterotopia, and septo-optic dysplasia are uncommon congenital cerebral malformations commonly diagnosed in children. The case is a rare one in which atretic parietal cephalocele, grey matter heterotopia, and septo-optic dysplasia are seen concurrently and diagnosed in a 60-year-old man with a history of focal onset seizures. In contrast to their congenital origin, the patient never experienced antecedent neurodevelopmental delay or significant endocrine disturbances. The case requires the consideration of the role of MRI in identifying unsuspected congenital cerebral malformations in adult patients with seizures and performing a complete neurological and ophthalmological examination in these patients.
Introduction
Atretic cephaloceles, their development likely linked to neural tube closure defects typically diagnosed in pediatric patients, are tiny, subcutaneous scalp lesions containing meninges, neural, and glial rests [ ]. Grey matter heterotopia is a disease of neuronal migration, which results in improperly placed clusters of cortical neurons due to disrupted migration from the germinal matrix to the cortex of the cerebrum from the 6th to 16th weeks of gestation [ , ]. Septo-optic dysplasia, which is associated with schizencephaly and hypothalamic-pituitary dysfunction, is characterized by anomalies of the optic nerves and septum pellucidum. Patients usually arrive with visual impairment and seizures; MRI provides a precise diagnosis [ ]. This report presents a rare case of these conditions diagnosed in a 60-year-old male patient presenting with seizures.
Clinical history
A male patient, 60 years old, arrived at the neurology clinic complaining of focal seizures. He was a known seizure disorder patient under medical management but was not previously evaluated for seizures. The medication was irregular, and the patient did not maintain a seizure diary. The patient had a focal seizure with clonic tonic movement of the upper limb with altered consciousness. The patient had no history of prodromal symptoms like light-headedness, insomnia, or changes in behavior. The seizures were not preceded by an aura. However, he complained of postictal confusion, headache, and sore upper arm muscles.
The patient’s birth history was normal. The patient had no history of delayed developmental milestones. The patient had no familial history of seizures or any congenital abnormalities. The patient had a typical build. The patient had no history of trauma or surgical history. As per protocol, the patient was advised to take an electroencephalogram [EEG], MRI, and serum electrolytes was advised. Serum electrolytes were advised. Serum sodium and potassium are within normal limits. Liver and kidney function tests revealed no abnormality. EEG showed a seizure focus along the right fronto-temporal region.
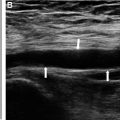
Magnetic resonance imaging [MRI] of the brain was done, which revealed the following imaging findings – A mid-line parietal subcutaneous cystic lesion, with an underlying calvarial defect and cerebrospinal fluid tract, compressed cerebellum with prominent supra cerebellar cistern and raised torcular herophili. The above findings are diagnostic of atretic parietal cephalocele [APE]. Multiple grey matter nodules were noted in sub ependymal region along bilateral lateral ventricles, suggesting grey matter heterotopia [GMH]. Fused and dilated bilateral lateral ventricles and third ventricle with thinning of cerebral parenchyma and corpus callosum are also noted along with absent septum pellucidum; however, the falx is present, the interhemispheric fissure is fully formed, the thalami and frontal lobes are not fused. The optic chiasm is mildly hypoplastic. These features are suggestive of septo-optic dysplasia [SOD] while ruling out lobar holoprosencephaly. The final diagnosis of this case was Septo-optic Dysplasia with Grey Matter Heterotopia and Atretic Parietal Cephalocele ( Figs. 1–4 ).