MR imaging of hip arthroplasty can be technically challenging due to artifacts associated with metallic implant components; however, utilization of specific parameter modifications and advanced metal reduction sequences allows acquisition of high-quality diagnostic images in patients with metallic implants. Given the increasing prevalence of hip arthroplasties within the population, familiarity with appropriate imaging techniques and expected pathology within this patient population is important knowledge for radiologists who encounter patients with hip arthroplasty in clinical practice.
Key points
- •
Total hip arthroplasties are increasing in prevalence; imaging is an important diagnostic tool.
- •
MR imaging around metallic implants is challenging due to artifact.
- •
Modification of routine pulse sequences and addition of advanced sequences can produce accurate diagnostic studies.
Introduction
Hip arthroplasty is an increasingly common procedure, with a recent study projecting a 5.2% annual growth rate for primary total hip arthroplasties (THAs) resulting in a 176% increase in THA by 2040 and a 659% increase by 2060. While high clinical success rates in an aging population contribute to increases in THA, these implants have a finite expected lifespan and are associated with a variety of complications.
Discussion of problem/clinical presentation
Diagnostic imaging is a crucial tool in evaluation of musculoskeletal pathology; however, metal-related artifacts make MR imaging of patients with arthroplasty particularly challenging. Given the clinical importance of accurate diagnosis in patients with arthroplasty, familiarity with current metal imaging techniques and ongoing advances is crucial knowledge for imagers involved in interpretation of arthroplasty imaging to maximize the diagnostic potential of MR imaging in patients with THA.
Imaging techniques
Routine Techniques
While conventional clinical MR imaging sequences tend to suffer from reduced image quality in the presence of metallic implants due to metal-related artifacts, modification of certain acquisition parameters can result in significant mitigation of metal-related artifacts and improvement in image quality. Scanning at high field strength should be avoided, as the degree of susceptibility artifact generated by a particular implant is directly proportional to magnetic field strength; therefore, scanning at 1.5 T is preferable to scanning at 3.0 T. Utilization of fast spin echo sequences limits signal decay due to their multiple refocusing pulses, while use of gradient echo sequences should be avoided. Placing the implant as close to isocenter as possible and aligning the long axis of the implant with the main magnetic field, when possible, also minimized the degree of associated artifact. When utilizing fat-suppressed techniques, spectrally selective fat suppression (eg, fat sat) should be avoided in favor of more robust techniques such as inversion recovery (IR), which is less susceptible to local field inhomogeneities. Reducing the voxel size reduces intra-voxel decay, while increasing the bandwidth reduces image distortion; these 2 modifications result in decreased signal-to-noise ratio, though this may be mitigated by increasing the number of excitations.
Advanced Techniques
Employing the earlier parameter modifications can yield significant improvements in image quality when acquiring conventional MR imaging sequences in the presence of metallic hardware; however, large metallic implants such as THAs, and in particular metal-on-metal arthroplasties, may generate a large amount of artifact in spite of appropriate parameter modifications. Advanced techniques specifically designed for metal artifact reduction are particularly useful in imaging patients with these types of implants.
Two of the most commonly utilized advanced metal reduction sequences are slice encoding metal artifact correction (SEMAC) and multi-acquisition variable resonance image combination (MAVRIC). These are multispectral techniques that achieve metal artifact reduction by exciting, encoding, and summing distinct 3 dimensional imaging volumes, with post-processed composite images demonstrating marked reduction in metal artifact relative to conventional images with parameter modifications. These sequences are continually evolving; for example, recent advances in the MAVRIC sequence allow acquisition of isotropic datasets that can be reformatted in multiple planes; this is achieved via utilization of an initial calibration pulse that allows reduction of the number of required frequency bins, resulting in time savings that can then be used toward the isotropic acquisition.
Protocols
A combination of modified routine clinical sequences plus additional advanced sequences typically provides an optimal combination of metal artifact suppression, tissue contrast, and spatial resolution when imaging patients following hip arthroplasty. At the authors’ institution, a routine THA imaging protocol consists of large field of view (FOV) coronal MAVRIC IR and MAVRIC proton density (PD)-weighted images, large FOV axial PD, and dedicated unilateral small FOV axial and coronal PD images of the affected hip. As the coronal MAVRIC PD images are obtained as an isotropic acquisition, these are reformatted as sagittal and axial images. Additional planes of IR imaging may be added as warranted based on findings visible at the time of the scan.
Imaging findings/pathology
Normal
When interpreting postsurgical imaging, it is crucial to be familiar with the range of expected normal postoperative appearances based on the procedure performed and the postsurgical timeframe, in order to facilitate differentiation of normal appearances versus pathologic. Immediately following THA, postsurgical marrow and soft tissue edema are expected findings, as is postsurgical synovitis. Overtime, these findings tend to resolve, though focal regions of postsurgical signal abnormality, such as marrow hyperintensity related to reaming and scar along incision sites, may persist indefinitely.
Pathology
MR imaging is useful for detecting a variety of complications in patients following THA. While complications such as infection are common to any type of surgical intervention, certain complications are specific to THA, and in particular certain implant designs, such as metal-on-metal bearings and constructs with modular junctions, may be prone to particular complications such as adverse local tissue reaction (ALTR).
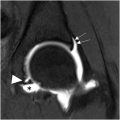
Periprosthetic Fracture
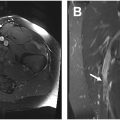
Periprosthetic fractures may occur intraoperatively or at any time during the postoperative time period. Marrow signal hyperintensity on fat-suppressed images should alert the interpreting radiologist to the potential presence of a periprosthetic fracture, though care must be taken to avoid mistaking regions of signal abnormality related to artifact for pathology. Periprosthetic fractures are commonly related to traumatic injury but may also develop in the setting of stress. Periprosthetic stress injury may manifest as stress reaction rather than a frank fracture and may be particularly difficult to differentiate from artifact. Periprosthetic fractures may also be pathologic; regions of osteolysis may weaken the bone and predispose to fracture. , For example, bulky osteolysis within the greater trochanter may sufficiently weaken the bone to the point where minimal insult such as traction related to the hip abductors results in fracture ( Fig. 1 ). This can be difficult to treat due to extensive loss of bone stock preventing normal healing.

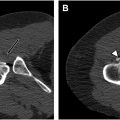
Mechanical Loosening
Component loosening may occur due to mechanical factors or may also occur due to extensive bulky osteolysis. Mechanical loosening on MR imaging manifests as circumferential linear bone resorption along the interfaces of the loose component. This imaging finding corresponds to a fibrous interface between the bone and implant on histopathology and is analogous to the thin rim of linear lucency observed on radiographs in patients with implant loosening ( Fig. 2 ). MR imaging assessment of loosening may be difficult in implants with cemented femoral components if there is delamination along the metal–cement junction, as metal and cement both appear as signal void on MR images, and therefore, unless there is fluid within the failed interface, lack of contrast between the 2 materials may prevent direct visualization of the failed interface. ,

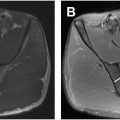
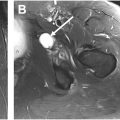
Infection
Prosthetic joint infection is a serious and difficult-to-treat complication following THA. The characteristic appearance of joint infection is a synovitis with hyperintense thickened synovium and a lamellated appearance that is highly specific for the presence of active infection ( Fig. 3 ). Ancillary finding may include sinus tracts, soft tissue fluid collections, lymphadenopathy, and marrow signal suggestive of osteomyelitis. Occasionally, atypical infections may present with synovitis containing rice bodies, though this is rare and somewhat nonspecific ( Fig. 4 ). Oftentimes, clinicians are already aware of the presence of infection but order imaging to determine the extent of infection for treatment planning. In this case, it is particularly important to note any loculated fluid collections separate from the joint that may need to be addressed individually.


Polymeric Wear and Osteolysis
Polymeric wear debris results in a foreign body reaction in which particles are phagocytized and/or encapsulated by macrophages and foreign body giant cells. This reaction also results in osteoclast activation, leading to bone resorption and osteolysis. On MR imaging, polymeric synovitis has a typical appearance, with isointense polymeric debris plus a variable amount of fluid. , , Polymeric osteolysis typically manifests as regions of isointense bone resorption with well-defined sclerotic margins ( Fig. 5 ), though osteolysis may less commonly appear as cystic foci with internal fluid signal. When extensive, osteolysis may result in poor implant integration and ultimately component loosening. Osteolysis may also result in significant loss of bone stock, predisposing to periprosthetic fracture and complicating revision arthroplasty. Though of obvious clinical import, polymeric wear tends to result in fairly indolent pathology and therefore may warrant surveillance rather than immediate revision.