Vascular and Lymphatics
QUESTIONS
A. Tc-99m sulfur colloid
B. Tc-99m DTPA
C. Tc-99m MAA
D. Tc-99m DMSA
View Answer
1 Answer A. In the United States, filtered Tc-99m sulfur colloid (particle size 100 to 200 nm) is most commonly used for sentinel lymph node (SLN) localization by lymphoscintigraphy. Tc-99m nanocolloidal albumin (particle size 5 to 100 nm) is preferred in most of Europe, while Tc-99m antimony trisulfide (particle size 3 to 30 nm) is preferred in Australia and Canada. Tc-99m tilmanocept (Lymphoseek) is an alternative to radiocolloid, which was approved by the FDA in 2013. It targets dextran-mannose receptors on the surface of macrophages.
Reference: Giammarile F, Alazraki N, Aarsvold JN, et al. The EANM and SNMMI practice guideline for lymphoscintigraphy and sentinel node localization in breast cancer. Eur J Nucl Med Mol Imaging 2013;40(12):1932-1947.
2 In order to expedite the migration as well as to optimize the retention within the lymph nodes, Tc-99m sulfur colloid utilized for lymphoscintigraphy is filtered. What is the typical size of these filtered particles?
A. 100 to 220 nm
B. 10 to 22 nm
C. 100 to 220 µm
D. 10 to 22 µm
View Answer
2 Answer A. The sulfur colloid (SC) particles in standard preparations are too large for the purposes of sentinel lymph node (SLN) lymphoscintigraphy. Particles greater than 400 nm in size may not migrate to the regional lymph nodes at all. Particles that are too small may migrate too quickly through the entire nodal basin, making identification of a single sentinel lymph node difficult. Unfiltered Tc-99m SC is comprised of particles ranging from 15 to 5,000 nm with an average size of 305 to 340 nm. For SNL scintigraphy, the SC is usually filtered using a 0.22-µm filter, which results in suspension of colloid particles ranging in size between 100 and 220 nm. This results in a more uniform mixture of smaller particles, which makes it more conducive to lymphatic drainage.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:353-355.
Newman EA, Newman LA. Lymphatic mapping techniques and sentinel lymph node biopsy in breast cancer. Surg Clin North Am 2007;87(2):353-364, viii.
3 Which of the following characteristic constitutes a lymph node as the sentinel lymph node on the lymphoscintigraphy?
A. Lymph node visualized closest to the tumor
B. Largest visualized lymph node
C. Most intense visualized lymph node
D. First visualized lymph node
View Answer
3 Answer D. Sentinel lymph nodes (SLN) are regional nodes that are directly connected to the primary tumor by lymphatic channels. Early dynamic images frequently demonstrate a channel leading to the SLN which is the first lymph node to be visualized in a nodal drainage basin. The major criteria for identifying SLNs are the time of appearance and occasionally visualization of the connecting lymphatic channels. SLN need not be the hottest, the closest, or the largest lymph nodes visualized. As one or more lymph nodes may be connected to the tumor by the lymphatic channels, multiple SLNs may be seen. In such a case, all should be surgically removed and tested for metastatic disease. SLN biopsy is now the gold standard for lymph node staging in breast cancer and melanoma. SLN resection reduces morbidity and has similar mortality rates compared to more invasive lymph node dissections.
Reference: Chakera AH, Hesse B, Burak Z, et al. EANM-EORTC general recommendations for sentinel node diagnostics in melanoma. Eur J Nucl Med Mol Imaging 2009;36(10):1713-1742.
4 Which of the following injection sites would be expected to have the most likelihood of internal mammary lymph node visualization?
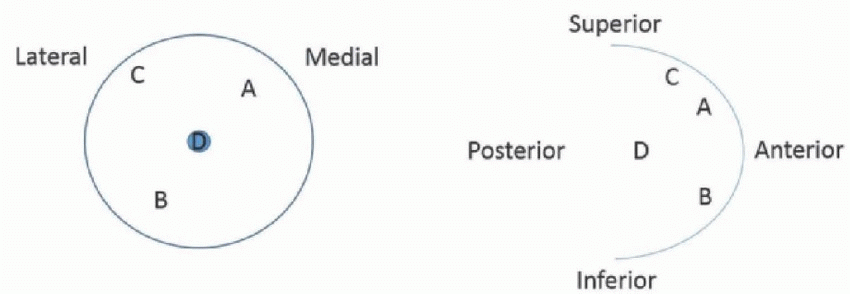 |
View Answer
4 Answer D. While one would surmise that the ideal injection site to visualize internal mammary nodes would be superficial skin injection medial to the midclavicular line (A), it has been shown that internal mammary node identification is better with deep peritumoral injections. A recent anatomical study on breast lymphatics found that separate lymphatic networks exist in the ventral and dorsal parts of the breast with the formal draining to the axilla and latter to the internal mammary chain. Important advantages of the deep injections include improved detection of the extra axillary sentinel lymph nodes and the possibility of using larger injection volumes. A major advantage of superficial injections (subdermal, periareolar, intradermal, or subareolar) is that there are easy to perform; however, they are often more painful than the peritumoral injections. Combination of both techniques may improve the sentinel lymph node detection and decrease false-negative findings.
References: Hindie E, Groheux D, Espie M, et al. [Sentinel node biopsy in breast cancer]. Bulletin du Cancer 2009;96(6):713-725.
Shimazu K, Tamaki Y, Taguchi T, et al. Lymphoscintigraphic visualization of internal mammary nodes with subtumoral injection of radiocolloid in patients with breast cancer. Ann Surg 2003;237(3):390-398.
Suami H, Pan WR, Mann GB, et al. The lymphatic anatomy of the breast and its implications for sentinel lymph node biopsy: a human cadaver study. Ann Surg Oncol 2008;15(3):863-871.
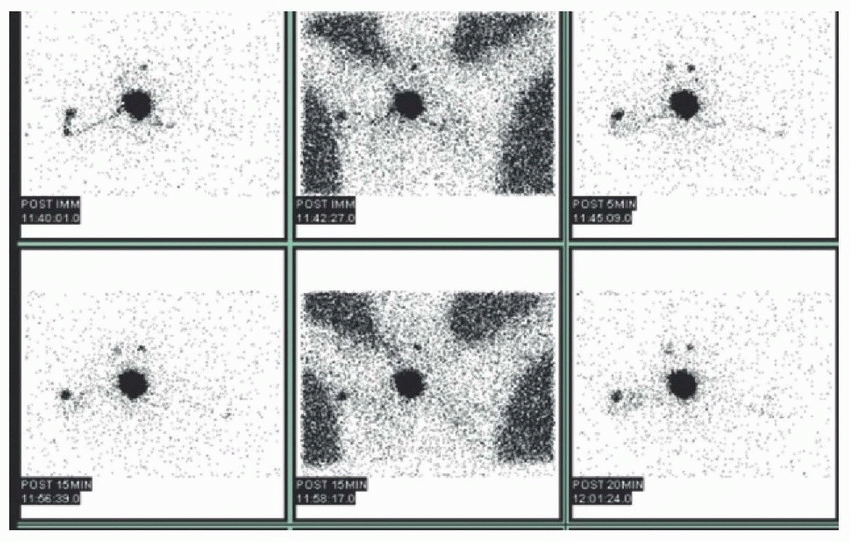
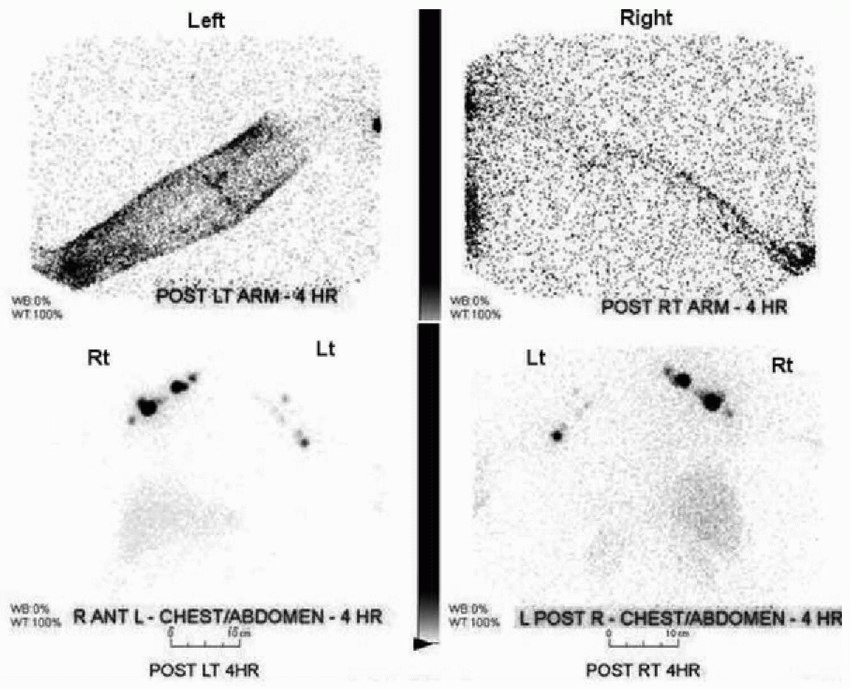
5 The following images are from a bilateral upper extremity lymphangiogram. What is the most likely side and level of the lymphatic obstruction?
 |
A. Right forearm
B. Left forearm
C. Right upper arm
D. Left upper arm
E. No evidence of obstruction
View Answer
5 Answer D. The patient was injected between the webs of the fingers in order to visualize the lymphatic drainage. The supplied images demonstrate subcutaneous activity tracking along the left upper extremity, which stops at the midupper arm. In contrast, normal lymphatic drainage via lymphatic channels is visualized on the right. Lymph node visualization is present but decreased within the left axilla when compared to the right. The combination of these findings suggest partial left-sided lymphatic obstruction. With complete obstruction, the left axillary lymph nodes would not be visualized at all, and superficial activity would be seen throughout the left arm. Typical indications for lymphatic drainage evaluation by lymphoscintigraphy include lymphedema, chyluria, chylothorax, and chyloperitoneum. The most common secondary causes of abnormal lymphatic drainage are prior surgery, cancer, infection, and radiation.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:345-360.
Moshiri M, Katz DS, Boris M, et al. Using lymphoscintigraphy to evaluate suspected lymphedema of the extremities. Am J Roentgenol 2002;178(2):405-412.
Yuan Z, Chen L, Luo Q, et al. The role of radionuclide lymphoscintigraphy in extremity lymphedema. Ann Nucl Med 2006;20(5):341-344.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: The requisites, 4th ed. Philadelphia, PA: Saunders, 2014:265-287.
6 Which of the following is correct regarding the lymphoscintigraphy of the breast?
A. Injection should take place 24 to 48 hours prior to the planned lymph node dissection.
B. Ultrasound guidance is recommended for superficial breast lesions.
C. Lymph nodes visualized in the first 60 minutes of imaging are considered sentinel lymph nodes.
D. Periareolar injection is recommended for lesions in the upper outer quadrant.
View Answer
6 Answer D. In some centers, all patients get periareolar injections; however, periareolar injection are specifically recommended for lesions located within the upper outer quadrant near the area of the axilla. Injection in the periareolar area in these patients helps differentiate the sentinel lymph node (SLN) from activity in the primary lesion if the injection was around the primary lesion close to the axilla. Injections should take place no more than 18 hours prior to planned SLN resection as intraoperative gamma detection is used to confirm the presence of radioactivity within the lymph nodes. While ultrasound guidance is recommended for deep lesions of the breast, subdermal and intradermal injections without guidance are usually sufficient for more superficial lesions. The first lymph nodes detected within a nodal drainage basin on imaging are considered to be the sentinel lymph node(s). While other lymph nodes may also be marked for potential resection, care should be taken to clearly document the SLN. Lymphoscintigraphy detects the SLN in 90% to 98% of cases.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:344-360.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:265-287.
A. Cobalt-57 sheet source
B. Cadmium-zinc-telluride detector
C. Flat panel x-ray detector
D. Tungsten x-ray tube
View Answer
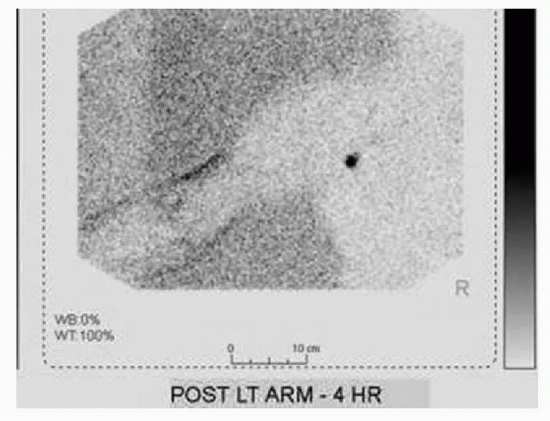
7 Answer A. This is a transmission image acquired using a cobalt-57 sheet source to help provide better anatomical localization. The sheet source is placed behind the patient. The radiation from the sheet gets attenuated by the soft tissues and does not reach the detector. The remaining radiation reaches the detector creating an outline of the patient’s body. Sheet sources are a simple and cheap method to enhance localization of lesions without contributing significant radiation dose to the patient. An x-ray tube can be used when acquiring SPECT/CT images but not in the transmission image that is shown.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:345-360.
Moshiri M, Katz DS, Boris M, et al. Using lymphoscintigraphy to evaluate suspected lymphedema of the extremities. Am J Roentgenol 2002;178(2):405-412.
Yuan Z, Chen L, Luo Q, et al. The role of radionuclide lymphoscintigraphy in extremity lymphedema. Ann Nucl Med 2006;20(5):341-344.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: The requisites, 4th ed. Philadelphia, PA: Saunders, 2014:265-287.
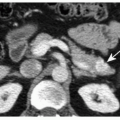
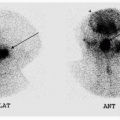
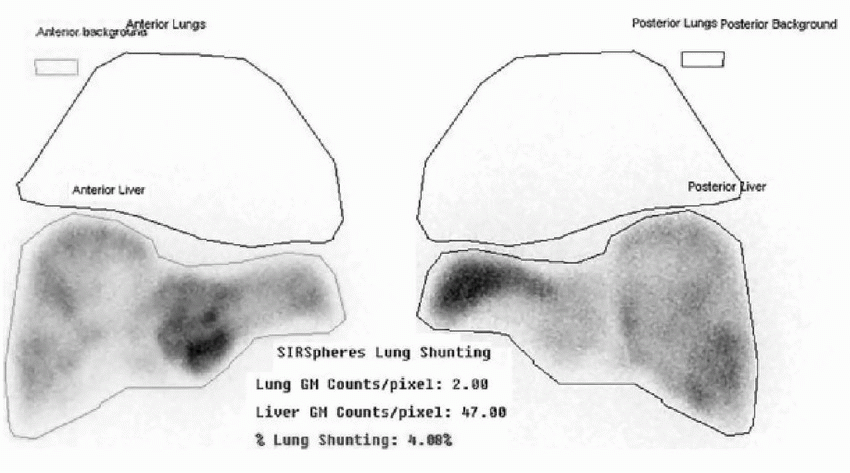
8 The following images were acquired after the intrahepatic injection of Tc-99m MAA. Which of the following would be the best recommendation regarding the planned Yttrium-90 SIR-Spheres treatment?
 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree