Vertebral augmentation consists of minimally invasive techniques indicated in the treatment of vertebral compression fractures (VCFs). These compression fractures cause vertebral body height loss and consequent significant pain and are most frequently the result of osteoporosis, cancer metastasis, or trauma. The deleterious effects of VCFs often compound, as greater load-bearing stress is transferred to the remaining healthy vertebrae. Kyphoplasty, vertebroplasty, and intravertebral implants are closely related vertebral augmentation techniques that serve to relieve pain and to counter pathophysiological stress and structural degradation of the vertebral column alignment. All 3 approaches are performed percutaneously and are therefore attractive options for patients deemed to be poor candidates for open surgery.
Each technique involves transpedicular needle access to the vertebral body matrix, followed by introduction of a cement-like polymer through a catheter to fill the space and provide structural fortification. Vertebroplasty involves injection of the cement material into the matrix space without any adjunctive measures. In kyphoplasty, a balloon is first introduced to expand the collapsed, fractured area with the goal of approximating the prefracture anatomy of the vertebral body and thereby spinal curvature, promptly followed by cement introduction. In intravertebral implantation procedures, a permanent jack is inserted into the vertebral body matrix and expanded craniocaudally, with the same purpose of restoring normal structure, before the matrix space is filled with cement polymer. This article provides an overview of these vertebral augmentation techniques, including pre and postprocedural considerations, with an emphasis on the technical aspects of the interventions.
Preprocedure
Vertebral augmentation procedures are indicated for symptomatic treatment of acute or acute-on-chronic pain related to vertebral compression fracture (VCF). Existing data shows that patients with chronic back pain related to VCF do not achieve sufficient pain resolution to justify intervention Upon physical examination of patients with acute lower back pain, tenderness over the affected vertebral level is classically seen, with diagnosis able to be confirmed via imaging. While radiographs can be used for screening, cross-sectional imaging with CT or MRI are frequently employed to better assess degree, chronicity, and underlying predisposing osteopathy of the VCF. In specific, fluid sensitive MRI and contrast enhanced CT or MRI sequences can be useful in providing an imaging correlate to potential levels of clinical pain and symptoms. Patients can be refractory to conservative treatment including pharmacologic analgesia, bracing, and immobilized bedrest. While more conservative methods are often seen as safer, these options carry well-described, harmful effects. Prolonged bedrest can lead to decreased bone density, decreased muscle mass, and development of pressure sores in elderly patients with VCFs. Recovery from acute VCF with nonprocedural options is of course possible, with pain decreasing as the VCF progresses to the sclerotic, chronic phase. However, for patients that are not sufficiently responsive to conservative treatment or who would prefer procedural intervention as a first choice, vertebral augmentation presents a safe and effective treatment. Patients who receive vertebral augmentation are typically first assessed by orthopedic or neurosurgeons and deemed to be unsuitable candidates for open surgery.
Vertebral augmentation interventions are most commonly performed on thoracolumbar and sacral vertebrae, with unique considerations at each level. Thoracic pedicles are wider than those in the lumbar region, necessitating a more oblique entry angle. Intervention at the thoracic level also carries risk of injury to the pleura as well as theoretical risks of the great vessels. The sacrum has an even wider angle of entry, but intervention remains safe and effective. Cervical augmentation is technically possible, but is seldom performed due to smaller anatomical space and the heightened risk of serious complications such as cord or nerve root damage or vascular laceration. There is no theoretical minimum or maximum number of vertebrae that can be intervened upon, given that intervention is justified by clinical symptoms, especially pain and correlative imaging.
Prior to intervention, patients should pause taking blood thinners for 2 days and aspirin for 5 days if they are able to do so per SIR guidelines and INR should be >2 to mitigate risk of bleeding The hemoglobin should ideally be >7 mg/dL. Due to the rich vascularity of the vertebral body, presence of coagulopathies amplifies inherently increased risk Heightened care should be taken pre and postprocedurally to ensure patients with coagulation and bleeding disorders remain hemodynamically stable.
Contraindications to vertebral augmentation include active infectious process and lack of symptoms such as pain caused by VCF. Given the rich vascularity of vertebrae, active and hematologic infections can be spread via intervention, opening the door for severe complications including osteomyelitis and septicemia. Infection is especially contraindicated for intravertebral implant placement, as the implant carries greater risk of colonization by bacteria. Bony retropulsion is a relative contraindication, involving posterior displacement of fractured bone into the spinal canal which can potentially cause spinal cord injury. Augmentation may not resolve neural injury and in fact may exacerbate symptoms. However, if pain related to bony retropulsion is occurring without neurological deficits, it may be appropriate to intervene as certain interventions such as vertebral body implantation can reduce some or all of the retropulsion. In general, if a patient is experiencing neurological symptoms prior to intervention, the case should be handled primarily or jointly by neurosurgery. As the goal of vertebral augmentation is resolution of pain, VCF without pain should not be intervened upon as the risks would outweigh the benefits.
Procedure
The patient is placed in the prone position and is draped according to the location of the target site. Betadine is used to clean the area, as chlorhexidine is alcohol-based and poses a greater risk of complication if it were to be introduced into the spinal canal. Chlorhexidine is toxic to nerve cells, and may cause meningitis, paralysis, paresthesia, and/or systemic toxicity. Due to the rich vascularity of the vertebral region, 2 grams of cefazolin is intravenously administered prophylactically. While the number needed to treat is high, the few patients who do become infected experience severe and costly complications. This occurs alongside sedation or anesthesia that typically ranges from mild to moderate sedation to general anesthesia if preferred by the patient.
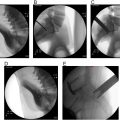
Vertebral access can be obtained via a bipedicular or unipedicular approach. Vertebroplasty and kyphoplasty are typically performed via unipedicular access when feasible. This can be done with either a curved or straight guiding cannula, with the only difference being the angle of insertion through the pedicle. Insertion of a curved cannula requires rotation towards the center of the vertebral body as the cannula is advanced under fluoroscopic guidance. Insertion of a straight cannula requires a more oblique approach angle through the pedicle so that its tip reaches the center of the vertebral body matrix ( Figs. 1 and 2 ). Conversely, intravertebral implant procedures are usually done via bipedicular access, meaning that cannulas are inserted bilaterally, parallel to each other through the pedicles ( Figs. 1 and 2 ). AP and oblique “scotty dog” views are used to visualize the vertebrae and accentuate the posterior elements. Anesthetic is given using a 3.5 Fr needle, inserted down to the level of the periosteum. Skin incision is then performed, and an 11 Fr guiding cannula is advanced to the level of the pedicle. Alignment must be visualized in the scotty dog view prior to engaging the needle into the cortex of the pedicle by malleating, then return should be made to true AP and lateral squared-up views ( Figs. 3 and 4 ). In the AP view, the spinous process should be midline and the end plates should be aligned linearly with each other. The pedicles should be visible just below the superior end plate. In the lateral view, the transverse processes should be aligned and the AP contours should appear as defined, nonoblique lines. After verification that the needle is not at risk of medial entry to the spinal canal or lateral exit through the cortex, continue malleating under intermittent or real-time fluoroscopy. The cannula should pass into the posterior vertebral body wall with great care to ensure no deviation, especially medially into the spinal canal.