Chapter TWO
Breast Imaging
MARY SCOTT SOO  CHAPTER EDITOR
CHAPTER EDITOR
MARGARET E.
WILLIFORD
AND
MARY SCOTT SOO
HISTORY
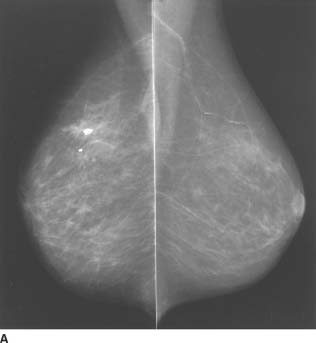
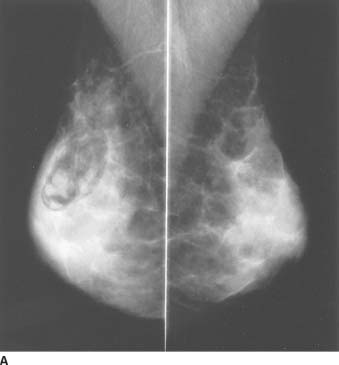
Screening mammogram in a 44-year-old woman.
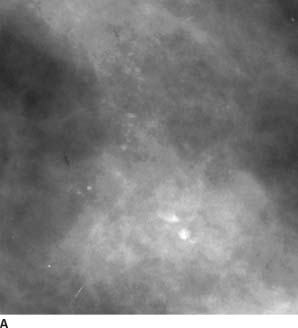
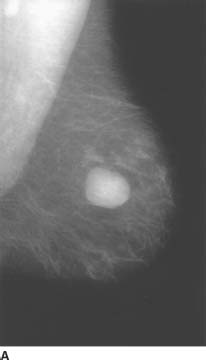
 FIGURE 2-1A Photographically enlarged, magnified craniocaudal mammogram of the right breast demonstrates heterogeneously dense fibroglandular tissue. Multiple vague, round, and indistinct calcifications are present. No calcifications were identified in other regions of the breast.
FIGURE 2-1A Photographically enlarged, magnified craniocaudal mammogram of the right breast demonstrates heterogeneously dense fibroglandular tissue. Multiple vague, round, and indistinct calcifications are present. No calcifications were identified in other regions of the breast.
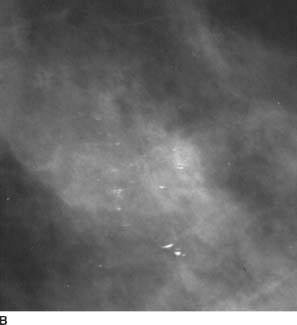
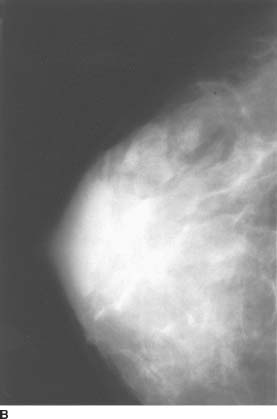
 FIGURE 2-1B Photographically enlarged, magnified true lateral mammogram of the right breast in the same region seen in Figure 2-1A. The calcifications are denser and assume a teacup or meniscus appearance as they layer ependently.
FIGURE 2-1B Photographically enlarged, magnified true lateral mammogram of the right breast in the same region seen in Figure 2-1A. The calcifications are denser and assume a teacup or meniscus appearance as they layer ependently.
 Milk of calcium: This is the best diagnosis because milk of calcium has different appearances depending on the mammographic projection obtained. The calcifications are often smudge-like or indistinct on the craniocaudal views but have a teacup or meniscus appearance on horizontal beam, 90-degree lateral radiographs.
Milk of calcium: This is the best diagnosis because milk of calcium has different appearances depending on the mammographic projection obtained. The calcifications are often smudge-like or indistinct on the craniocaudal views but have a teacup or meniscus appearance on horizontal beam, 90-degree lateral radiographs.
 Fat necrosis: The calcifications associated with fat necrosis often vary in density and shape and can be indistinguishable from carcinoma. Many of the calcifications evolve over time to a more coarse configuration, or may have an eggshell appearance, as seen in oil cysts. However, the appearance of fat necrosis does not usually vary on the different projections, making this an unlikely diagnosis in this case.
Fat necrosis: The calcifications associated with fat necrosis often vary in density and shape and can be indistinguishable from carcinoma. Many of the calcifications evolve over time to a more coarse configuration, or may have an eggshell appearance, as seen in oil cysts. However, the appearance of fat necrosis does not usually vary on the different projections, making this an unlikely diagnosis in this case.
 Carcinoma: Calcifications associated with carcinoma are often pleomorphic, varying in shape and density. However, the appearance of calcifications associated with carcinoma does not change on the different mammographic projections, making carcinoma a poor choice in this case.
Carcinoma: Calcifications associated with carcinoma are often pleomorphic, varying in shape and density. However, the appearance of calcifications associated with carcinoma does not change on the different mammographic projections, making carcinoma a poor choice in this case.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 2, benign. Recommend annual screening mammography.
DIAGNOSIS
Milk of calcium
KEY FACTS
Clinical
 Milk of calcium represents calcified debris that is sedi-mented in the dependent portions of microcysts or cystically dilated acini of cystic lobular hyperplasia.
Milk of calcium represents calcified debris that is sedi-mented in the dependent portions of microcysts or cystically dilated acini of cystic lobular hyperplasia.
 Benign milk of calcium calcifications are seen in 4% to 6% of women undergoing mammography.
Benign milk of calcium calcifications are seen in 4% to 6% of women undergoing mammography.
 Milk of calcium is usually seen in multiple areas of the breast and is usually bilateral. It can be a diagnostic problem when it appears as a unilateral focus. It is important to recognize milk of calcium so that an inappropriate biopsy is not recommended.
Milk of calcium is usually seen in multiple areas of the breast and is usually bilateral. It can be a diagnostic problem when it appears as a unilateral focus. It is important to recognize milk of calcium so that an inappropriate biopsy is not recommended.
 Milk of calcium calcifications are benign and do not require a biopsy, but carcinomas can occur adjacent to such microcystic calcifications. Therefore, each group of calcifications must be inspected carefully.
Milk of calcium calcifications are benign and do not require a biopsy, but carcinomas can occur adjacent to such microcystic calcifications. Therefore, each group of calcifications must be inspected carefully.
Radiologic
 The shape of milk of calcium calcifications has been described as meniscus, crescent, teacup, or semilunar. The meniscus or crescent shape is best seen on an erect 90-degree lateral projection since the x-ray beam is horizontal and therefore tangential to the fluid calcium interface in the microcyst.
The shape of milk of calcium calcifications has been described as meniscus, crescent, teacup, or semilunar. The meniscus or crescent shape is best seen on an erect 90-degree lateral projection since the x-ray beam is horizontal and therefore tangential to the fluid calcium interface in the microcyst.
 On the 90-degree lateral view, the linear, curvilinear, or meniscus-shaped calcifications will be oriented parallel to one another along the horizontal axis. The upper border of the calcification may be less distinct than the lower border where the sedimented calcified debris is sharply bounded by the wall of the microcyst.
On the 90-degree lateral view, the linear, curvilinear, or meniscus-shaped calcifications will be oriented parallel to one another along the horizontal axis. The upper border of the calcification may be less distinct than the lower border where the sedimented calcified debris is sharply bounded by the wall of the microcyst.
 The characteristic meniscus or crescent shape is not as well seen on the 45-degree mediolateral oblique view.
The characteristic meniscus or crescent shape is not as well seen on the 45-degree mediolateral oblique view.
 On the craniocaudal projection, the calcifications are seen en face since the x-ray beam is vertical and therefore perpendicular to the fluid calcium interface in the microcyst.
On the craniocaudal projection, the calcifications are seen en face since the x-ray beam is vertical and therefore perpendicular to the fluid calcium interface in the microcyst.
 On the craniocaudal projection, the calcifications are round or ovoid smudges. They can be so faint that they are invisible.
On the craniocaudal projection, the calcifications are round or ovoid smudges. They can be so faint that they are invisible.
 The dramatic difference in the appearance of the calcifications on the craniocaudal, mediolateral, and 90-degree lateral projections is a characteristic feature of benign milk of calcium.
The dramatic difference in the appearance of the calcifications on the craniocaudal, mediolateral, and 90-degree lateral projections is a characteristic feature of benign milk of calcium.
 When milk of calcium calcifications are suspected, magnification views in the 90-degree lateral projection and craniocaudal projection should be performed.
When milk of calcium calcifications are suspected, magnification views in the 90-degree lateral projection and craniocaudal projection should be performed.
SUGGESTED READING
Hamer MJ, Cooper AG, Pile-Spellman ER. Milk of calcium in breast microcysts: manifestation as a solitary focal disease. Am J Roentgenol 1988;150:789.
Linden SS, Sickles EA. Sedimented calcium in benign breast cysts. Am J Roentgenol 1989;152:957.
Moy L, Slanetz PJ, Yeh ED, et al. The pendent view: an additional projection to confirm the diagnosis of milk of calcium. Am J Roentgenol 2001;177:173–175.
Sickles EA, Abele JS. Milk of calcium within tiny benign breast cysts. Radiology 1981;141:655.
D’Orsi CJ, Mendelson EB, Ikeda DM, et al. Breast Imaging Reporting and Data System: ACR BI-RADS – Breast Imaging Atlas. Reston, VA: American College of Radiology, 2003.
RUTH WALSH
AND
MARY SCOTT SOO
HISTORY
A 45-year-old asymptomatic woman presenting for a screening mammogram. A breast ultrasound was subsequently performed.
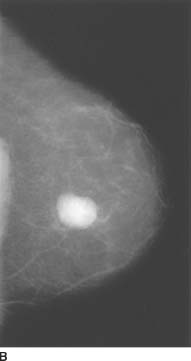
FIGURES 2-2A and 2-2B Craniocaudal (A) and mediolateral oblique (B) mammograms of both breasts show heterogeneously dense fibroglandular tissue. Multiple, bilateral, and predominantly well-circumscribed oval and round masses are present.
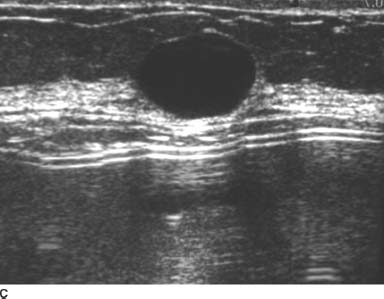
 FIGURE 2-2C Longitudinal sonographic image of the medial left breast, 10:00 position. Sonography of one of the masses shows an anechoic, well-circumscribed oval mass with posterior acoustic enhancement. This appearance was typical of the remainder of the masses.
FIGURE 2-2C Longitudinal sonographic image of the medial left breast, 10:00 position. Sonography of one of the masses shows an anechoic, well-circumscribed oval mass with posterior acoustic enhancement. This appearance was typical of the remainder of the masses.
 Cysts: As seen in this case, cysts are anechoic, well-circumscribed masses that have posterior acoustic enhancement. Cysts are the most commonly encountered breast masses, which cannot be differentiated from other circumscribed masses at mammography unless they contain milk of calcium. Sonography can be used to differentiate cysts from solid breast masses accurately.
Cysts: As seen in this case, cysts are anechoic, well-circumscribed masses that have posterior acoustic enhancement. Cysts are the most commonly encountered breast masses, which cannot be differentiated from other circumscribed masses at mammography unless they contain milk of calcium. Sonography can be used to differentiate cysts from solid breast masses accurately.
 Fibroadenomas: Fibroadenomas can be multiple or bilateral in 15% of cases and are the most common palpable breast masses in adolescents and young women. Although noncalcified fibroadenomas cannot be differentiated at mammography from other circumscribed masses, fibroadenomas appear solid at sonography, unlike the lesions in this case. Large, coarse, popcornlike calcifications are pathognomonic mammographic findings of degenerating fibroadenomas.
Fibroadenomas: Fibroadenomas can be multiple or bilateral in 15% of cases and are the most common palpable breast masses in adolescents and young women. Although noncalcified fibroadenomas cannot be differentiated at mammography from other circumscribed masses, fibroadenomas appear solid at sonography, unlike the lesions in this case. Large, coarse, popcornlike calcifications are pathognomonic mammographic findings of degenerating fibroadenomas.
 Metastases: The sonographic appearance of metastases is that of a solid mass, differing from the lesions seen in this case. Metastatic disease to the breast from an extramammary primary malignancy is rare (0.5% to 1.3% of breast malignancies) and most often has the mammographic appearance of single or multiple circumscribed masses. A clinical history of extramammary malignancy should be present to suspect this diagnosis.
Metastases: The sonographic appearance of metastases is that of a solid mass, differing from the lesions seen in this case. Metastatic disease to the breast from an extramammary primary malignancy is rare (0.5% to 1.3% of breast malignancies) and most often has the mammographic appearance of single or multiple circumscribed masses. A clinical history of extramammary malignancy should be present to suspect this diagnosis.
 Papillomas: Papillomas are less common masses seen at mammography. They are usually <1 cm in size and are typically located in the subareolar region. At sonog-raphy, papillomas are often solid, lobulated masses, making this diagnosis unlikely in the case illustrated. A papilloma can also present as a complex mass at sonography (intracystic or intraductal papilloma), for which biopsy is indicated to exclude a malignant lesion.
Papillomas: Papillomas are less common masses seen at mammography. They are usually <1 cm in size and are typically located in the subareolar region. At sonog-raphy, papillomas are often solid, lobulated masses, making this diagnosis unlikely in the case illustrated. A papilloma can also present as a complex mass at sonography (intracystic or intraductal papilloma), for which biopsy is indicated to exclude a malignant lesion.
 Lymph nodes: Intramammary lymph nodes are typically <1 cm in size, often demonstrate a fatty hilus at mammography, and are usually located in the upper outer quadrants of the breasts. At sonography, lymph nodes are usually hypoechoic with an echogenic fatty hilus. All these features make this an unlikely diagnosis in this case.
Lymph nodes: Intramammary lymph nodes are typically <1 cm in size, often demonstrate a fatty hilus at mammography, and are usually located in the upper outer quadrants of the breasts. At sonography, lymph nodes are usually hypoechoic with an echogenic fatty hilus. All these features make this an unlikely diagnosis in this case.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 2, benign. Recommend annual screening mammography.
DIAGNOSIS
Bilateral simple cysts confirmed by ultrasound
KEY FACTS
Clinical
 Cysts can be seen in all age groups but are more common in women 30 to 50 years of age.
Cysts can be seen in all age groups but are more common in women 30 to 50 years of age.
 Cysts arise in the terminal duct lobular units. They can be grossly visible at mammography or seen only microscopically.
Cysts arise in the terminal duct lobular units. They can be grossly visible at mammography or seen only microscopically.
 Autopsy studies report grossly visible cysts in 20% to 50% of women.
Autopsy studies report grossly visible cysts in 20% to 50% of women.
 Cysts cannot be differentiated reliably from solid palpable masses on physical examination. Therefore, sonog-raphy or needle aspiration is necessary to confirm the diagnosis.
Cysts cannot be differentiated reliably from solid palpable masses on physical examination. Therefore, sonog-raphy or needle aspiration is necessary to confirm the diagnosis.
Radiologic
 Cysts are typically round, oval, or lobular in shape and often multiple and bilateral.
Cysts are typically round, oval, or lobular in shape and often multiple and bilateral.
 Cyst margins are usually well-defined on mammography if not obscured by adjacent fibroglandular tissue. Occasionally, the margins can be indistinct.
Cyst margins are usually well-defined on mammography if not obscured by adjacent fibroglandular tissue. Occasionally, the margins can be indistinct.
 Because cysts cannot be differentiated from other circumscribed masses at mammography, sonography is performed to establish the diagnosis.
Because cysts cannot be differentiated from other circumscribed masses at mammography, sonography is performed to establish the diagnosis.
 Strict sonographic criteria for a simple cyst include anechoic round or oval appearance, smooth, well-circumscribed margins, and posterior acoustic enhancement.
Strict sonographic criteria for a simple cyst include anechoic round or oval appearance, smooth, well-circumscribed margins, and posterior acoustic enhancement.
 When multiple, bilateral, round or oval well-circumscribed masses are present on a baseline screening mammogram, sonography can be performed to determine if the masses are cystic or solid. A 12-month follow-up mammogram is usually recommended for these cystic or solid masses if there are no suspicious features, dominant mass, or history of an extramammary malignancy.
When multiple, bilateral, round or oval well-circumscribed masses are present on a baseline screening mammogram, sonography can be performed to determine if the masses are cystic or solid. A 12-month follow-up mammogram is usually recommended for these cystic or solid masses if there are no suspicious features, dominant mass, or history of an extramammary malignancy.
SUGGESTED READING
Adler DD. Mammographic evaluation of masses. In DB Kopans (ed). Syllabus: A Categorical Course in Breast Imaging. Oak Brook, IL: RSNA,1995:107-116.
Bohman LG, Bassett LW, Gold RH, Volt R. Breast metastases from extramammary malignancies. Radiology 1982;144:309-312.
Jackson VP. Circumscribed microlobulated noncalcified mass. In BA Siegel (ed). Breast Disease Test and Syllabus (2nd Series). Reston, VA: American College of Radiology, 1993:89-99.
Kopans DB (ed). Breast Imaging. Philadelphia, PA: Lippincott, 1989.
Soo MS, Ghate SV, Baker JA, et al. Streaming detection for evaluation of indeterminate sonographic breast masses: a pilot study. Am J Roentgenol 2006;186:1335-1341.
Weinstein SP, Conant EF, Sehgal C. Technical advances in breast ultrasound imaging. Semin Ultrasound CT MR 2006;27:273-283.
RUTH WALSH
AND
MARY SCOTT SOO
HISTORY
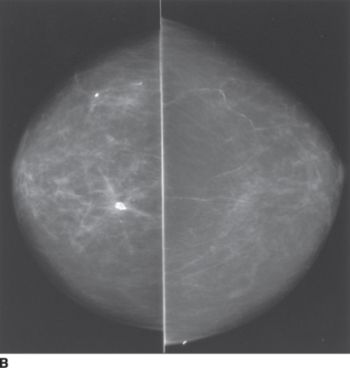
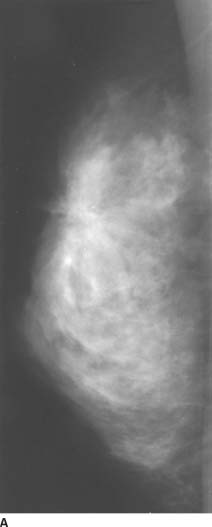
A 43-year-old woman with a palpable lump in the upper outer quadrant of the right breast presents for diagnostic mammography. There is no past surgical history.
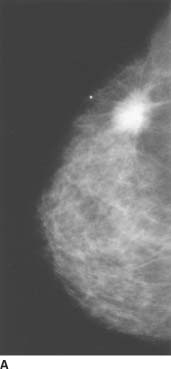
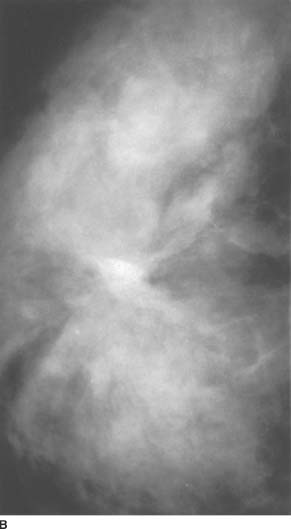
 FIGURES 2-3A and 2-3B Exaggerated lateral craniocaudal view of the right breast with cutaneous BB marking the palpable lump (A), and mediolateral oblique view of the right breast (B) show heterogeneously dense fibroglandular tissue. A 3-cm irregular mass with spiculated margins is present in the upper outer quadrant of the right breast. Several faint punctate microcalcifications are present within the mass. A rounded, dense 1.5-cm lymph node is present in the right axilla.
FIGURES 2-3A and 2-3B Exaggerated lateral craniocaudal view of the right breast with cutaneous BB marking the palpable lump (A), and mediolateral oblique view of the right breast (B) show heterogeneously dense fibroglandular tissue. A 3-cm irregular mass with spiculated margins is present in the upper outer quadrant of the right breast. Several faint punctate microcalcifications are present within the mass. A rounded, dense 1.5-cm lymph node is present in the right axilla.
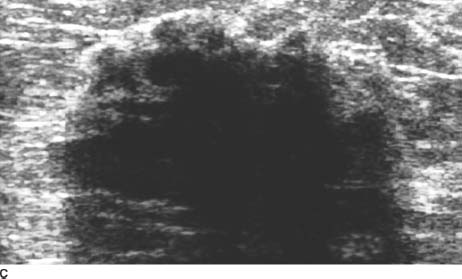
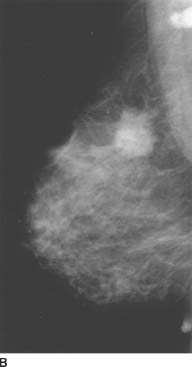
 FIGURE 2-3C Ultrasound of the right breast mass demonstrates an irregular, hypoechoic, microlobulated mass with posterior acoustic shadowing.
FIGURE 2-3C Ultrasound of the right breast mass demonstrates an irregular, hypoechoic, microlobulated mass with posterior acoustic shadowing.
 Carcinoma: A mass with spiculated margins is almost pathognomonic of malignancy. The abnormal axillary lymph node is suggestive of metastatic disease. These features make carcinoma the most likely diagnosis. Although a few rare benign processes can present as spiculated lesions, biopsy is indicated to exclude malignancy.
Carcinoma: A mass with spiculated margins is almost pathognomonic of malignancy. The abnormal axillary lymph node is suggestive of metastatic disease. These features make carcinoma the most likely diagnosis. Although a few rare benign processes can present as spiculated lesions, biopsy is indicated to exclude malignancy.
 Posttraumatic scarring and fat necrosis: There is no history of prior trauma or breast surgery, making this diagnosis unlikely. A postoperative scar can appear as an area of architectural distortion or a spiculated mass that should either decrease in size and density or remain stable over time. Any increase in size should prompt biopsy. To confirm the diagnosis of a surgical scar, the site of the spiculated lesion must match the location of the patient’s cutaneous scar and the location of the biopsied lesion on preoperative or needle localization mammograms.
Posttraumatic scarring and fat necrosis: There is no history of prior trauma or breast surgery, making this diagnosis unlikely. A postoperative scar can appear as an area of architectural distortion or a spiculated mass that should either decrease in size and density or remain stable over time. Any increase in size should prompt biopsy. To confirm the diagnosis of a surgical scar, the site of the spiculated lesion must match the location of the patient’s cutaneous scar and the location of the biopsied lesion on preoperative or needle localization mammograms.
 Radial scar/complex sclerosing lesion: Radial scars are regions of architectural distortion that typically have long, thin spicules radiating outward from a radiolucent center. However, occasionally they can appear dense centrally and contain microcalcifications. The large central mass in this case makes the diagnosis of radial scar unlikely. The term radial scar is used when the lesion measures <1 cm and complex sclerosing lesion is used when the lesion measures >1 cm. These benign proliferative lesions of unknown etiology are usually nonpalpable and cannot be differentiated reliably from carcinoma without biopsy.
Radial scar/complex sclerosing lesion: Radial scars are regions of architectural distortion that typically have long, thin spicules radiating outward from a radiolucent center. However, occasionally they can appear dense centrally and contain microcalcifications. The large central mass in this case makes the diagnosis of radial scar unlikely. The term radial scar is used when the lesion measures <1 cm and complex sclerosing lesion is used when the lesion measures >1 cm. These benign proliferative lesions of unknown etiology are usually nonpalpable and cannot be differentiated reliably from carcinoma without biopsy.
 Abscess: Because there is no history of pain, swelling, or erythema, this is an unlikely diagnosis. Abscesses tend to occur in the subareolar region and often are associated with mammographic changes of mastitis, such as diffuse skin thickening and increased trabecular density.
Abscess: Because there is no history of pain, swelling, or erythema, this is an unlikely diagnosis. Abscesses tend to occur in the subareolar region and often are associated with mammographic changes of mastitis, such as diffuse skin thickening and increased trabecular density.
 Granular cell tumor: These benign tumors have a spic-ulated appearance at mammography but are very rare, making this diagnosis less likely. Biopsy is indicated to differentiate these lesions from carcinoma.
Granular cell tumor: These benign tumors have a spic-ulated appearance at mammography but are very rare, making this diagnosis less likely. Biopsy is indicated to differentiate these lesions from carcinoma.
 Extraabdominal desmoid tumor: These are locally invasive tumors that do not metastasize. Their mam-mographic appearance mimics that of an invasive breast cancer, requiring biopsy for diagnosis. These, too, are rare, making the diagnosis unlikely in the case illustrated.
Extraabdominal desmoid tumor: These are locally invasive tumors that do not metastasize. Their mam-mographic appearance mimics that of an invasive breast cancer, requiring biopsy for diagnosis. These, too, are rare, making the diagnosis unlikely in the case illustrated.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 5, highly suggestive of malignancy. Biopsy and other appropriate clinical action should be taken.
DIAGNOSIS
Infiltrating ductal carcinoma with metastatic carcinoma to axillary lymph nodes
KEY FACTS
Clinical
 Breast cancer is the most common malignancy in American women, excluding skin cancers. After lung cancer, it is the second leading cause of cancer death among women.
Breast cancer is the most common malignancy in American women, excluding skin cancers. After lung cancer, it is the second leading cause of cancer death among women.
 According to current estimates, breast cancer will be diagnosed in approximately one in eight women in their lifetime.
According to current estimates, breast cancer will be diagnosed in approximately one in eight women in their lifetime.
 Invasive ductal carcinoma, not otherwise specified, comprises 65% to 80% of invasive breast cancers. The second most common type is invasive lobular carcinoma, accounting for 3% to 14% of cases. Other, less common specific forms of ductal carcinoma include medullary, mucinous, papillary, and tubular carcinoma.
Invasive ductal carcinoma, not otherwise specified, comprises 65% to 80% of invasive breast cancers. The second most common type is invasive lobular carcinoma, accounting for 3% to 14% of cases. Other, less common specific forms of ductal carcinoma include medullary, mucinous, papillary, and tubular carcinoma.
Radiologic
 A spiculated mass, characterized by lines radiating outward from a central mass, is the most common mam-mographic appearance for invasive ductal carcinoma.
A spiculated mass, characterized by lines radiating outward from a central mass, is the most common mam-mographic appearance for invasive ductal carcinoma.
 Spiculated margins usually signify invasion.
Spiculated margins usually signify invasion.
 Spiculated projections result from (1) a desmoplastic response (connective tissue proliferation) that distorts the adjacent tissue, (2) tumor infiltrating into the surrounding tissue, or (3) both conditions.
Spiculated projections result from (1) a desmoplastic response (connective tissue proliferation) that distorts the adjacent tissue, (2) tumor infiltrating into the surrounding tissue, or (3) both conditions.
 A spectrum of mammographic appearances can be seen with invasive ductal carcinoma, including (1) masses with either spiculated, microlobulated, indistinct, and circumscribed margins; (2) architectural distortion; and (3) focal asymmetric or developing densities.
A spectrum of mammographic appearances can be seen with invasive ductal carcinoma, including (1) masses with either spiculated, microlobulated, indistinct, and circumscribed margins; (2) architectural distortion; and (3) focal asymmetric or developing densities.
 Ultrasound often shows an irregular, hypoechoic, shadowing mass that can have ill-defined, microlobulated, or spiculated margins.
Ultrasound often shows an irregular, hypoechoic, shadowing mass that can have ill-defined, microlobulated, or spiculated margins.
SUGGESTED READING
Adler DD. Mammographic evaluation of masses. In DB Kopans (ed). Syllabus: A Categorical Course in Breast Imaging. Oak Brook, IL: RSNA, 1995:107–116.
De Paredes ES. Atlas of Film-Screen Mammography. Baltimore, MD: Williams & Wilkins, 1992.
Feig SA. Breast masses: mammographic and sonographic evaluation. Radiol Clin North Am 1992;30:67–92.
Smith RA. The epidemiology of breast cancer. In DB Kopans (ed). Syllabus: A Categorical Course in Breast Imaging. Oak Brook, IL: RSNA, 1995:7–20.
Yang WT, Hennessy B, Broglio K, et al. Imaging differences in metaplastic and invasive ductal carcinomas of the breast. Am J Roentgenol 2007;189:1288–1293.
MARGARET E.
WILLIFORD AND
MARY SCOTT SOO
HISTORY
Annual diagnostic mammogram in a 70-year-old woman, status post right lumpectomy in the upper central breast and radiation therapy for treatment of carcinoma.
 FIGURES 2-4A and 2-4B Mediolateral oblique (A) and craniocaudal (B) mammograms of right and left breasts show scattered fibroglandular tissue bilaterally. Right breast shows focal asymmetry and focal distortion with coarse benign dystrophic calcification in the superior medial quadrant.
FIGURES 2-4A and 2-4B Mediolateral oblique (A) and craniocaudal (B) mammograms of right and left breasts show scattered fibroglandular tissue bilaterally. Right breast shows focal asymmetry and focal distortion with coarse benign dystrophic calcification in the superior medial quadrant.
 Postoperative and postradiation changes of right breast: This is the best diagnosis, given the history and correlation of architectural distortion and coarse dystrophic calcification to the site of lumpectomy.
Postoperative and postradiation changes of right breast: This is the best diagnosis, given the history and correlation of architectural distortion and coarse dystrophic calcification to the site of lumpectomy.
 Edema: This diagnosis is less likely because edema is commonly bilateral, with no associated mass or focal distortion. Correlation with physical exam is helpful.
Edema: This diagnosis is less likely because edema is commonly bilateral, with no associated mass or focal distortion. Correlation with physical exam is helpful.
 Inflammatory carcinoma: Inflammatory carcinoma has prominent, diffuse asymmetric density and skin thickening. In its pure form, there is no focal mass or distortion, but in many cases, there is a focal mass-like density. Clinical presentation and physical exam are important correlates, which demonstrate an erythema-tous, nontender breast with peau d’orange appearance of the skin. This diagnosis is considered less likely due to the history of radiation therapy. Inflammatory carcinoma also would not be expected to be associated with dystrophic calcifications.
Inflammatory carcinoma: Inflammatory carcinoma has prominent, diffuse asymmetric density and skin thickening. In its pure form, there is no focal mass or distortion, but in many cases, there is a focal mass-like density. Clinical presentation and physical exam are important correlates, which demonstrate an erythema-tous, nontender breast with peau d’orange appearance of the skin. This diagnosis is considered less likely due to the history of radiation therapy. Inflammatory carcinoma also would not be expected to be associated with dystrophic calcifications.
 Mastitis: Mastitis presents with a clinical history of tenderness and fever, not present in this case. Physical exam reveals cutaneous inflammatory changes and tenderness. Focal mass is usually not present unless there is an abscess. Biopsy is indicated if there is incomplete resolution with antibiotic therapy.
Mastitis: Mastitis presents with a clinical history of tenderness and fever, not present in this case. Physical exam reveals cutaneous inflammatory changes and tenderness. Focal mass is usually not present unless there is an abscess. Biopsy is indicated if there is incomplete resolution with antibiotic therapy.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 2, benign. Recommend annual mammography.
DIAGNOSIS
Postoperative and postradiation changes following lumpectomy and radiation therapy
KEY FACTS
Clinical
 Lumpectomy creates focal distortion of normal breast parenchyma at the site of the tumor. Radiation causes fibrosis throughout the breast and can enhance the distortion created by the surgical excision.
Lumpectomy creates focal distortion of normal breast parenchyma at the site of the tumor. Radiation causes fibrosis throughout the breast and can enhance the distortion created by the surgical excision.
 Skin thickening and asymmetry in breast size may be evident on clinical exam.
Skin thickening and asymmetry in breast size may be evident on clinical exam.
Radiologic
 Diagnosis of postoperative distortion can be confirmed by correlating posttherapy films with preoperative films showing the site of the tumor and needle localization done before the surgical excision. Scar markers can also be placed on the skin at the site of surgical scar, aiding in correlating the distortion with the surgical site.
Diagnosis of postoperative distortion can be confirmed by correlating posttherapy films with preoperative films showing the site of the tumor and needle localization done before the surgical excision. Scar markers can also be placed on the skin at the site of surgical scar, aiding in correlating the distortion with the surgical site.
 Postoperative distortion and asymmetric increased density due to surgery and radiation are most prominent on the first posttherapy mammogram done 6 to 12 months after therapy.
Postoperative distortion and asymmetric increased density due to surgery and radiation are most prominent on the first posttherapy mammogram done 6 to 12 months after therapy.
 Distortion and asymmetric density gradually stabilize or resolve over time, usually 2.5 to 3.0 years following therapy.
Distortion and asymmetric density gradually stabilize or resolve over time, usually 2.5 to 3.0 years following therapy.
 Benign, dystrophic calcifications are a commonly associated finding, particularly at the lumpectomy site. Radiation and surgery can also cause benign fat necrosis calcifications.
Benign, dystrophic calcifications are a commonly associated finding, particularly at the lumpectomy site. Radiation and surgery can also cause benign fat necrosis calcifications.
 Recurrent tumor can occur at the site of the primary tumor; therefore, magnification views of the lumpec-tomy site are routinely performed during annual diagnostic mammography. Increased mass, distortion, or malignant-appearing calcifications are signs that may indicate recurrence. These findings should prompt biopsy.
Recurrent tumor can occur at the site of the primary tumor; therefore, magnification views of the lumpec-tomy site are routinely performed during annual diagnostic mammography. Increased mass, distortion, or malignant-appearing calcifications are signs that may indicate recurrence. These findings should prompt biopsy.
SUGGESTED READING
Dershaw DD. Evaluation of the breast undergoing lumpectomy and radiation therapy. Radiol Clin North Am 1995;33:1147–1160.
Mendelson EB. Evaluation of the post-operative breast. Radiol Clin North Am 1992;30:107–138.
Preda L, Villa G, Rizzo S, et al. Magnetic resonance mammography in the evaluation of recurrence at the prior lumpectomy site after conservative surgery and radiotherapy. Breast Cancer Res 2006;8:R53.
MARY SCOTT SOO
HISTORY
Diagnostic mammogram in a 33-year-old woman with pain in her left breast. Sixteen years ago she underwent breast augmentation with silicone implants; the right implant was ruptured and replaced 3 years before the mammogram shown in Figure 2-5A. One year prior to the mammogram shown in Figure 2-5B, she underwent explantation of both implants.
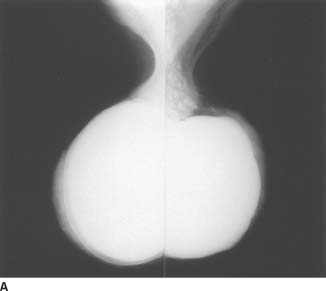
 FIGURE 2-5A Mediolateral oblique mammograms of both breasts. Bilateral subglandular implants are present. On the left, the contour of the single-lumen silicone implant is lobulated, and multiple high-density nodules are seen in the left axilla. On the right, a double-lumen implant is present with the outer saline lumen intact.
FIGURE 2-5A Mediolateral oblique mammograms of both breasts. Bilateral subglandular implants are present. On the left, the contour of the single-lumen silicone implant is lobulated, and multiple high-density nodules are seen in the left axilla. On the right, a double-lumen implant is present with the outer saline lumen intact.

 FIGURE 2-5B Repeat mediolateral oblique mammograms of both breasts 1 year after explantation of the prostheses. The prostheses have been removed. There are persistent high-density nodules within the left axilla. No mammographic abnormality is seen within either breast.
FIGURE 2-5B Repeat mediolateral oblique mammograms of both breasts 1 year after explantation of the prostheses. The prostheses have been removed. There are persistent high-density nodules within the left axilla. No mammographic abnormality is seen within either breast.
 Ruptured silicone implant with free silicone extravasation into the left axilla: This is the best diagnosis because the high-density nodules in the axilla are equal in density to the silicone prosthesis, resulting from migration of free silicone away from the ruptured prosthesis. The lobulated contour of the prosthesis is not specific for implant rupture if seen as an isolated finding but should raise the question of rupture and prompt further evaluation.
Ruptured silicone implant with free silicone extravasation into the left axilla: This is the best diagnosis because the high-density nodules in the axilla are equal in density to the silicone prosthesis, resulting from migration of free silicone away from the ruptured prosthesis. The lobulated contour of the prosthesis is not specific for implant rupture if seen as an isolated finding but should raise the question of rupture and prompt further evaluation.
 Breast carcinoma metastatic to axillary lymph nodes: This diagnosis is unlikely because the density of the nodules in the axilla is equal to silicone, higher even than expected for nodes involved with metastatic disease. In addition, there are no breast lesions that are suspicious for carcinoma.
Breast carcinoma metastatic to axillary lymph nodes: This diagnosis is unlikely because the density of the nodules in the axilla is equal to silicone, higher even than expected for nodes involved with metastatic disease. In addition, there are no breast lesions that are suspicious for carcinoma.
 Sarcoidosis: Axillary lymph nodes can be seen at mammography in patients with sarcoidosis. However, the process is usually bilateral, and nodes are usually enlarged. Abnormal lymph nodes associated with sar-coidosis are denser than normal fatty-replaced lymph nodes but do not have density as high as silicone, making this an unlikely diagnosis in this case.
Sarcoidosis: Axillary lymph nodes can be seen at mammography in patients with sarcoidosis. However, the process is usually bilateral, and nodes are usually enlarged. Abnormal lymph nodes associated with sar-coidosis are denser than normal fatty-replaced lymph nodes but do not have density as high as silicone, making this an unlikely diagnosis in this case.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 2, Benign. Further evaluation of free silicone in the left axilla should be based on clinical examination.
DIAGNOSIS
Ruptured silicone prosthesis on the left, with residual free silicone seen 1 year later
KEY FACTS
Clinical
 Rupture of prostheses (intracapsular or extracapsular) is considered a major complication of prosthesis placement, which necessitates surgical explantation of the ruptured implant.
Rupture of prostheses (intracapsular or extracapsular) is considered a major complication of prosthesis placement, which necessitates surgical explantation of the ruptured implant.
 Intracapsular rupture occurs when the gel escaping from a ruptured implant is contained within the surrounding fibrous capsule.
Intracapsular rupture occurs when the gel escaping from a ruptured implant is contained within the surrounding fibrous capsule.
 Extracapsular rupture occurs when free silicone from a ruptured implant extends outside of the fibrous capsule. This free silicone is difficult to remove completely at surgery and can stimulate a granulomatous reaction within the breast.
Extracapsular rupture occurs when free silicone from a ruptured implant extends outside of the fibrous capsule. This free silicone is difficult to remove completely at surgery and can stimulate a granulomatous reaction within the breast.
 Silicone granulomas can cause a palpable mass, which is difficult to differentiate from carcinoma.
Silicone granulomas can cause a palpable mass, which is difficult to differentiate from carcinoma.
Radiologic
 When extracapsular free silicone is present, the diagnosis of rupture can often be made mammographically because the density of the free silicone within the breast tissue is higher than that of other structures.
When extracapsular free silicone is present, the diagnosis of rupture can often be made mammographically because the density of the free silicone within the breast tissue is higher than that of other structures.
 The presence of extracapsular silicone is often diagnostic of implant rupture. However, sometimes prior films are needed to document the source of the rupture. For instance, in a patient in whom a previously ruptured implant has been replaced, prior films would be needed to determine which implant was the source of the extracapsular silicone.
The presence of extracapsular silicone is often diagnostic of implant rupture. However, sometimes prior films are needed to document the source of the rupture. For instance, in a patient in whom a previously ruptured implant has been replaced, prior films would be needed to determine which implant was the source of the extracapsular silicone.
 Ruptures that occur posteriorly or ruptures in which only a small amount of silicone escapes into the breast parenchyma may not be detected mammographically because they are either not included on the image or the dense prosthesis obscures visualization of the free silicone. In these situations, other imaging studies, such as MRI or sonography, are necessary to make the diagnosis.
Ruptures that occur posteriorly or ruptures in which only a small amount of silicone escapes into the breast parenchyma may not be detected mammographically because they are either not included on the image or the dense prosthesis obscures visualization of the free silicone. In these situations, other imaging studies, such as MRI or sonography, are necessary to make the diagnosis.
 Mammography cannot detect intracapsular rupture reliably. MRI has the highest sensitivity and specificity for diagnosing intracapsular rupture.
Mammography cannot detect intracapsular rupture reliably. MRI has the highest sensitivity and specificity for diagnosing intracapsular rupture.
SUGGESTED READING
Berg WA, Caskey CI, Hamper UM, et al. Diagnosing breast implant rupture with MR imaging, US, and mammography. Radiographics 1993;13:1323–1336.
Berg WA, Caskey CI, Hamper UM, et al. Single- and double-lumen silicone breast implant integrity: prospective evaluation of MR and US criteria. Radiology 1995;197:45–52.
Caskey CI, Berg WA, Hamper UM, et al. Imaging spectrum of extracapsu-lar silicone: correlation of US, MR imaging, mammographic, and histo-pathologic findings. Radiographics 1999;19 Spec No:S39–S51.
Destouet JM, Monsees BS, Oser RF, et al. Screening mammography in 350 women with breast implants: prevalence and findings of implant complications. Am J Roentgenol 1992;159:973–987.
Everson LI, Parantainen H, Detlie T, et al. Diagnosis of breast implant rupture: imaging findings and relative efficacies of imaging techniques. Am J Roentgenol 1994;163:57–60.
Gorczyca DP, Gorczyca SM, Gorczyca KL. The diagnosis of silicone breast implant rupture. Plast Reconstr Surg 2007;120:49S–61S.
Gorczyca DP, Sinha S, Ahn CY, et al. Silicone breast implants in vivo: MR imaging. Radiology 1992;185:407–410.
RUTH WALSH
AND
MARY SCOTT SOO
HISTORY
Diagnostic mammogram in a 52-year-old female, status post left mastectomy for breast cancer and right subcutaneous mastectomy with implant reconstruction.

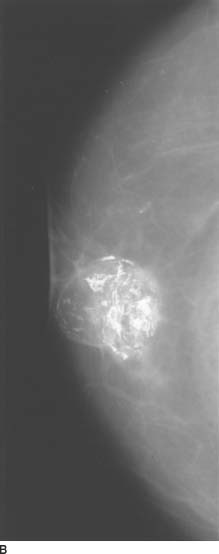
 FIGURES 2-6A and 2-6B Routine mediolateral oblique (A) and craniocaudal (B) “implant exclusion”or “push-back”mammograms of the right breast. Minimal residual fibroglandular tissue remains in the breast status post subcutaneous mastectomy. A 3-cm radiolucent mass with associated rim-like and dystrophic calcifications is present in the subareolar region. A submuscular silicone implant is partially visualized on the mediolateral oblique view.
FIGURES 2-6A and 2-6B Routine mediolateral oblique (A) and craniocaudal (B) “implant exclusion”or “push-back”mammograms of the right breast. Minimal residual fibroglandular tissue remains in the breast status post subcutaneous mastectomy. A 3-cm radiolucent mass with associated rim-like and dystrophic calcifications is present in the subareolar region. A submuscular silicone implant is partially visualized on the mediolateral oblique view.
 Fat necrosis: Low-density (fatty) masses in the breast are almost always benign. A low-density mass associated with dystrophic (bizarre, irregular, and plaquelike) calcifications, as is seen in this case, is most consistent with fat necrosis. Dystrophic calcifications can be seen with fat necrosis secondary to trauma, surgery, or radiation therapy.
Fat necrosis: Low-density (fatty) masses in the breast are almost always benign. A low-density mass associated with dystrophic (bizarre, irregular, and plaquelike) calcifications, as is seen in this case, is most consistent with fat necrosis. Dystrophic calcifications can be seen with fat necrosis secondary to trauma, surgery, or radiation therapy.
 Carcinoma: Malignant calcifications are usually <0.5 mm in size, ranging from minute up to 3 mm. Many of the calcifications in the case illustrated are >2 to 3 mm in size and have benign rim and plaque-like shapes, making carcinoma an unlikely diagnosis.
Carcinoma: Malignant calcifications are usually <0.5 mm in size, ranging from minute up to 3 mm. Many of the calcifications in the case illustrated are >2 to 3 mm in size and have benign rim and plaque-like shapes, making carcinoma an unlikely diagnosis.
 Fibroadenoma: Although fibroadenomas can contain large, bizarre, irregular calcifications, as seen in this case, involuting fibroadenomas typically contain coarse or “popcorn-like”calcifications. The mass in this case is not consistent with a fibroadenoma because it has low density, as opposed to fibroadenomas, which are water-density masses.
Fibroadenoma: Although fibroadenomas can contain large, bizarre, irregular calcifications, as seen in this case, involuting fibroadenomas typically contain coarse or “popcorn-like”calcifications. The mass in this case is not consistent with a fibroadenoma because it has low density, as opposed to fibroadenomas, which are water-density masses.
 Secondary hyperparathyroidism with metastatic calcifications: Patients with hypercalcemia can develop coarse amorphous calcifications within the breast. However, this is rare, and calcifications would not be expected to be rim-like or associated with a radiolucent mass, making this diagnosis unlikely.
Secondary hyperparathyroidism with metastatic calcifications: Patients with hypercalcemia can develop coarse amorphous calcifications within the breast. However, this is rare, and calcifications would not be expected to be rim-like or associated with a radiolucent mass, making this diagnosis unlikely.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 2, benign. Recommend annual screening mammography for the right breast.
DIAGNOSIS
Fat necrosis secondary to prior subcutaneous mastectomy surgery
KEY FACTS
Clinical
 Fat necrosis is an inflammatory response that is usually due to trauma or surgery but can be idiopathic.
Fat necrosis is an inflammatory response that is usually due to trauma or surgery but can be idiopathic.
 Fat necrosis can be difficult to distinguish from carcinoma on both physical examination and mam-mography.
Fat necrosis can be difficult to distinguish from carcinoma on both physical examination and mam-mography.
 Clinically, fat necrosis can present as a hard painless mass that is ill-defined and poorly mobile. Skin thickening or retraction may also be identified, increasing the clinical suspicion of carcinoma.
Clinically, fat necrosis can present as a hard painless mass that is ill-defined and poorly mobile. Skin thickening or retraction may also be identified, increasing the clinical suspicion of carcinoma.
 In some cases, the traumatic event leading to fat necrosis is forgotten or unknown.
In some cases, the traumatic event leading to fat necrosis is forgotten or unknown.
Radiologic
 At mammography, fat necrosis has a wide spectrum of appearances, ranging from well-defined oil cysts to spiculated masses that simulate carcinoma.
At mammography, fat necrosis has a wide spectrum of appearances, ranging from well-defined oil cysts to spiculated masses that simulate carcinoma.
 Calcifications are commonly associated with fat necrosis. When calcifications first appear, they can be small and pleomorphic, mimicking malignant calcifications. However, they usually evolve into larger, coarse, plaque-like calcifications that have a more benign appearance.
Calcifications are commonly associated with fat necrosis. When calcifications first appear, they can be small and pleomorphic, mimicking malignant calcifications. However, they usually evolve into larger, coarse, plaque-like calcifications that have a more benign appearance.
 Early dystrophic calcifications can be difficult to distinguish from malignancy. If calcifications cannot be assessed as benign following magnification mammography, then core biopsy may be warranted to exclude malignancy.
Early dystrophic calcifications can be difficult to distinguish from malignancy. If calcifications cannot be assessed as benign following magnification mammography, then core biopsy may be warranted to exclude malignancy.
SUGGESTED READING
De Paredes ES. Atlas of Film-Screen Mammography. Baltimore, MD: Williams & Wilkins, 1992.
Feig SA. Mammographic evaluation of calcifications. In DB Kopans, EB Mendelson (eds), Syllabus: A Categorical Course in Breast Imaging. Oak Brook, IL: RSNA, 1995.
Mendelson EB. Evaluation of the post operative breast. Radiol Clin North Am 1992;30:107–138.
Morrow M. Breast trauma, hematoma, and fat necrosis. In JR Harris, S Hellman, IC Henderson, DW Kinne (eds). Breast Disease. Philadelphia, PA: Lippincott, 1991.
Tan PH, Lai LM, Carrington EV, et al. Fat necrosis of the breast—a review. Breast 2006;15:313–318.
PHYLLIS J.
KORNGUTH
AND
MARY SCOTT SOO
HISTORY
Screening mammogram in a 36-year-old woman. The family history is significant for a sister with premenopausal breast carcinoma. The patient’s prior mammogram was normal.
 FIGURES 2-7A and 2-7B Mediolateral oblique (A) and craniocaudal (B) mammograms of the left breast show a large, well-circumscribed, solitary noncalcified mass located centrally in a predominantly fatty-replaced breast. The mass was new compared to the prior exam.
FIGURES 2-7A and 2-7B Mediolateral oblique (A) and craniocaudal (B) mammograms of the left breast show a large, well-circumscribed, solitary noncalcified mass located centrally in a predominantly fatty-replaced breast. The mass was new compared to the prior exam.

 FIGURE 2-7C Sonogram of the mass seen in Figures 2-7A and 2-7B shows a well-defined, solid hypoechoic mass with no posterior acoustic enhancement or shadowing.
FIGURE 2-7C Sonogram of the mass seen in Figures 2-7A and 2-7B shows a well-defined, solid hypoechoic mass with no posterior acoustic enhancement or shadowing.
 Fibroadenoma: The mammographic and sonographic features of this lesion, as well as the young age of the patient, are typical of a fibroadenoma.
Fibroadenoma: The mammographic and sonographic features of this lesion, as well as the young age of the patient, are typical of a fibroadenoma.
 Carcinoma: Some well-defined carcinomas (medullary, mucinous, papillary) can have these mammographic and sonographic features. However, these tumors are uncommon tumors, making this diagnosis less likely.
Carcinoma: Some well-defined carcinomas (medullary, mucinous, papillary) can have these mammographic and sonographic features. However, these tumors are uncommon tumors, making this diagnosis less likely.
 Phyllodes tumor: At mammography, phyllodes tumors are well-circumscribed, often large masses indistinguishable from fibroadenomas or other tumors. The sonographic appearance of a phyllodes tumor can be identical to the lesion in the case illustrated. However, many phyllodes tumors contain cystic spaces, producing a more heterogeneous sonographic appearance.
Phyllodes tumor: At mammography, phyllodes tumors are well-circumscribed, often large masses indistinguishable from fibroadenomas or other tumors. The sonographic appearance of a phyllodes tumor can be identical to the lesion in the case illustrated. However, many phyllodes tumors contain cystic spaces, producing a more heterogeneous sonographic appearance.
 Cyst: The mammographic features of a cyst can be identical to the appearance of the mass in this case. However, the sonogram reveals a solid mass, not a simple cyst.
Cyst: The mammographic features of a cyst can be identical to the appearance of the mass in this case. However, the sonogram reveals a solid mass, not a simple cyst.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 4-A. Low suspicion for malignancy. Biopsy should be considered.
DIAGNOSIS
Fibroadenoma
KEY FACTS
Clinical
 Fibroadenomas are common benign breast lesions that occur in premenopausal and perimenopausal age groups.
Fibroadenomas are common benign breast lesions that occur in premenopausal and perimenopausal age groups.
 On physical examination, the mass is usually firm, well-defined, and mobile.
On physical examination, the mass is usually firm, well-defined, and mobile.
 Growth of fibroadenomas is stimulated by hormonal influence.
Growth of fibroadenomas is stimulated by hormonal influence.
 Fibroadenomas can be multiple and bilateral. Multiplicity and bilaterality are more common in black women.
Fibroadenomas can be multiple and bilateral. Multiplicity and bilaterality are more common in black women.
Radiologic
 Biopsy is the standard of care for management of any new mammographic mass that is solid on ultrasound.
Biopsy is the standard of care for management of any new mammographic mass that is solid on ultrasound.
 In the case illustrated, the mass had benign features by mammographic and sonographic criteria, including oval shape and circumscribed margins; however, biopsy is the standard of care because the mass was new. The BI-RADS Category 4-A reflects the fact that the lesion has a low suspicion for malignancy, given the high likelihood that it was a fibroadenoma.
In the case illustrated, the mass had benign features by mammographic and sonographic criteria, including oval shape and circumscribed margins; however, biopsy is the standard of care because the mass was new. The BI-RADS Category 4-A reflects the fact that the lesion has a low suspicion for malignancy, given the high likelihood that it was a fibroadenoma.
 Ultrasound-guided core biopsy is frequently performed to make the diagnosis because it is less invasive and less expensive than open surgical biopsy, yet it allows for surgical planning if a malignancy is diagnosed.
Ultrasound-guided core biopsy is frequently performed to make the diagnosis because it is less invasive and less expensive than open surgical biopsy, yet it allows for surgical planning if a malignancy is diagnosed.
 If a noncalcified, well-circumscribed, benign-appearing solid mass is identified on a baseline screening mammogram (i.e., the mass is not palpable and there is no evidence that the mass is new), then 6-month follow-up mammography (BI-RADS Category 3, probably benign finding) would be an acceptable final assessment category and follow-up recommendation.
If a noncalcified, well-circumscribed, benign-appearing solid mass is identified on a baseline screening mammogram (i.e., the mass is not palpable and there is no evidence that the mass is new), then 6-month follow-up mammography (BI-RADS Category 3, probably benign finding) would be an acceptable final assessment category and follow-up recommendation.
SUGGESTED READING
Liberman L, Bonaccio E, Hamele-Bena D, et al. Benign and malignant phyllodes tumors: mammographic and sonographic findings. Radiology 1996;198:122–124.
Sickles EA. Nonpalpable, circumscribed, noncalcified solid breast masses: likelihood of malignancy based on lesion size and age of patient. Radiology 1994;192:439–442.
Skaane P, Engedal K. Analysis of sonographic features in the differentiation of fibroadneoma and invasive ductal carcinoma. Am J Roentgenol 1998;170:109–114.
Sklair-Levy M, Sella T, Alweiss T, et al. Incidence and management of complex fibroadneomas. Am J Roentgenol 2008;190:214–218.
Smith BL. Fibroadenomas. In JR Harris, S Hellman, IC Henderson, DW Kinne (eds). Breast Diseases. Philadelphia, PA: Lippincott, 1991:34–37.
MARGARET E.
WILLIFORD
AND
MARY SCOTT SOO
HISTORY
Screening mammogram in a 49-year-old premenopausal woman. She had no palpable abnormality or history of surgery.
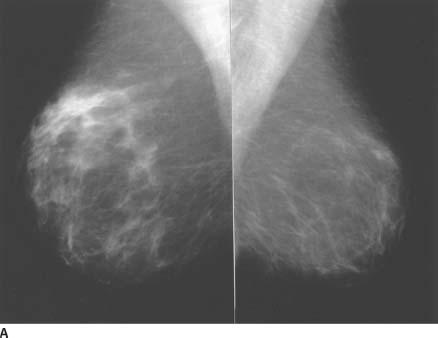
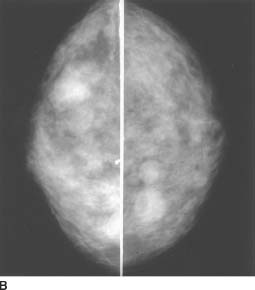
 FIGURE 2-8A There is scattered fibroglandular tissue in the left breast and heterogeneously dense tissue in the right breast. Mediolateral oblique mammograms of right and left breasts show global asymmetry in the lateral right breast.
FIGURE 2-8A There is scattered fibroglandular tissue in the left breast and heterogeneously dense tissue in the right breast. Mediolateral oblique mammograms of right and left breasts show global asymmetry in the lateral right breast.
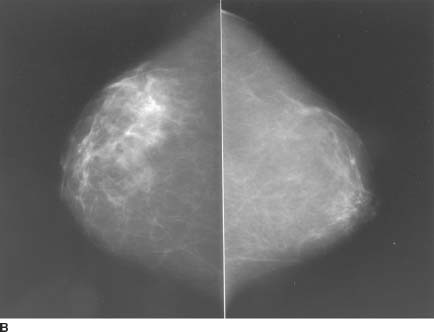
 FIGURE 2-8B Craniocaudal mammograms of right and left breasts show global asymmetry in the outer right breast.
FIGURE 2-8B Craniocaudal mammograms of right and left breasts show global asymmetry in the outer right breast.
 Global asymmetry of fibroglandular tissue: This is the best diagnosis because the asymmetry is dispersed throughout the lateral right breast and has the appearance of normal parenchyma with no underlying suspicious characteristics. No corresponding palpable mass was identified to raise the suspicion for other processes.
Global asymmetry of fibroglandular tissue: This is the best diagnosis because the asymmetry is dispersed throughout the lateral right breast and has the appearance of normal parenchyma with no underlying suspicious characteristics. No corresponding palpable mass was identified to raise the suspicion for other processes.
 Postoperative change with removal of breast tissue from the contralateral breast: This diagnosis is unlikely because there is no history of prior breast surgery.
Postoperative change with removal of breast tissue from the contralateral breast: This diagnosis is unlikely because there is no history of prior breast surgery.
 Carcinoma: Although carcinoma may rarely present as global asymmetry, there is no associated palpable mass or associated suspicious mammographic feature to suggest malignancy.
Carcinoma: Although carcinoma may rarely present as global asymmetry, there is no associated palpable mass or associated suspicious mammographic feature to suggest malignancy.
 Focal asymmetry: This diagnosis is unlikely because the asymmetry involves a large area of the breast.
Focal asymmetry: This diagnosis is unlikely because the asymmetry involves a large area of the breast.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 3, probably benign. A 6-month interval follow-up is suggested.
DIAGNOSIS
Global asymmetry of breast tissue
KEY FACTS
Clinical
 At least 3% of women have asymmetric breast tissue that appears as an increased volume or asymmetry relative to the contralateral breast. This is most commonly seen in the upper outer quadrants. It reflects normal asymmetric development or variable response to hormonal stimulation.
At least 3% of women have asymmetric breast tissue that appears as an increased volume or asymmetry relative to the contralateral breast. This is most commonly seen in the upper outer quadrants. It reflects normal asymmetric development or variable response to hormonal stimulation.
 The area of asymmetry should be evaluated with a careful physical breast examination. If there is a palpable abnormality or palpable asymmetry, biopsy should be recommended.
The area of asymmetry should be evaluated with a careful physical breast examination. If there is a palpable abnormality or palpable asymmetry, biopsy should be recommended.
 A clinical history of prior breast surgery is important. For instance, asymmetry can be due to removal of tissue during biopsy of the contralateral breast.
A clinical history of prior breast surgery is important. For instance, asymmetry can be due to removal of tissue during biopsy of the contralateral breast.
Radiologic
 Asymmetries are areas of glandular density that are differentiated from masses in that they lack convex borders or evidence of a 3D mass. Two types of asymmetries are defined in the Breast Imaging Reporting and Data System, 4th edition: “global”asymmetries and “focal”asymmetries.
Asymmetries are areas of glandular density that are differentiated from masses in that they lack convex borders or evidence of a 3D mass. Two types of asymmetries are defined in the Breast Imaging Reporting and Data System, 4th edition: “global”asymmetries and “focal”asymmetries.
 Global asymmetry involves a larger area of the breast (at least one quadrant) compared to focal asymmetry and is only rarely a secondary sign of malignancy. Global asymmetry represents a normal variant if the glandular structures and fat are normally dispersed in the area with no mass, distortion, or microcalcifications, and no corresponding palpable abnormality.
Global asymmetry involves a larger area of the breast (at least one quadrant) compared to focal asymmetry and is only rarely a secondary sign of malignancy. Global asymmetry represents a normal variant if the glandular structures and fat are normally dispersed in the area with no mass, distortion, or microcalcifications, and no corresponding palpable abnormality.
 Additional mammographic views, including magnification compression images, are necessary to evaluate the global asymmetry for underlying mass, architectural distortion, or subtle microcalcifications.
Additional mammographic views, including magnification compression images, are necessary to evaluate the global asymmetry for underlying mass, architectural distortion, or subtle microcalcifications.
 Comparison with prior films should be performed to assess stability of the asymmetry, or if no prior films are available, a 6-month mammographic follow-up is recommended to document the stability of the pattern.
Comparison with prior films should be performed to assess stability of the asymmetry, or if no prior films are available, a 6-month mammographic follow-up is recommended to document the stability of the pattern.
 Focal asymmetry involves a smaller area of breast and is of more concern at mammography. Magnification compression images and sometimes ultrasound are necessary to exclude an underlying mass in an area of focal asymmetry.
Focal asymmetry involves a smaller area of breast and is of more concern at mammography. Magnification compression images and sometimes ultrasound are necessary to exclude an underlying mass in an area of focal asymmetry.
SUGGESTED READING
American College of Radiology (ACR). ACR BI-RADS—mammography. In ACR Breast Imaging Reporting and Data System, Breast Imaging Atlas. Reston, VA: American College of Radiology, 2003;253–254.
Kopans DB (ed). Breast Imaging. Philadelphia, PA: Lippincott, 1989.
Kopans DB, Swann CA, White CA, et al. Asymmetric breast tissue. Radiology 1989;171:639–643.
Sickles, EA. The spectrum of breast asymmetries: imaging features, work-up and management. Radiol Clin North Am 2007;45:765–771.
RUTH WALSH
AND
MARY SCOTT SOO
HISTORY
A 43-year-old asymptomatic woman presenting for a screening mammogram.
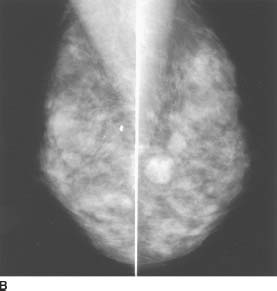
 FIGURES 2-9A and 2-9B Mediolateral oblique mammograms of both breasts (A) and craniocaudal mammogram of the right breast (B) show extremely dense fibroglandular tissue. There is a circumscribed 3- x 2-cm mass present in the upper outer quadrant of the right breast. This mass contains both radiolucent regions and regions that are isodense to parenchyma.
FIGURES 2-9A and 2-9B Mediolateral oblique mammograms of both breasts (A) and craniocaudal mammogram of the right breast (B) show extremely dense fibroglandular tissue. There is a circumscribed 3- x 2-cm mass present in the upper outer quadrant of the right breast. This mass contains both radiolucent regions and regions that are isodense to parenchyma.
 Hamartoma (fibroadenolipoma): The encapsulated, well-circumscribed mass with internal fat and fibroglandular tissue in disorganized array seen in the upper lateral right breast is typical of a hamartoma. These findings make hamartoma the best diagnosis.
Hamartoma (fibroadenolipoma): The encapsulated, well-circumscribed mass with internal fat and fibroglandular tissue in disorganized array seen in the upper lateral right breast is typical of a hamartoma. These findings make hamartoma the best diagnosis.
 Intramammary lymph node: Normal intramammary lymph nodes are typically round, oval, or lobulated isodense masses that measure <1 cm in size and usually contain a central fatty hilum. The size of the lesion presented here and the haphazardly arranged fatty and soft tissue components make the lymph node an unlikely diagnosis.
Intramammary lymph node: Normal intramammary lymph nodes are typically round, oval, or lobulated isodense masses that measure <1 cm in size and usually contain a central fatty hilum. The size of the lesion presented here and the haphazardly arranged fatty and soft tissue components make the lymph node an unlikely diagnosis.
 Galactocele: Galactoceles are milk-containing cysts that appear as a radiolucent or mixed-density circumscribed mass that can have a mottled appearance, mimicking a hamartoma. A fat-fluid level can be seen on a horizontal beam radiograph, which is not present in this case. This diagnosis is also unlikely in the present case because there is no history of current or recent lactation.
Galactocele: Galactoceles are milk-containing cysts that appear as a radiolucent or mixed-density circumscribed mass that can have a mottled appearance, mimicking a hamartoma. A fat-fluid level can be seen on a horizontal beam radiograph, which is not present in this case. This diagnosis is also unlikely in the present case because there is no history of current or recent lactation.
 Lipoma: Lipomas are circumscribed, fat-containing masses that are radiolucent on mammograms. However, in addition to radiolucent regions, the lesion presented here has regions that are isodense with breast parenchyma. This finding would not be found in a pure lipoma and makes this diagnosis unlikely.
Lipoma: Lipomas are circumscribed, fat-containing masses that are radiolucent on mammograms. However, in addition to radiolucent regions, the lesion presented here has regions that are isodense with breast parenchyma. This finding would not be found in a pure lipoma and makes this diagnosis unlikely.
 Oil cyst: Oil cysts would also be a consideration in a lesion that was predominantly radiolucent. Again, the mixed density arranged in a haphazard pattern argues against this diagnosis in the case illustrated.
Oil cyst: Oil cysts would also be a consideration in a lesion that was predominantly radiolucent. Again, the mixed density arranged in a haphazard pattern argues against this diagnosis in the case illustrated.
After assessing the imaging findings and considering the differential diagnosis, the final assessment is BI-RADS Category 2, benign. Recommend annual screening mammography.
DIAGNOSIS
Hamartoma
KEY FACTS
Clinical
 Hamartomas are uncommon, benign breast tumors containing ducts, lobules, adipose tissue, and fibrous tissue in varying proportions. Smooth muscle can also be present.
Hamartomas are uncommon, benign breast tumors containing ducts, lobules, adipose tissue, and fibrous tissue in varying proportions. Smooth muscle can also be present.
 Hamartomas can be discovered incidentally on screening mammography or present clinically as a painless breast lump or enlarging breast.
Hamartomas can be discovered incidentally on screening mammography or present clinically as a painless breast lump or enlarging breast.
 When palpable, hamartomas are usually firm, smooth, and mobile.
When palpable, hamartomas are usually firm, smooth, and mobile.
 Hamartomas usually grow slowly but can reach a large size, producing marked asymmetry of the breast. In these cases, surgical excision may be performed.
Hamartomas usually grow slowly but can reach a large size, producing marked asymmetry of the breast. In these cases, surgical excision may be performed.
Radiologic
 The characteristic mammographic appearance of a hamartoma is a circumscribed oval or round mass composed of mixed radiolucent and radiodense areas. This classic appearance is pathognomonic for a hamartoma, obviating the need for surgical excision.
The characteristic mammographic appearance of a hamartoma is a circumscribed oval or round mass composed of mixed radiolucent and radiodense areas. This classic appearance is pathognomonic for a hamartoma, obviating the need for surgical excision.
 Not all hamartomas have a classic mammographic appearance. The mass can vary from relatively radiolucent to very dense, depending on the proportions of fibrous and fatty tissue. Sometimes the mass can be uniformly dense with obscured margins. In these cases, the appearance is nonspecific, and biopsy may be required for diagnosis.
Not all hamartomas have a classic mammographic appearance. The mass can vary from relatively radiolucent to very dense, depending on the proportions of fibrous and fatty tissue. Sometimes the mass can be uniformly dense with obscured margins. In these cases, the appearance is nonspecific, and biopsy may be required for diagnosis.
 The mass displaces adjacent fibroglandular tissue, often leaving a thin intervening radiolucent zone. It usually has a well-defined margin and can appear encapsulated.
The mass displaces adjacent fibroglandular tissue, often leaving a thin intervening radiolucent zone. It usually has a well-defined margin and can appear encapsulated.
 If small or in a dense breast, hamartomas can be inapparent at mammography.
If small or in a dense breast, hamartomas can be inapparent at mammography.
SUGGESTED READING
Dean D, Trus T, D’souza TJ, et al. Hamartoma of the breast, an underrecognized breast lesion. Am J Clin Pathol 1995;103:685–689.
Georgian-Smith D, Kricun B, McKee G, et al. The mammary hamartoma: appreciation of additional imaging characteristics. J Ultrasound Med 2004;23:1267–1273.
Helvie MA, Adler DD, Rebner M, Oberman HA. Breast hamartomas: variable mammographic appearance. Radiology 1989;170:417–421.
Kopans DB (ed). Breast Imaging. Philadelphia, PA: Lippincott, 1989.
McGuire LI, Cohn D. Hamartoma of the breast. Aust N Z J Surg 1991;61: 713–716.
Murat A, Ozdemir H, Yildirim H, et al. Hamartoma of the breast. Australas Radiol 2007;51:B37–B39.
MARY SCOTT SOO
HISTORY
Screening mammogram in a 36-year-old asymptomatic woman with no past surgical history. She has no palpable breast masses.
 FIGURES 2-10A and 2-10B True lateral (A) and craniocaudal (B) mammograms of the right breast demonstrate extremely dense fibroglandular tissue. A 3-cm area of architectural distortion is present in the upper central right breast. Numerous calcifications are associated with the distortion.
FIGURES 2-10A and 2-10B True lateral (A) and craniocaudal (B) mammograms of the right breast demonstrate extremely dense fibroglandular tissue. A 3-cm area of architectural distortion is present in the upper central right breast. Numerous calcifications are associated with the distortion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


