Congenital Heart Disease
QUESTIONS
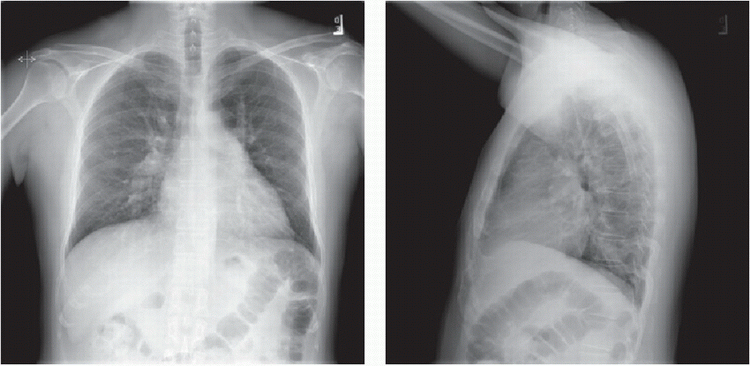
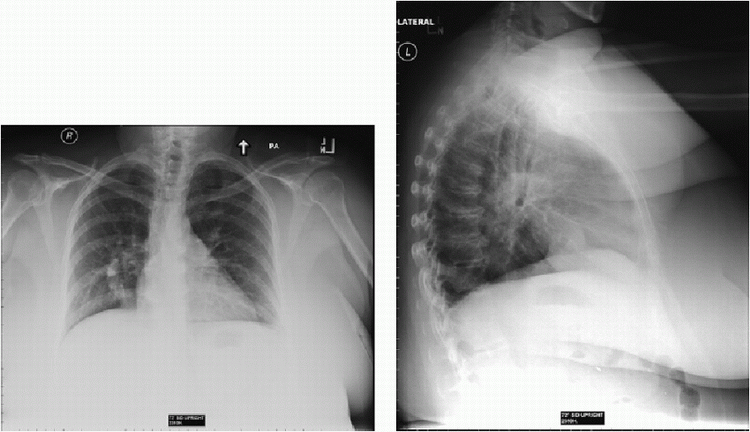
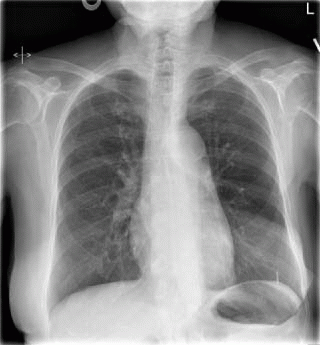
1a A 48-year-old male with heart murmur. What is the most likely underlying condition based on the chest radiographs?
|
A. Aortic stenosis
B. Mitral stenosis
C. Atrial septal defect (ASD)
D. Normal
E. Ebstein anomaly
View Answer
1a Answer C. Frontal and lateral chest radiographs demonstrate an enlarged pulmonary artery trunk and increased vascular flow. This is suggestive of underlying left to right shunting which can be caused by an atrial septal defect. Both aortic and mitral stenosis should not give an enlarged pulmonary artery trunk nor increased vascular flow. The findings are not normal given the enlarged pulmonary trunk and increased pulmonary flow. Ebstein anomaly would give a markedly enlarged right heart (e.g., boxed-shaped heart).
References: Baron MG, Book WM. Congenital heart disease in the adult: 2004. Radiol Clin North Am 2004;42(3):675-690, vii. Review.
Steiner RM, Gross GW, Flicker S, et al. Congenital heart disease in the adult patient: the value of plain film chest radiology. J Thorac Imaging 1995;10(1):1-25. Review.
A. Qp/Qs > 2
B. Atrial fibrillation
C. Lack of adequate rims
D. Bilateral iliac artery thrombosis
View Answer
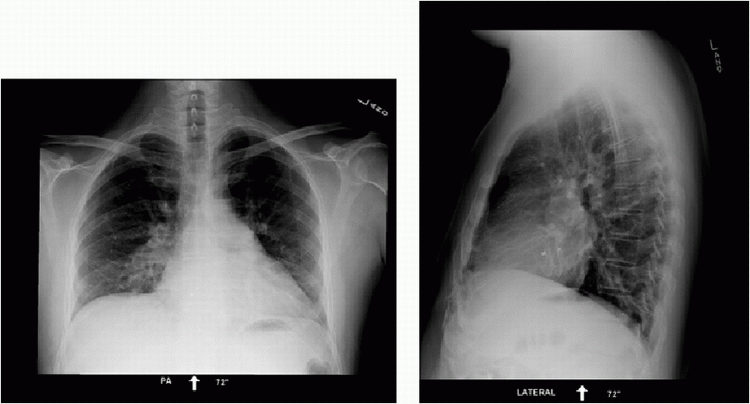
1b Answer C. An Amplatzer septal occluder is now seen on the chest radiograph. Indications for percutaneous atrial septal defect (ASD) closure include hemodynamically significant ASD (such as Qp/Qs > 2) and paradoxical emboli. It is not indicated in patients with small secundum ASD of no hemodynamic significance. It is also not indicated in septum primum, sinus venosus, and unroofed coronary sinus type of ASDs. Atrial fibrillation is not a contraindication to ASD closure. Adequate rims are required for the placement of the Amplatzer device. Only venous access is needed to deploy the device.
References: Kazmouz S, Kenny D, Cao QL, et al. Transcatheter closure of secundum atrial septal defects. J Invasive Cardiol 2013;25(5):257-264. Review.
Lee EY, Siegel MJ, Chu CM, et al. Amplatzer atrial septal defect occluder for pediatric patients: radiographic appearance. Radiology 2004;233(2):471-476.
1c Which of the following is a potential long-term complication of septal occluder device placement?
A. Atrial fibrillation
B. Heart block
C. Embolization/malpositioning
D. Erosion of the device
View Answer
1c Answer D. Complications of ASD occlusion include atrial fibrillation, SVT, heart block, device malposition, embolization, and erosion. The most common immediate complication is device embolization and malpositioning. Atrial fibrillation and heart block also typically occur early. Cardiac erosion is a long-term complication that can be difficult to detect.
References: Crawford GB, Brindis RG, Krucoff MW, et al. Percutaneous atrial septal occluder devices and cardiac erosion: a review of the literature. Catheter Cardiovasc Interv 2012;80(2):157-167. doi: 10.1002/ccd.24347. Epub 2012 May 2. Review.
Lee T, Tsai IC, Fu YC, et al. MDCT evaluation after closure of atrial septal defect with an Amplatzer septal occluder. AJR Am J Roentgenol 2007;188(5):W431-W439. PubMed PMID: 17449739.
A. Medical
B. Surgical
C. Endovascular
D. None
View Answer
2 Answer B. This is an inferior type of sinus venosus atrial septal defect (ASD) associated with anomalous pulmonary venous return of the right inferior pulmonary vein. The treatment is surgical. While secundum ASD can potentially be treated endovascularly with closure devices, sinus venosus ASD cannot be treated endovascularly due to the lack of rims for the device to attach to.
Reference: Vyas HV, Greenberg SB, Krishnamurthy R. MR imaging and CT evaluation of congenital pulmonary vein abnormalities in neonates and infants. Radiographics 2012;32(1):87-98. doi: 10.1148/rg.321105764. PubMed PMID: 22236895.
3a This was an incidental finding on a gated CTA of an asymptomatic patient. What is the best next step?
|
A. Surgical closure.
B. Catheter-based closure.
C. Leave it alone.
View Answer
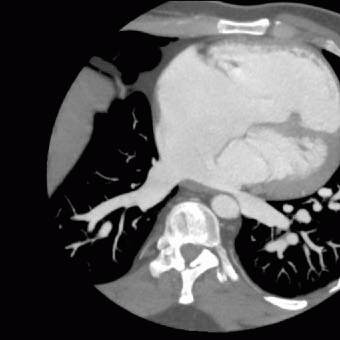
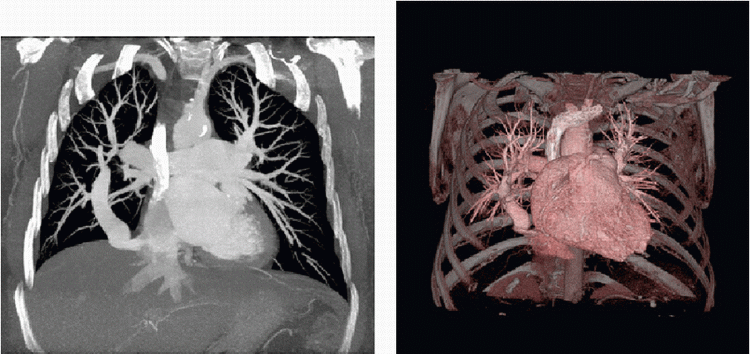
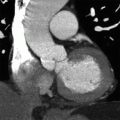
3a Answer C. Images demonstrate unroofed coronary sinus (note the connection between the left and right atrium and the coronary sinus). In this case, the shunt appears small without evidence of left heart enlargement. Given the small shunt, no treatment is required. Surgical treatment would be considered if there is a significant shunt (Qp/Qs > 2). There is no role for catheter-based closure in unroofed coronary sinus.
3b Unroofed coronary sinus is associated with which of the following vascular abnormalities?
A. Azygos continuation of the IVC
B. Coarctation of the aorta
C. Anomalous right pulmonary venous return
D. Left-sided SVC
View Answer
3b Answer D. Unroofed coronary sinus is associated with left-sided SVC. Azygous continuation of the IVC is associated with polysplenia and many other congenital heart diseases. Coarctation is classically associated with bicuspid aortic valve. Anomalous right pulmonary venous return can be associated with sinus venosus atrial septal defects.
Reference: Shah SS, Teague SD, Lu JC, et al. Imaging of the coronary sinus: normal anatomy and congenital abnormalities. Radiographics 2012;32(4):991-1008. doi: 10.1148/rg.324105220. PubMed PMID: 22786990.
4 How many types of atrial septal defects (ASD) are there?
A. There are two types of ASD.
B. There are three types of ASD.
C. There are four types of ASD.
D. There are five types of ASD.
View Answer
4 Answer C. There are 4 types of ASD: sinus venosus, ostium secundum, ostium primum, and unroofed coronary sinus.
Reference: Rojas CA, El-Sherief A, Medina HM, et al. Embryology and developmental defects of the interatrial septum. AJR Am J Roentgenol 2010;195(5):1100-1104. doi: 10.2214/AJR.10.4277. Review. PubMed PMID: 20966313.
5 What is a major difference between membranous versus muscular ventricular septal defects (VSD)?
A. Muscular VSD can undergo spontaneous closure.
B. Membranous VSD can undergo spontaneous closure.
C. Endocarditis prophylaxis is not required for muscular VSD.
D. Endocarditis prophylaxis is not required for membranous VSD.
View Answer
5 Answer A. Muscular VSD can undergo spontaneous closure while membranous VSD will not close spontaneously. Endocarditis prophylaxis is necessary for both muscular and membranous VSDs.
Reference: Minette MS, Sahn DJ. Ventricular septal defects. Circulation 2006;114(20):2190-2197. Review. Erratum in: Circulation 2007;115(7):e205.
A. Biopsy
B. CT of the chest without contrast
C. CTA of the chest
D. VQ scan
E. No further imaging necessary
View Answer
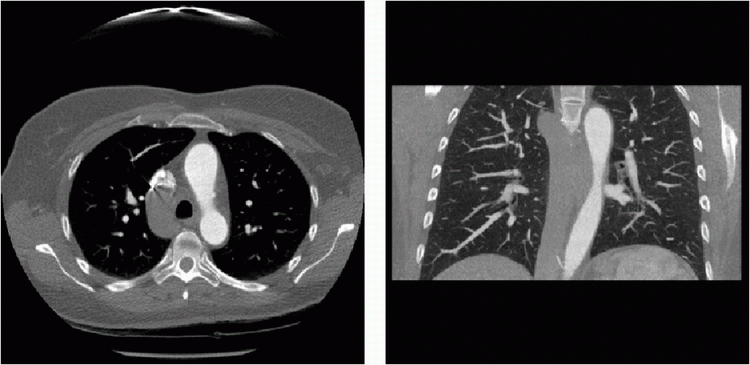
6a Answer C. PA and lateral chest radiographs show an abnormal vertical linear opacity along the right lower lung. On the lateral view, it appears to course inferiorly toward the IVC region. This is consistent with the “scimitar sign,” which is suggestive of anomalous pulmonary venous return (scimitar vein). The differential also includes anomalous single pulmonary vein, which would drain normally into the left atrium. These conditions have different treatments (surgical for scimitar, no treatment for anomalous single pulmonary vein). The best next step would be to define the anatomy with a CTA chest. Biopsy would not be helpful and may even be dangerous. CT without IV contrast would not define the vascular anatomy well. VQ scan would not clarify what the tubular structure is. No further imaging would also not be helpful given we need to further define the abnormality.
References: Ferguson EC, Krishnamurthy R, Oldham SA. Classic imaging signs of congenital cardiovascular abnormalities. Radiographics 2007;27(5):1323-1334. Review. PubMed PMID: 17848694.
Nazarian J, Kanne JP, Rajiah P. Scimitar sign. J Thorac Imaging 2013;28(4):W61.
A. Left to right
B. Right to left
C. No shunt
View Answer
6b Answer A. A scimitar vein is draining into the IVC. This is a type of anomalous pulmonary venous return and a left to right shunt (remember that the pulmonary veins carry oxygenated blood so it is part of the left circulation).
In classic scimitar syndrome, there is anomalous right pulmonary vein, hypoplasia of the right lung along with pulmonary artery hypoplasia, dextrocardia, and systemic arterial supply to the lungs. These features are not always present on all patients. Atrial septal defect (ASD) is not part of the syndrome but can sometimes occur concurrently. If patient is symptomatic due to significant shunting, surgical correction to redirect the vein into the left atrium can be performed.
References: Ferguson EC, Krishnamurthy R, Oldham SA. Classic imaging signs of congenital cardiovascular abnormalities. Radiographics 2007;27(5):1323-1334. Review. PubMed PMID: 17848694.
Nazarian J, Kanne JP, Rajiah P. Scimitar sign. J Thorac Imaging 2013;28(4):W61.
A. Muscular ventricular septal defect without Eisenmenger syndrome
B. Muscular ventricular septal defect with Eisenmenger syndrome
C. Membranous ventricular septal defect without Eisenmenger syndrome
D. Membranous ventricular septal defect with Eisenmenger syndrome
View Answer
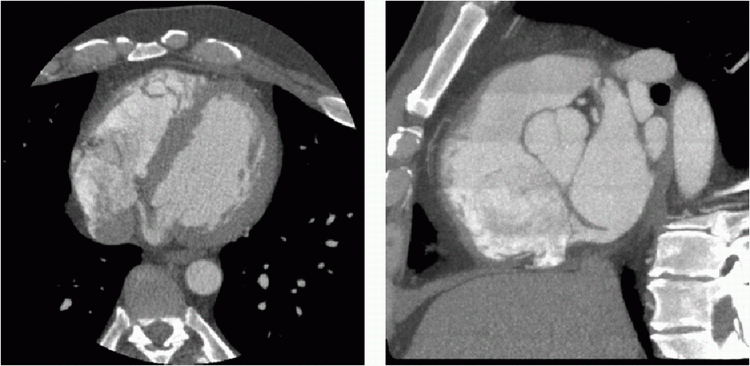
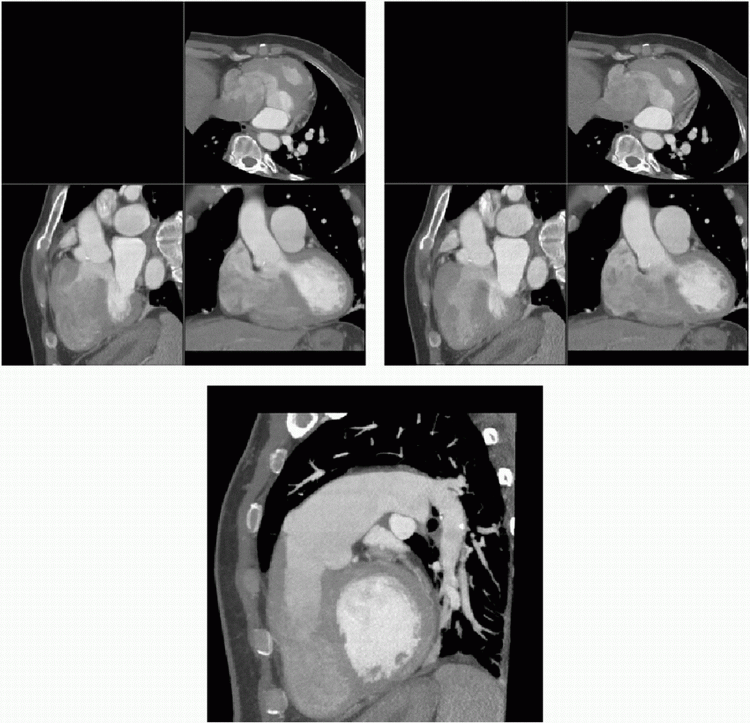
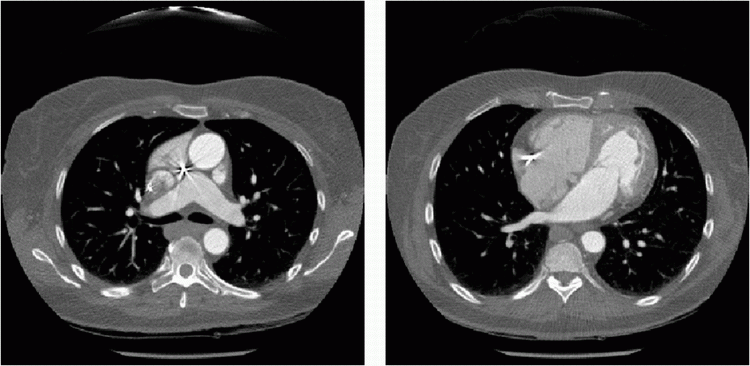
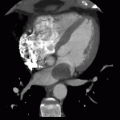
7 Answer D. Images show a membranous VSD with evidence of both left to right and right to left shunting (note the mixing of the contrast material at the site of ventricular septal defect). This is consistent with Eisenmenger syndrome with suprasystemic right heart pressures causing right to left shunting. Note the marked right ventricular hypertrophy from the pulmonary hypertension due to long-standing shunt. Muscular ventricular septal defects are located along the muscular septum, which is not shown here.
Reference: Peña E, Dennie C, Veinot J, et al. Pulmonary hypertension: how the radiologist can help. Radiographics 2012;32(1):9-32. doi: 10.1148/rg.321105232. PubMed PMID: 22236891.
A. Left atrium
B. Aorta
C. Pulmonary vein
D. Left ventricle
View Answer
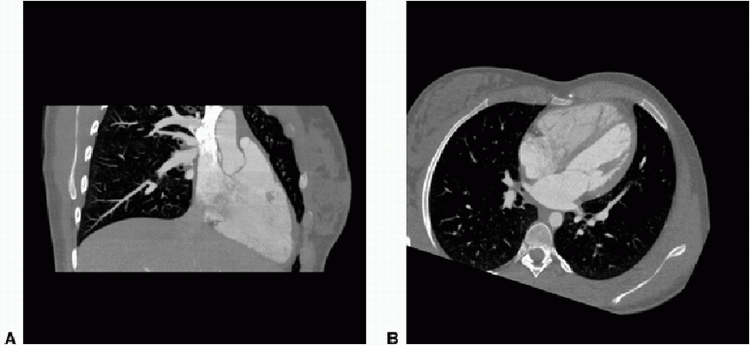
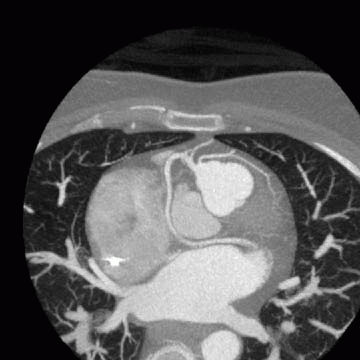
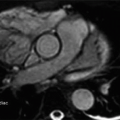
8a Answer C. Image A shows anomalous pulmonary venous return with right superior pulmonary vein (RSPV) returning to SVC. Note the right heart appears enlarged (Image B). Left atrium and ventricle appear normal. Visualized ascending aorta also appears normal.
Reference: Kafka H, Mohiaddin RH. Cardiac MRI and pulmonary MR angiography of sinus venosus defect and partial anomalous pulmonary venous connection in cause of right undiagnosed ventricular enlargement. AJR Am J Roentgenol 2009;192(1):259-266. doi: 10.2214/AJR.07.3430. PubMed PMID: 19098208.
8b A cardiac catheterization was subsequently performed. The Qp/Qs was determined to be 2.1. The Patient became symptomatic and developed atrial fibrillation. What is the best treatment?
A. Stent
B. Surgical repair
C. Medical treatment
D. Device closure
View Answer
8b Answer B. The images show anomalous pulmonary venous return with the right superior pulmonary vein (RSPV) entering to the SVC. There is significant shunting as evidenced by Qp/Qs of 2.1 and right heart enlargement. In addition, the presence of atrial fibrillation suggests significant volume overloading and chamber remodeling. The best treatment therefore is surgery. Note there is an association between right partial anomalous pulmonary venous return and sinus venosus atrial septal defects. Device closure is not feasible since the anomalous vein needs to be redirected to the left atrium. Medical treatment is not advisable given the significant shunting (Qp/Qs > 1.5) and development of atrial fibrillation. Stenting would not fix this problem.
References: Dillman JR, Yarram SG, Hernandez RJ. Imaging of pulmonary venous developmental anomalies. AJR Am J Roentgenol 2009;192(5):1272-1285. doi: 10.2214/AJR.08.1526. Review. PubMed PMID: 19380552.
Kafka H, Mohiaddin RH. Cardiac MRI and pulmonary MR angiography of sinus venosus defect and partial anomalous pulmonary venous connection in cause of right undiagnosed ventricular enlargement. AJR Am J Roentgenol 2009;192(1):259-266. doi: 10.2214/AJR.07.3430. PubMed PMID: 19098208.
A. Aorta
B. Main pulmonary trunk
C. Left atrium
D. No abnormality
View Answer
9a Answer B. Frontal CXR shows an enlarged pulmonary trunk. The left mediastinal contour is composed of, starting superiorly, the left subclavian artery, left arch, main pulmonary trunk, left atrial appendage (if enlarged), and left ventricle. In this case, the contour below the arch is enlarged suggesting enlarged pulmonary trunk. Aortic enlargement can occur throughout its course so can involve the ascending aorta, arch, or descending aorta. Left atrial enlargement can be seen with enlarged left atrial appendage contour, or in extreme left atrial enlargement, a double contour is seen along the right heart border (double density sign). There can also be splaying of the carina.
Reference: Ferguson EC, Krishnamurthy R, Oldham SA. Classic imaging signs of congenital cardiovascular abnormalities. Radiographics 2007;27(5):1323-1334. Review. PubMed PMID: 17848694.
A. Left-to-left shunt
B. Right-to-left shunt
C. Left-to-right shunt
D. Right-to-right shunt
E. Mixed shunt
View Answer
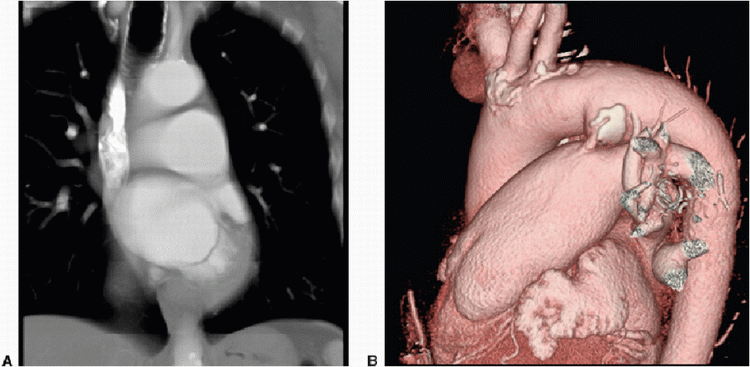
9b Answer C. Coronal reformat shows enlarged PA contour (Image A). 3D volume rendered images show a PDA (image B). Patent ductus arteriosus is a type of left to right shunt. However, it does not involve the right heart since the connection is between the aorta and pulmonary artery (so the right heart will not be enlarged). It is associated with rubella infection during pregnancy. It can lead to Eisenmenger syndrome in long-standing shunts.
References: Goitein O, Fuhrman CR, Lacomis JM. Incidental finding on MDCT of patent ductus arteriosus: use of CT and MRI to assess clinical importance. AJR Am J Roentgenol 2005;184(6):1924-1931. PubMed PMID: 15908555.
Morgan-Hughes GJ, Marshall AJ, Roobottom C. Morphologic assessment of patent ductus arteriosus in adults using retrospectively ECG-gated multidetector CT. AJR Am J Roentgenol 2003;181(3): 749-754. PubMed PMID: 12933475.
Schneider DJ, Moore JW. Patent ductus arteriosus. Circulation 2006;114(17):1873-1882.
A. Aortic stent is in place.
B. Pulmonary artery stent is in place.
C. Pulmonary vein stent is in place.
D. Left SVC stent is in place.
View Answer
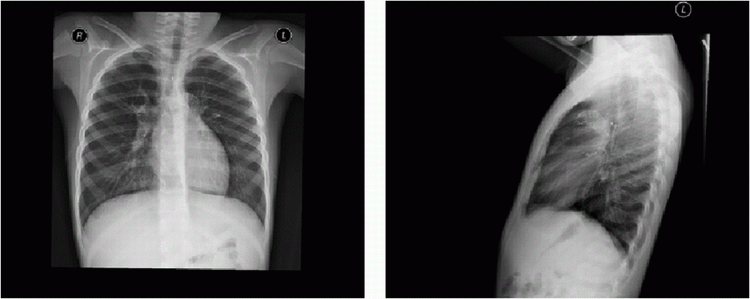
10a Answer B. Frontal and lateral chest radiographs show a narrowed mediastinum with a left pulmonary artery stent. The stent is positioned anteriorly on the lateral view. Coarctation stents would be more superior and posterior in location along the course of the aorta. Pulmonary vein stents would be near the left atrium at a inferior and posterior position. Left SVC stent would be vertical in nature.
A. Arterial switch
B. Ross procedure
C. Mustard baffle
D. Fontan procedure
View Answer
10b Answer A. The pulmonary artery draping over the aorta is a pathognomonic appearance of an arterial switch used to correct underlying dextrotransposition of the great arteries (d-TGA). In this case, the patient had the arterial switch with subsequent left pulmonary stenosis. This was treated with a stent.
In a Ross procedure, the native pulmonary valve is switched to the aortic position and a prosthetic pulmonic valve is put in place. Mustard baffle is used to treat dextrotransposition of the great arteries; the systemic and pulmonary venous returns are redirected via baffles to correct for the great vessel switch. In the Fontan procedure, the systemic venous return is connected into the pulmonary arteries directly, bypassing the heart; this is typically used in patients with single ventricular physiology.
Reference: Spevak PJ, Johnson PT, Fishman EK. Surgically corrected congenital heart disease: utility of 64-MDCT. AJR Am J Roentgenol 2008;191(3):854-861. doi: 10.2214/AJR.07.2889. Review. PubMed PMID: 18716119.
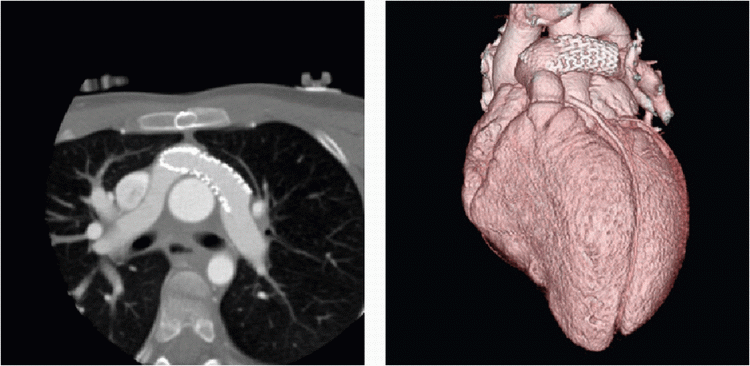
11a A 56-year-old female presents with shortness of breath. What is commonly associated with this condition?
|
A. Polysplenia
B. Asplenia
C. Bicuspid aortic valve
D. Unicuspid aortic valve
View Answer
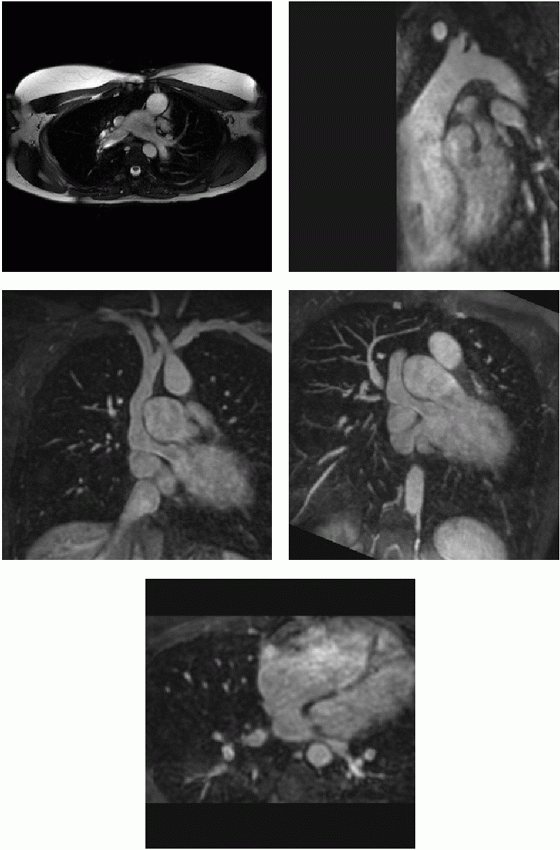
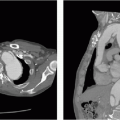
11a Answer A. The images show enlarged azygos vein seen in interrupted IVC with azygos continuation. This condition is associated with polysplenia. Bicuspid aortic valve is associated with coarctation but also aortic aneurysm from bicuspid aortopathy. Unicuspid aortic valve is associated with aortic stenosis.
Reference: Applegate KE, Goske MJ, Pierce G, et al. Situs revisited: imaging of the heterotaxy syndrome. Radiographics 1999;19(4):837-852; discussion 853-854. Review. PubMed PMID: 10464794.
A. Dextrotransposition of the great arteries (D-TGA)
B. Levotransposition of the great arteries (L-TGA)
C. Truncus arteriosus
D. Normal anatomy
View Answer
11b Answer B. The Images show transposition of the vessels with the aorta arising anterior to the pulmonary artery. This is a levo-type of transposition of the great arteries (l-TGA) with ventricular inversion (morphologic RV on the left side, morphologic LV on the right side). With the ventricles switched in position, there is a transposition of the great arteries. However, the flow circuit is normal with the systemic blood going into the pulmonary artery and oxygenated pulmonary venous blood to the aorta. The systemic ventricle on the left is a morphologic right ventricle containing the tricuspid valve. This can cause problems later as the morphologic RV can fail and the tricuspid valve can be leaky. There is also a higher rate of arrhythmia from the systemic RV. As a result, these patients can sometimes present at a young age with already an ICD and valvular replacement.
Reference: Cohen MD, Johnson T, Ramrakhiani S. MRI of surgical repair of transposition of the great vessels. AJR Am J Roentgenol 2010;194(1):250-260. doi: 10.2214/AJR.09.3045. Review. PubMed PMID: 20028930.
A. Surgical correction
B. No treatment
C. No contact sports
D. ICD placement
View Answer
11c Answer B. A retroaortic left circumflex artery is seen. This is a benign coronary anomaly and no surgery is necessary. There is no need for activity restriction or ICD placement.
References: Kim SY, Seo JB, Do KH, et al. Coronary artery anomalies: classification and ECG-gated multi-detector row CT findings with angiographic correlation. Radiographics 2006;26(2):317-333; discussion 333-334. Review. PubMed PMID: 16549600.
Shriki JE, Shinbane JS, Rashid MA, et al. Identifying, characterizing, and classifying congenital anomalies of the coronary arteries. Radiographics. 2012;32(2):453-468. doi: 10.1148/rg.322115097. Review. PubMed PMID: 22411942.
A. Tetralogy of Fallot repair
B. Mustard/Senning procedure
C. Jatene arterial switch
D. Rastelli procedure
View Answer




12 Answer B. There is d-TGA with Mustard/Senning baffle. The great vessels are switched so the procedure switches the inflow to redirect systemic blood to the left ventricle and the pulmonary venous return to the right atrium. Tetralogy repair involves closing the VSD and alleviating the right ventricular outflow tract obstruction. Arterial switch typically show a characteristic draping of the pulmonary artery over the aorta. Rastelli procedure would involve a right ventricular outflow conduit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree