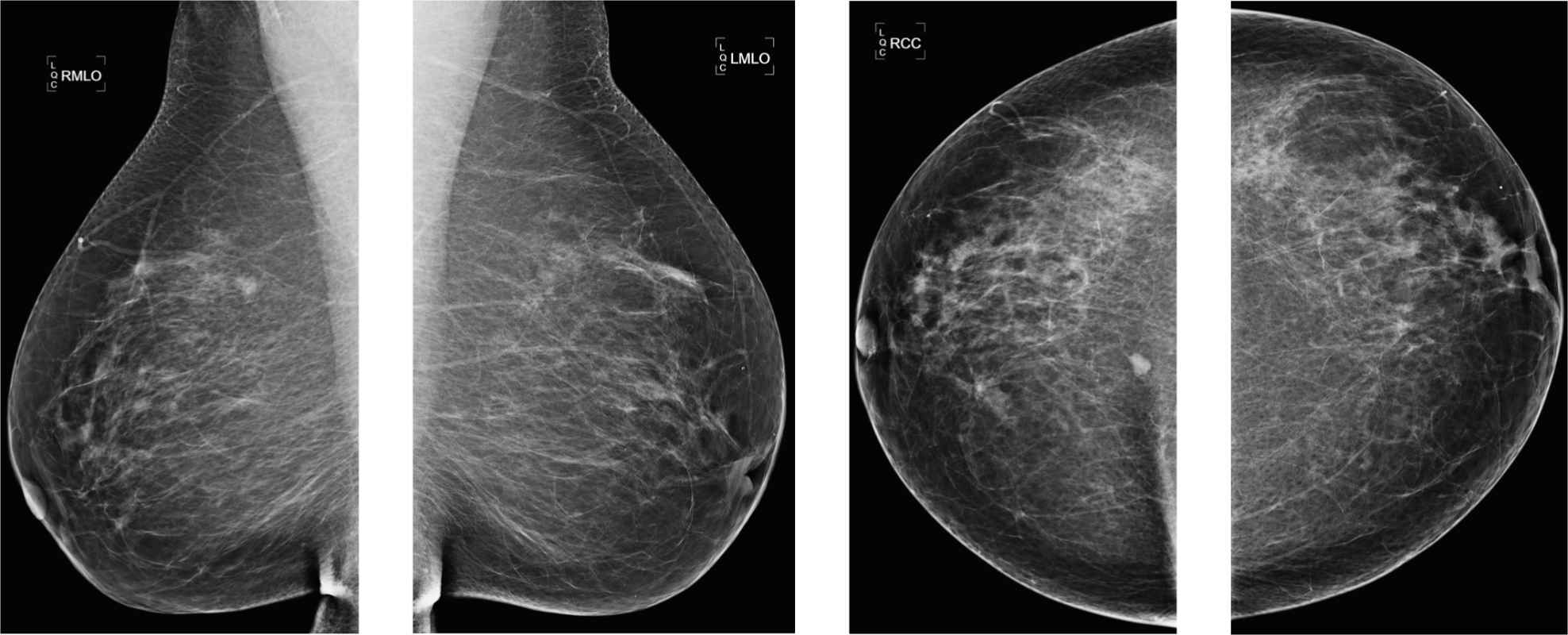
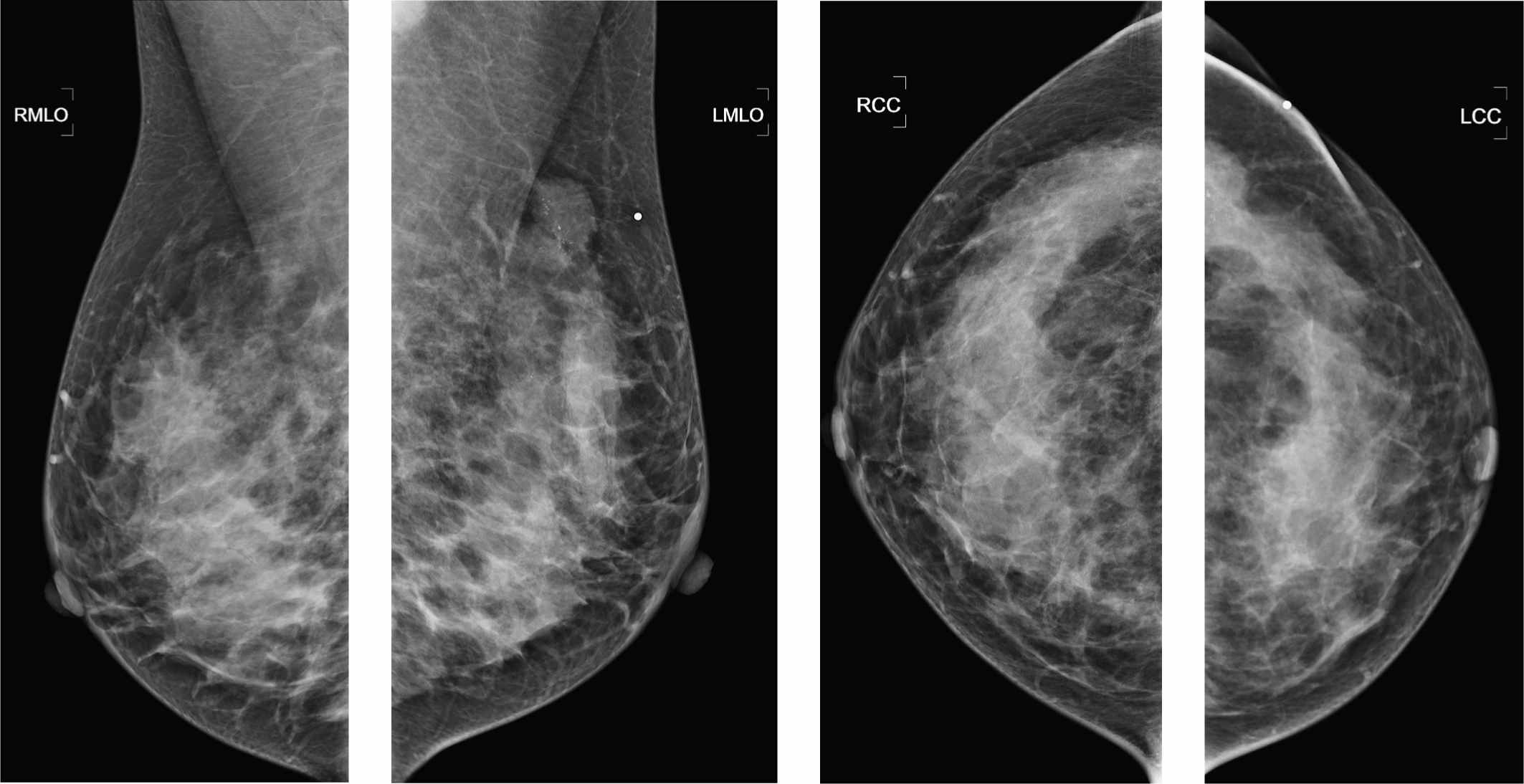
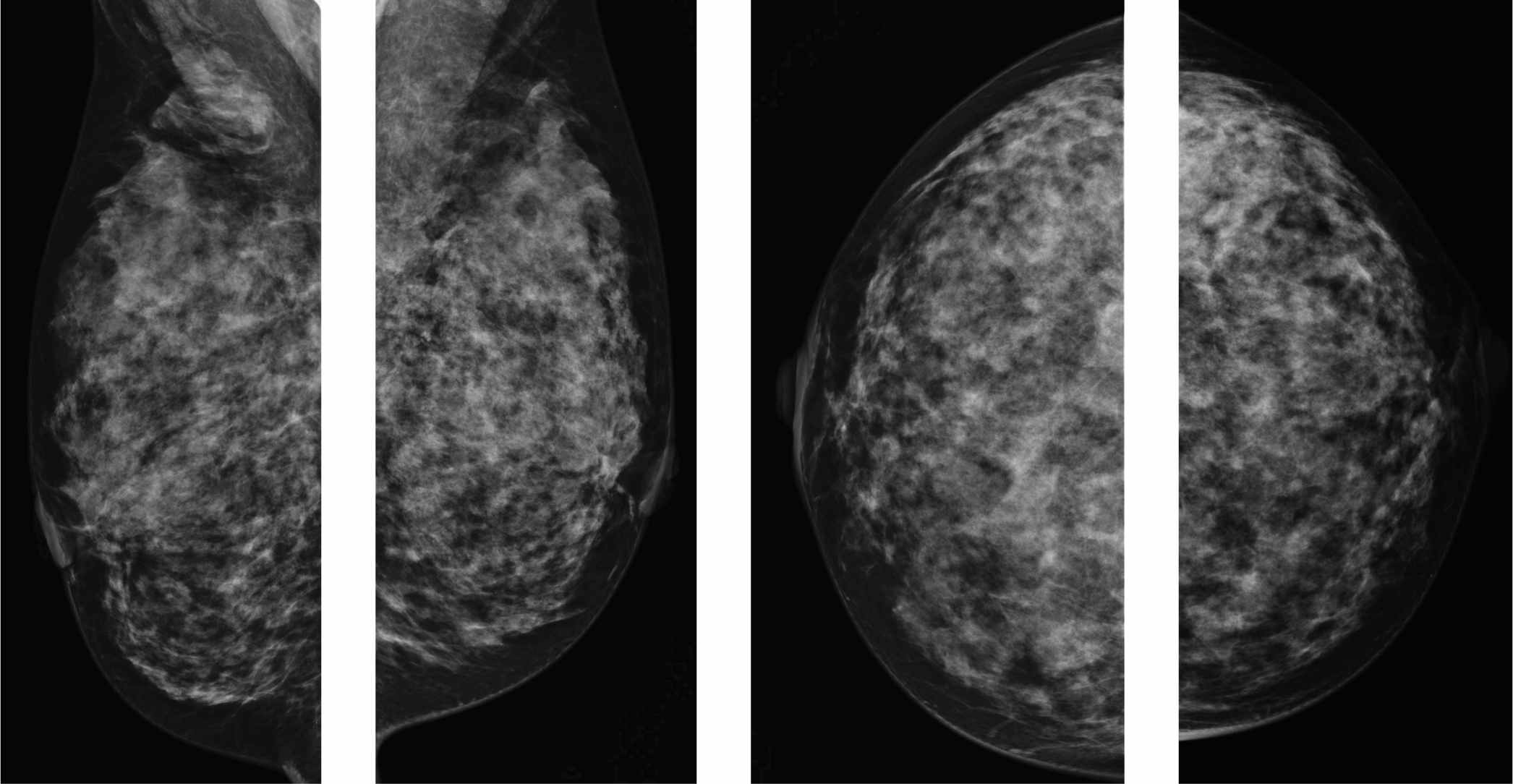
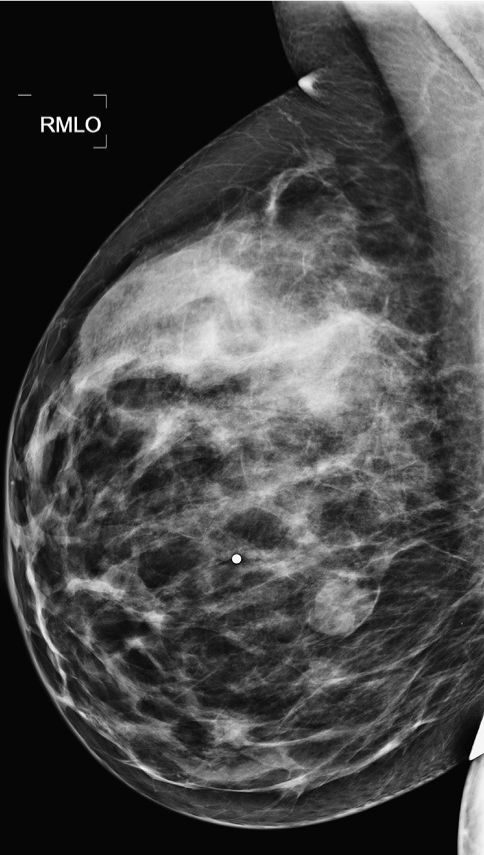
1. What BI-RADS classification should be used here?
2. What are the possible diagnostic imaging exams to work up this finding?
3. What type of biopsy would you recommend?
4. When you see microcalcification developing in a surgical scar, what is your differential?
5. What are the complications of breast reduction or reconstruction you should be looking for on surveillance?
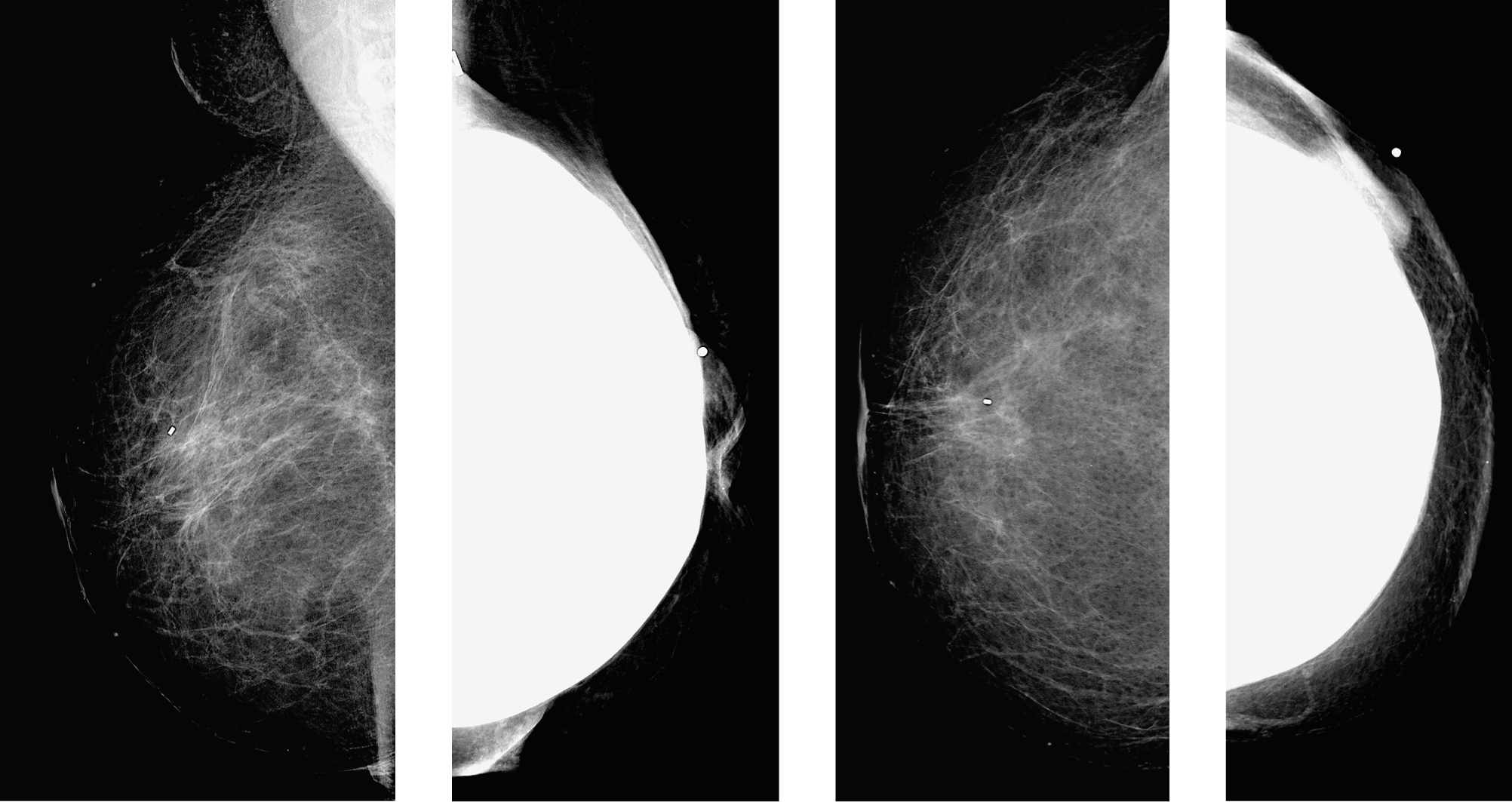
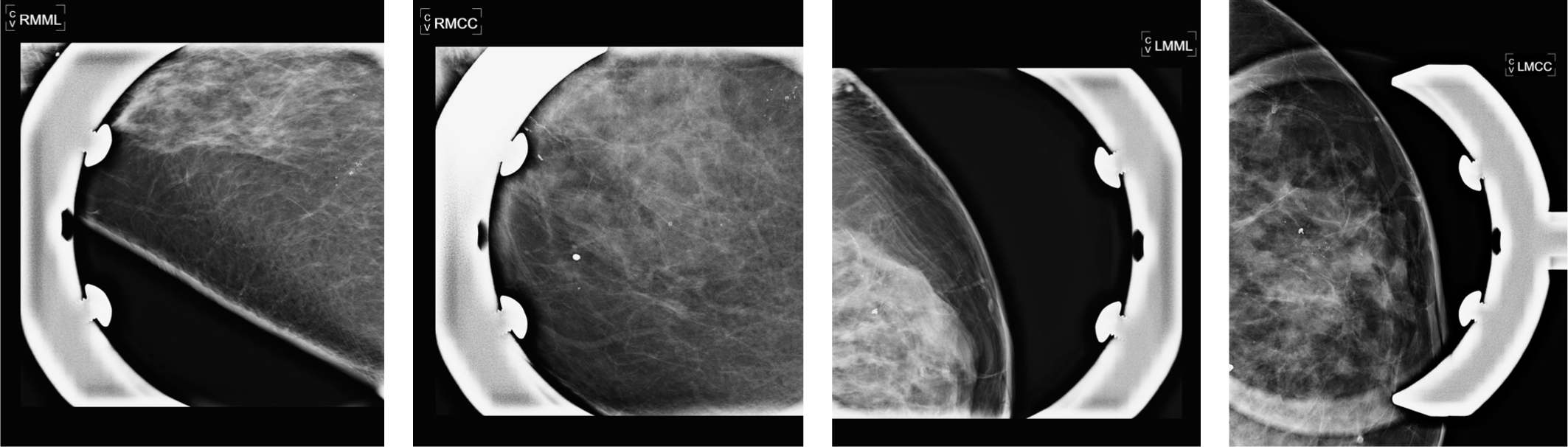
Transverse rectus abdominis myocutaneous flap (TRAM) reconstruction complications 1865
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
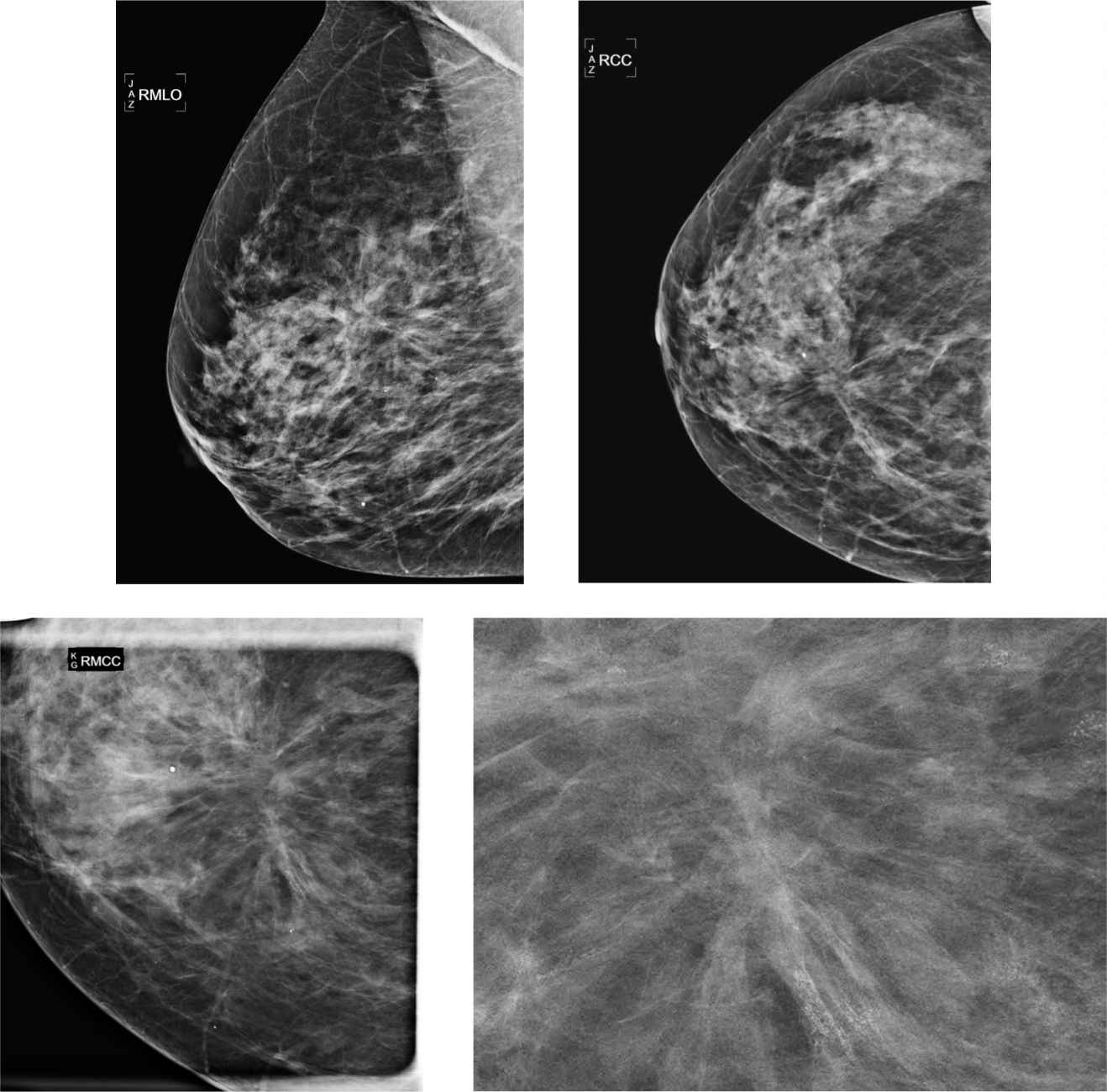
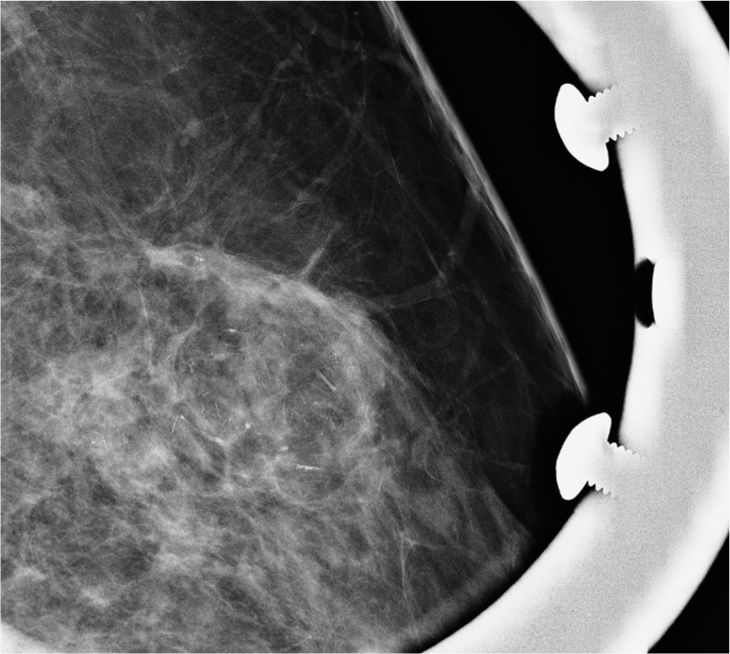
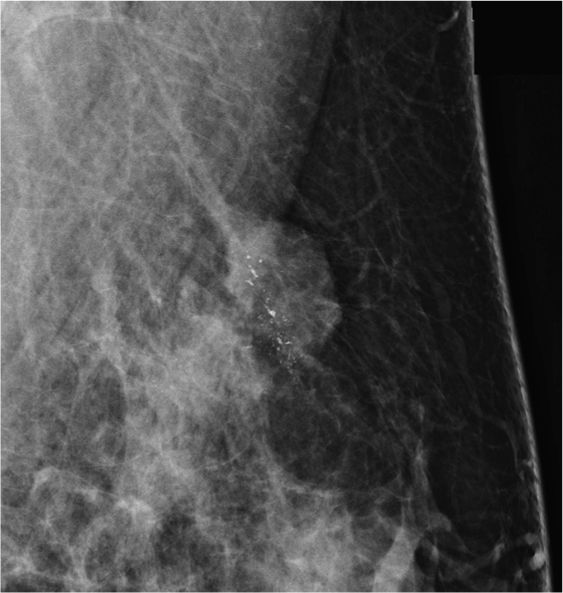
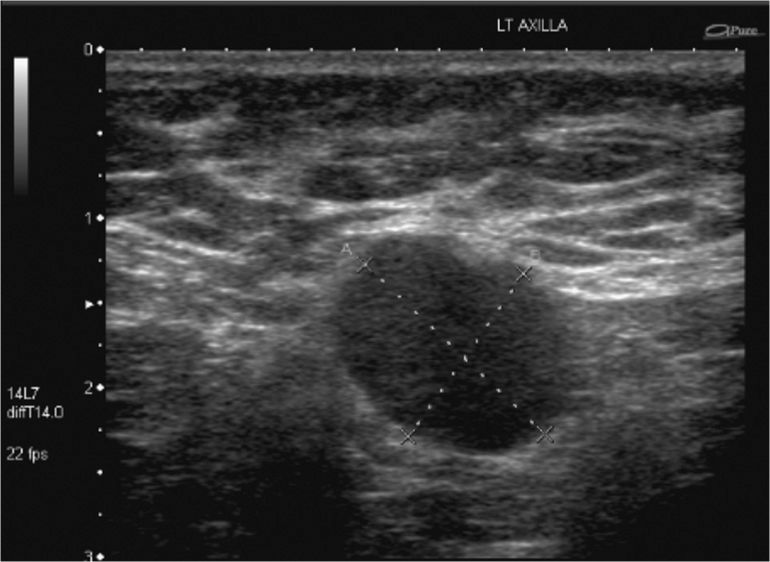
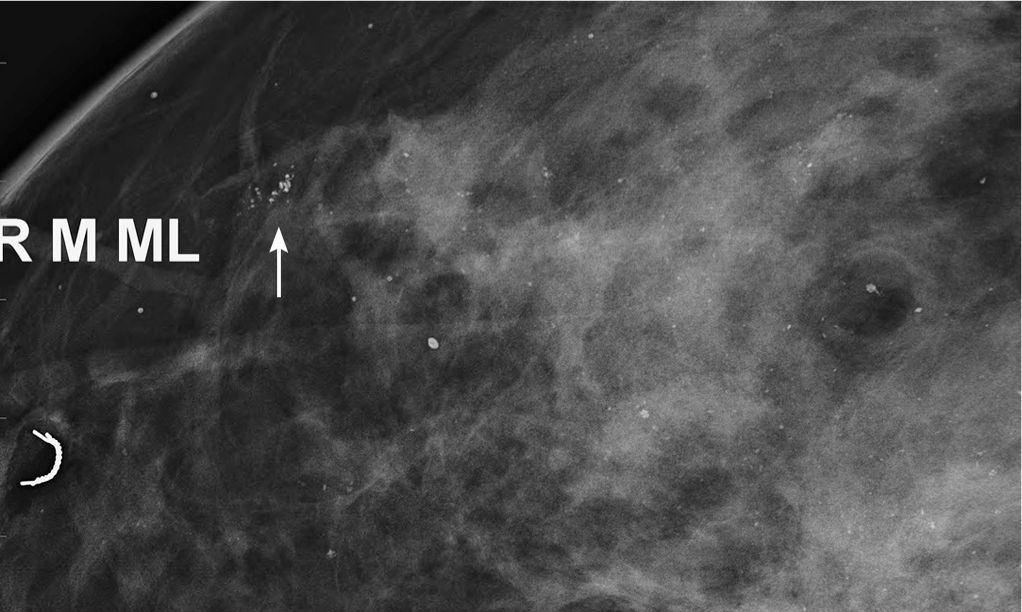
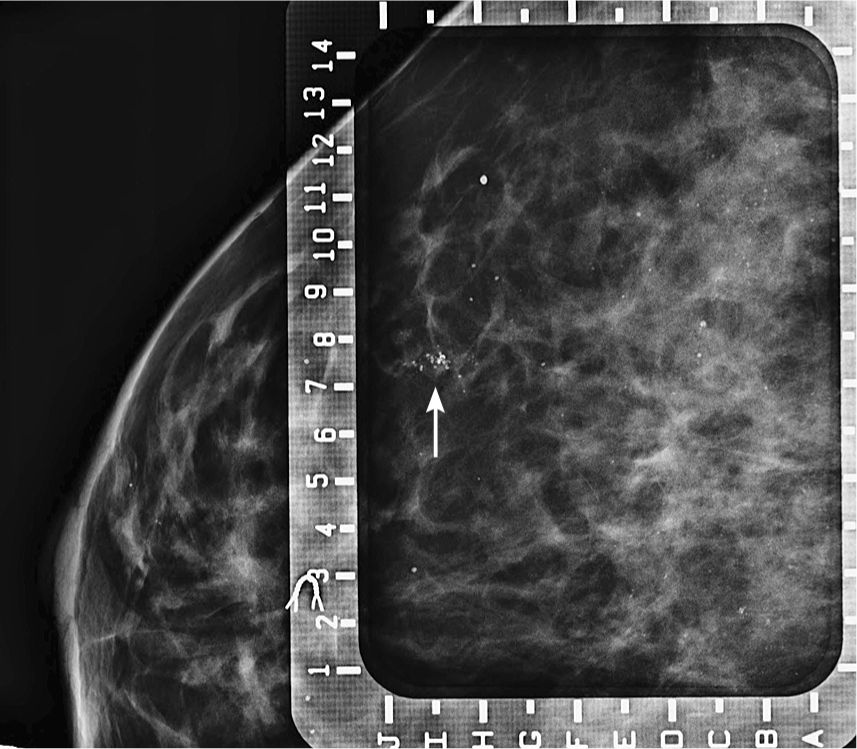
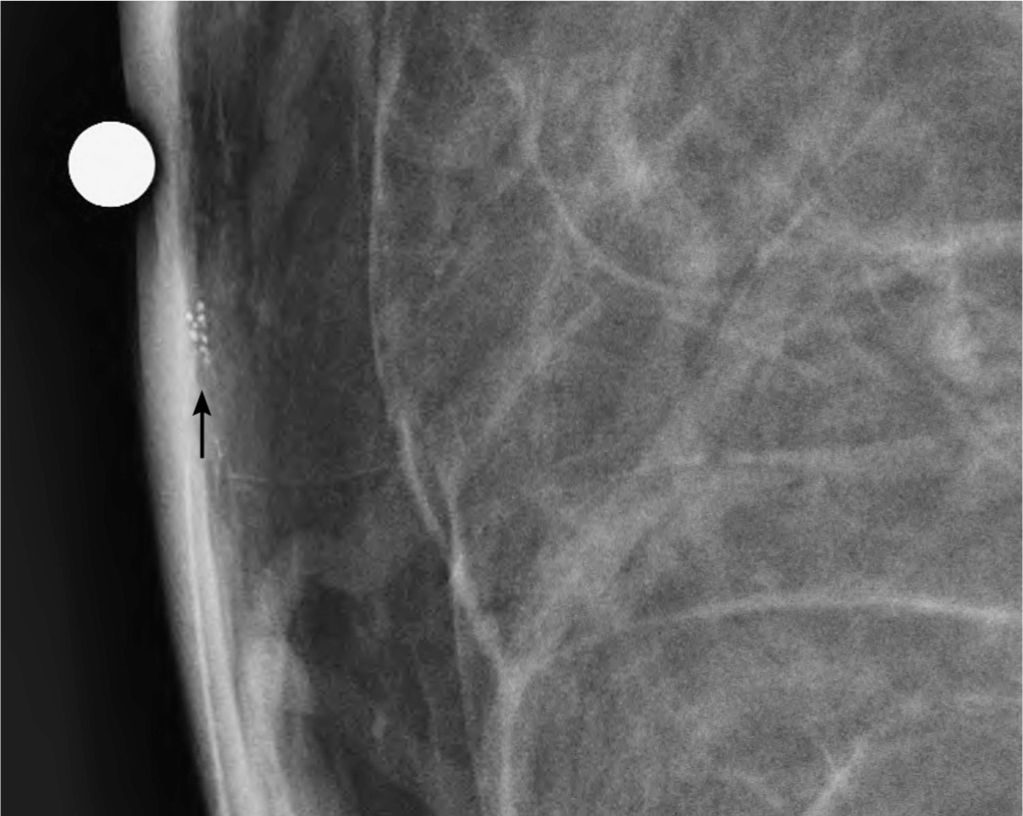
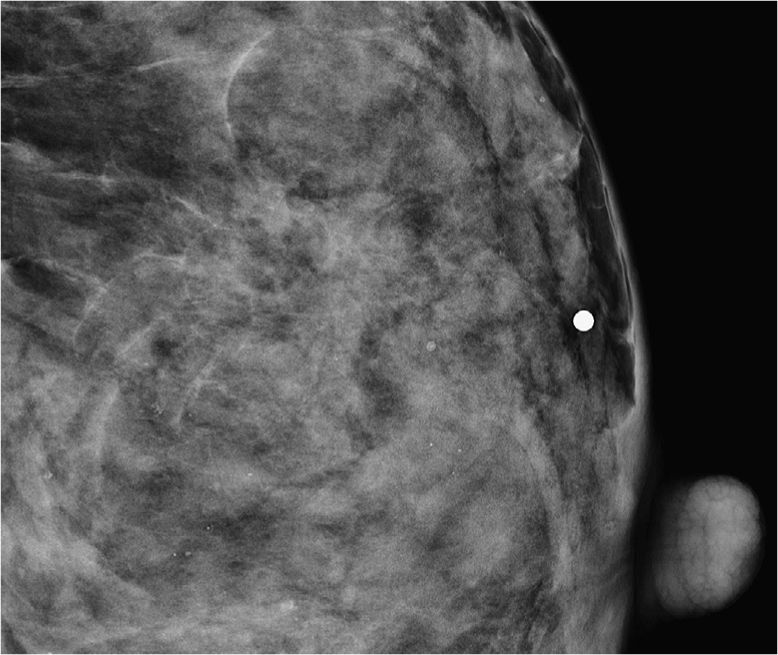
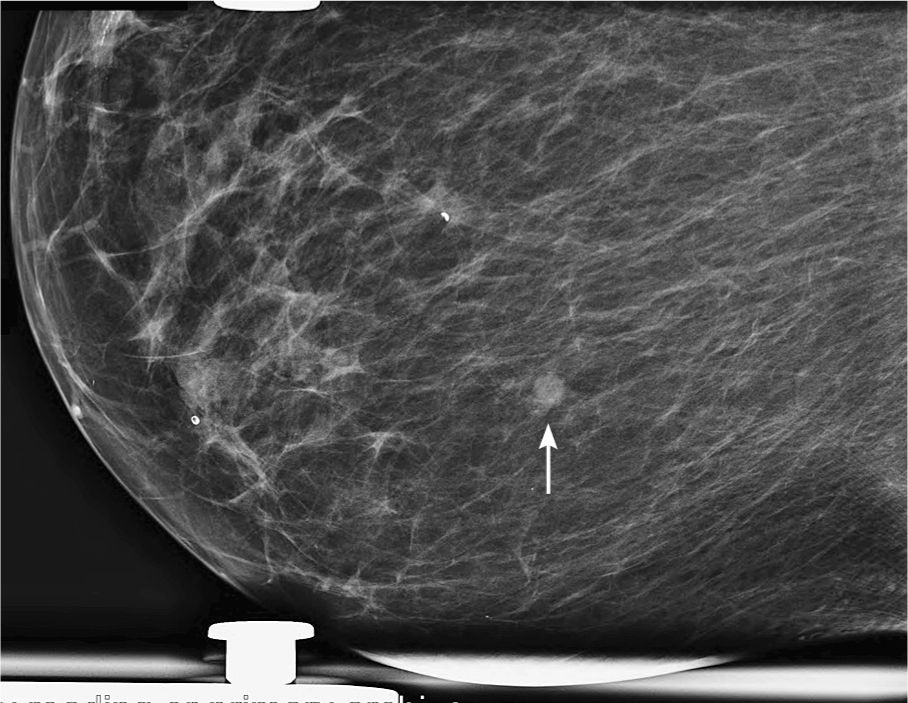
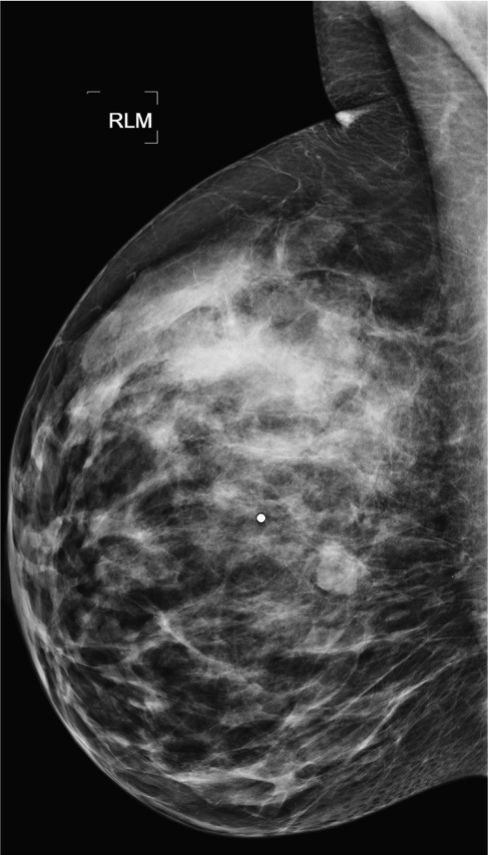
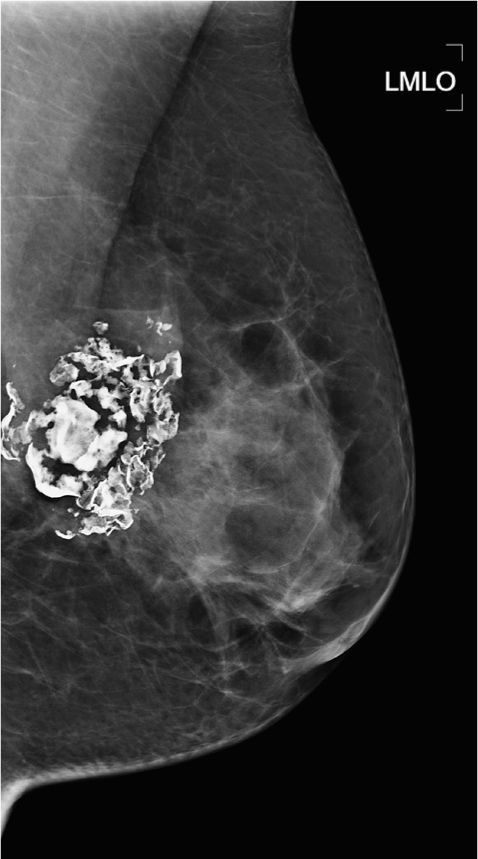
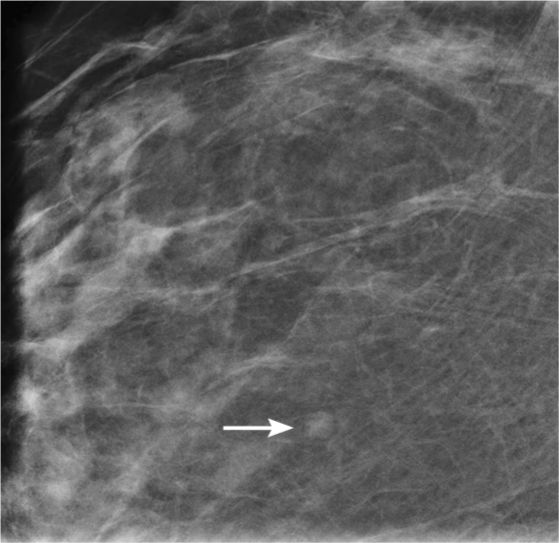
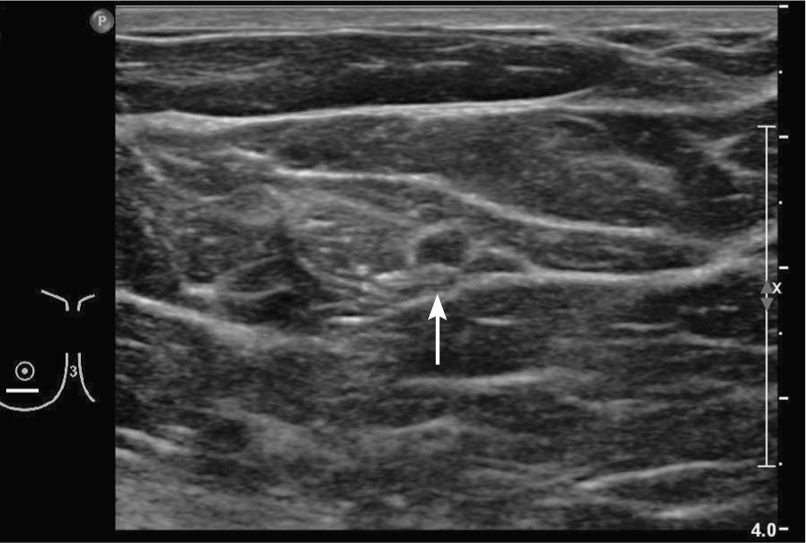
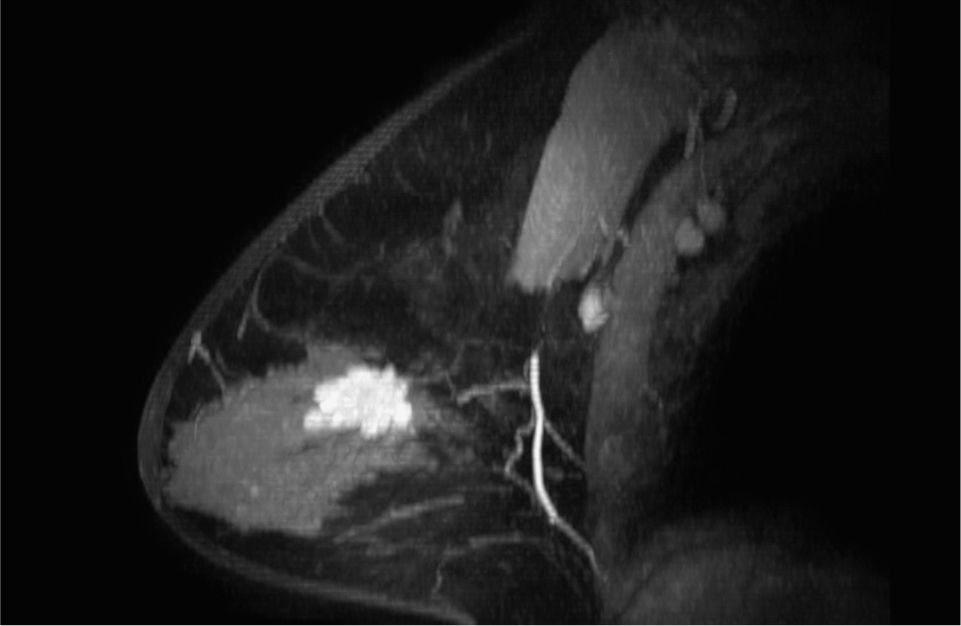
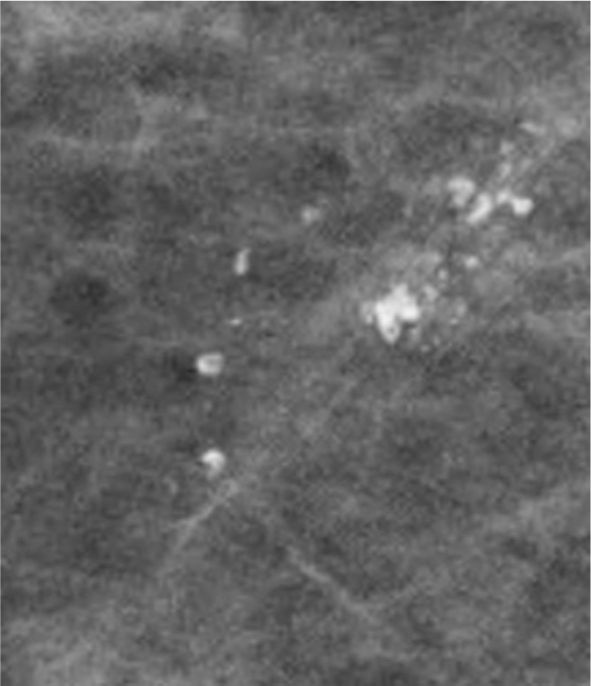
Close-up fat necrosis in TRAM reconstruction. Note that the calcifications make up a peripheral component to the mass.

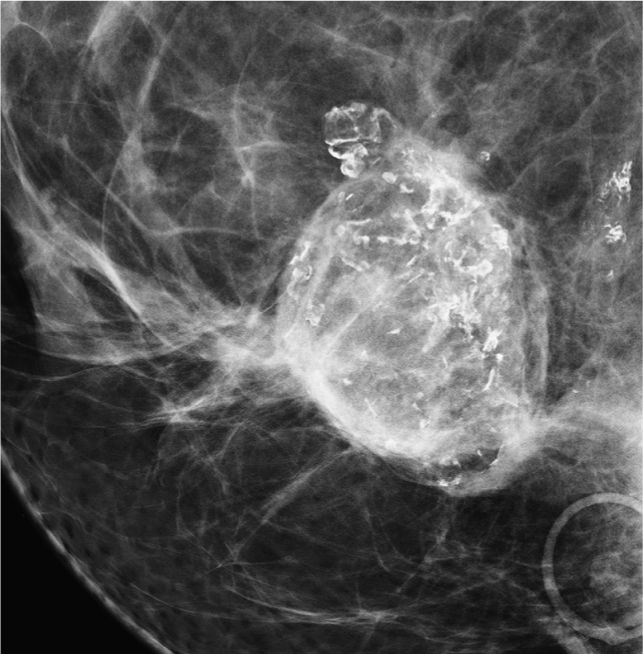
Close-up local recurrence in TRAM reconstruction.
Answers
1. BI-RADS 2 should be used, as this is a characteristically benign finding. BI-RADS 0 is not appropriate. If the patient was having a “tramogram,” then it would be a diagnostic exam in the first place. Early fat necrosis can sometimes look suspicious, and therefore if this was one of those cases, a BI-RADS 4 may potentially be more appropriate.
2. All of the answers can be correct. If you have prior films and they are stable, no action need be taken. First visit, you may wish to work up with either spot (magnification) views or ultrasound. Ultrasound itself can appear suspicious when fat necrosis calcifies; therefore, it may not be a good exam in this instance. For reconstructed breasts, MRI is a good tool for surveillance. Tomosynthesis can be used in place of diagnostic special views.
3. This is a characteristic benign finding; therefore, no action other than follow-up is recommended.
4. Depends on what the lumpectomy was performed for. If there was ductal carcinoma in situ (DCIS) present in the surgical excision, then DCIS recurrence is always at the top of the list. “Dead DCIS” is said to be a recognized phenomenon in patients with lower-grade DCIS, who have undergone radiation therapy. Dystrophic calcifications commonly occur related to the development of fat necrosis. Dermal calcifications are usually seen only in the skin, but if there is marked posttreatment distortion, they may be projected over the surgical scar.
5. All of the answers can be true and can present as findings. However, in general practice, the common things you encounter are developing areas of fat necrosis that may be visible on both mammography and ultrasound. If they have had a breast reduction, they tend to have a characteristic pattern of parenchymal change with swirly lines, sometimes best seen on the CC and sometimes in the lower half on the MLO. Decreased breast volume related to lobular cancer is for global change over a time period, rather than just to the reduction surgery.
Suggested Reading
Eidelman Y, Liebling RW, Buchbinder S, Strauch B, Goldstein RD. Mammography in the evaluation of masses in breasts reconstructed with TRAM flaps. Ann Plast Surg. 1998;41(3):229-233.
History of prior benign excisional biopsy for biopsy-proven ADH
1. What are the pertinent findings on mammography?
2. What could be the etiology?
3. Which malignancy typically presents with distortion like this?
4. Are there any additional findings on the magnification view?
5. What is the consequence?
Distortion from prior excisional biopsy as a result of prior biopsy of ADH and now recurrent calcifications 1308
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
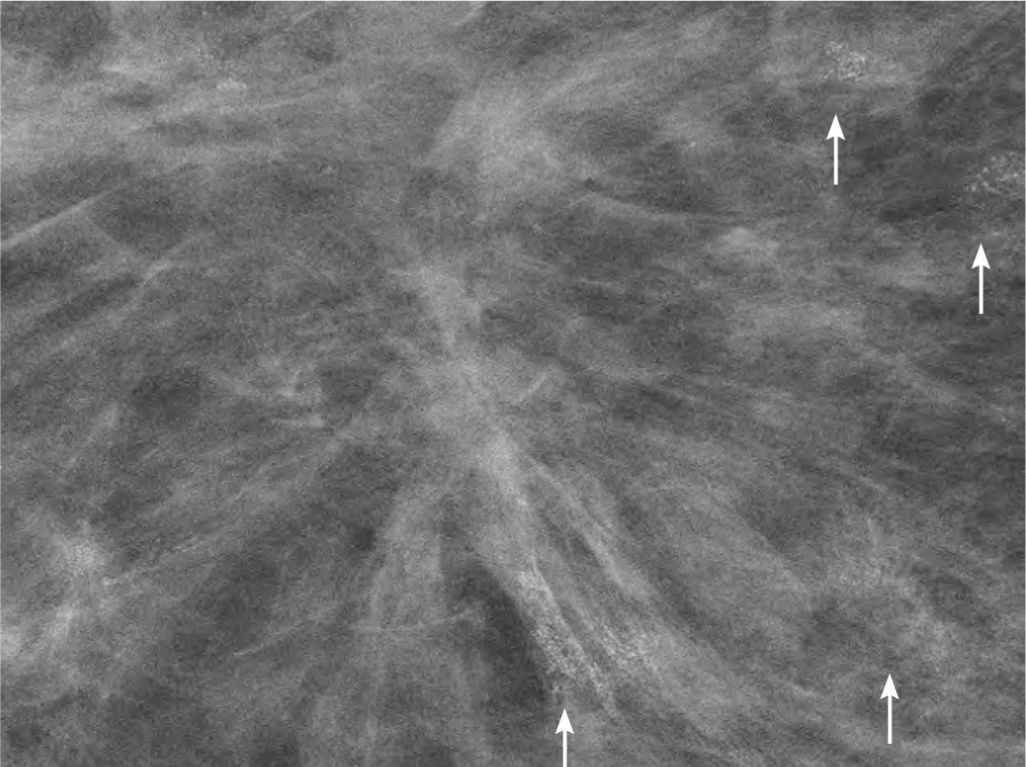
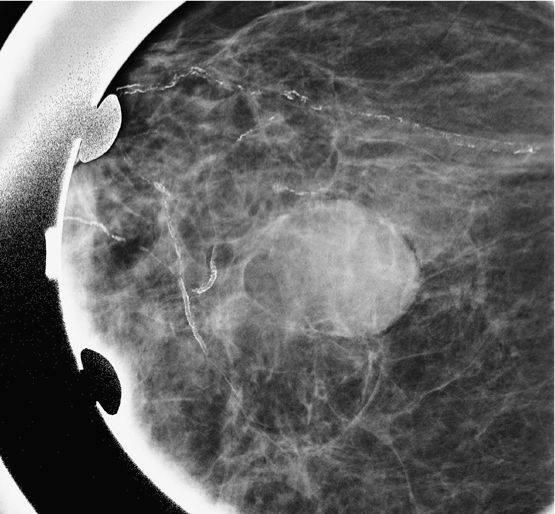
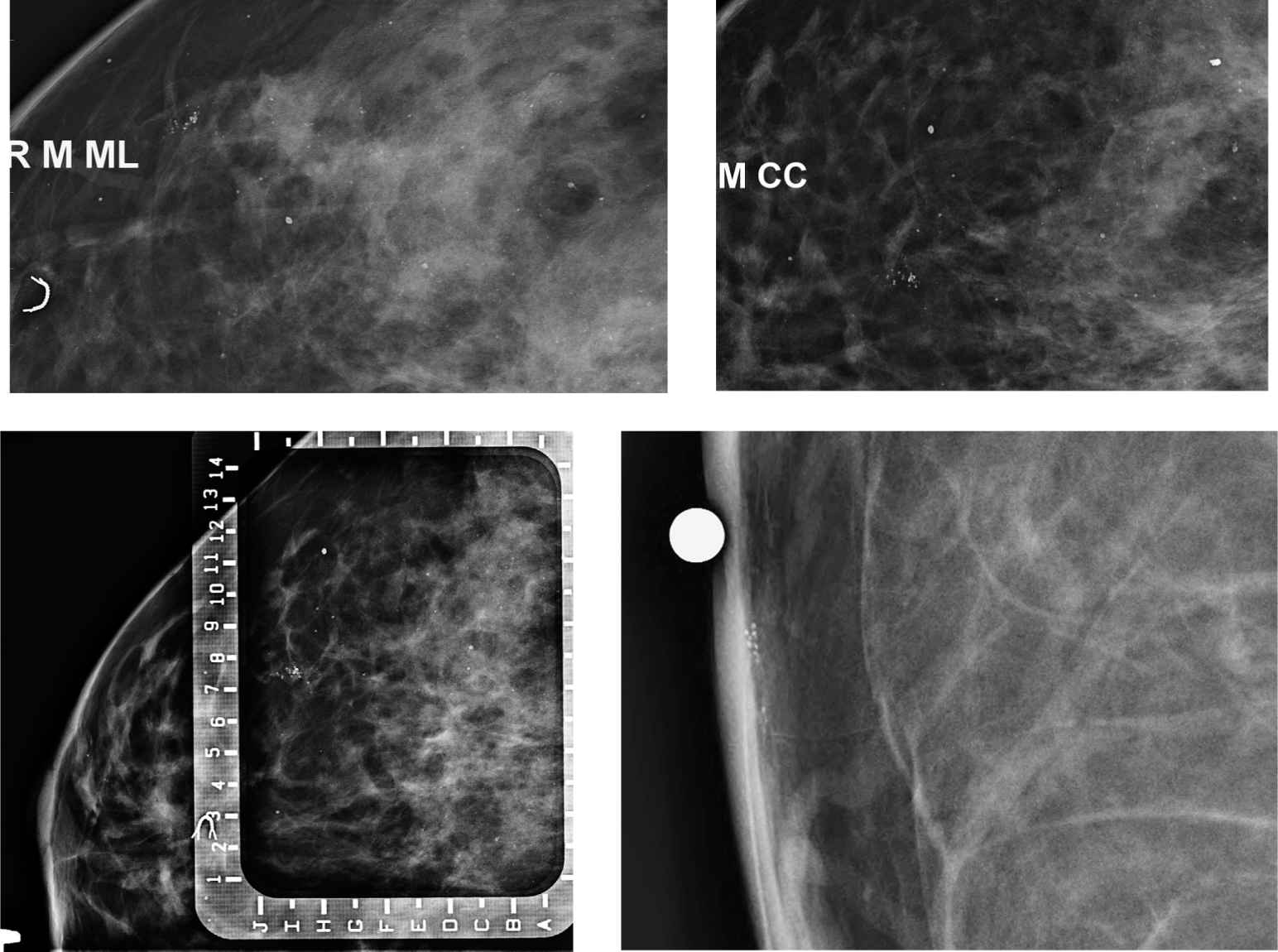
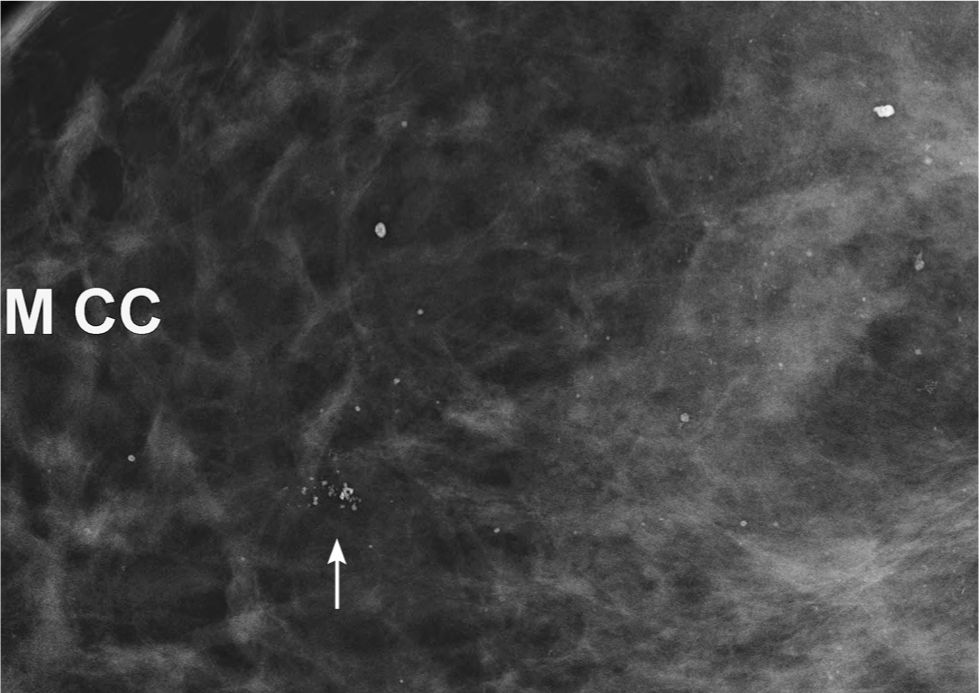
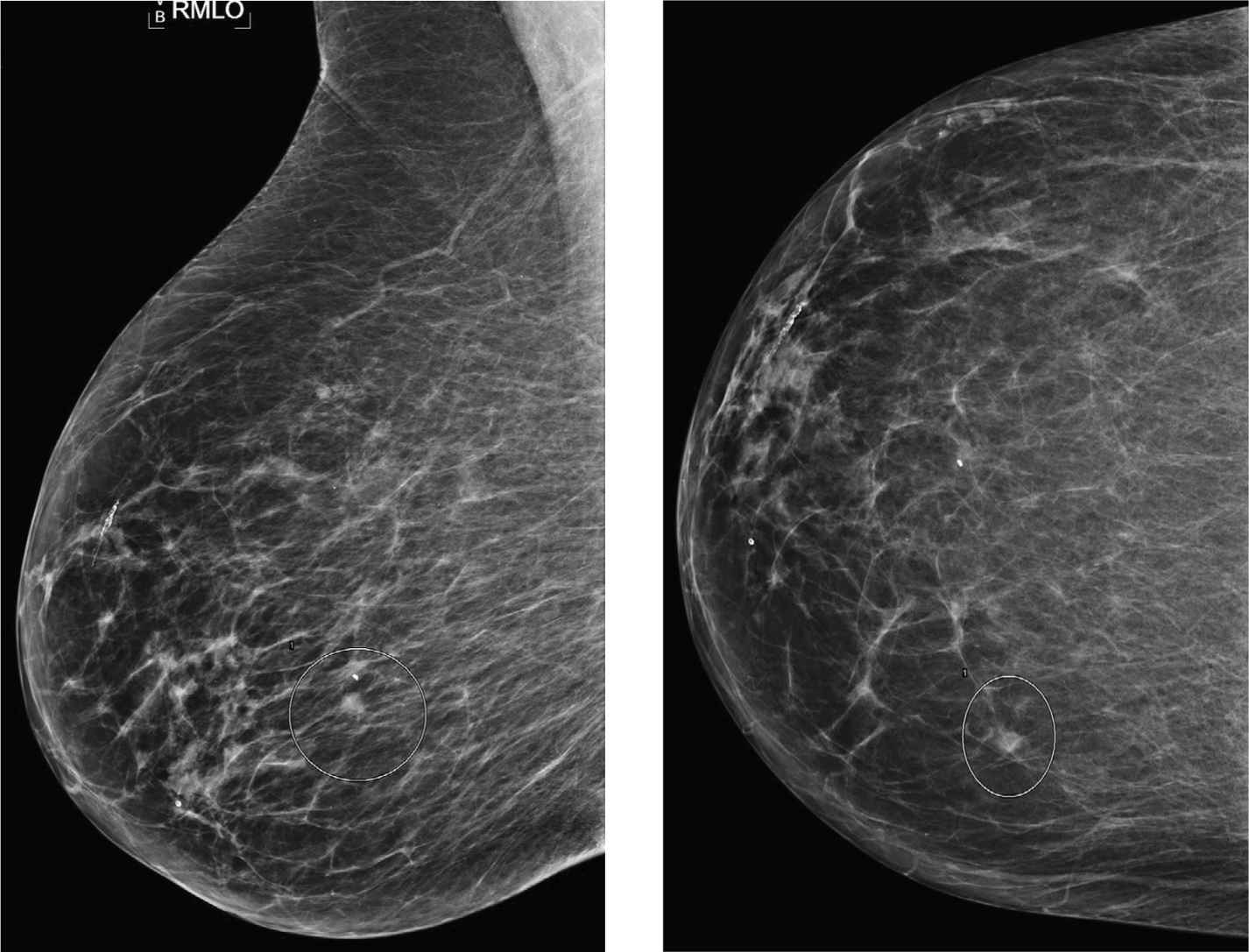
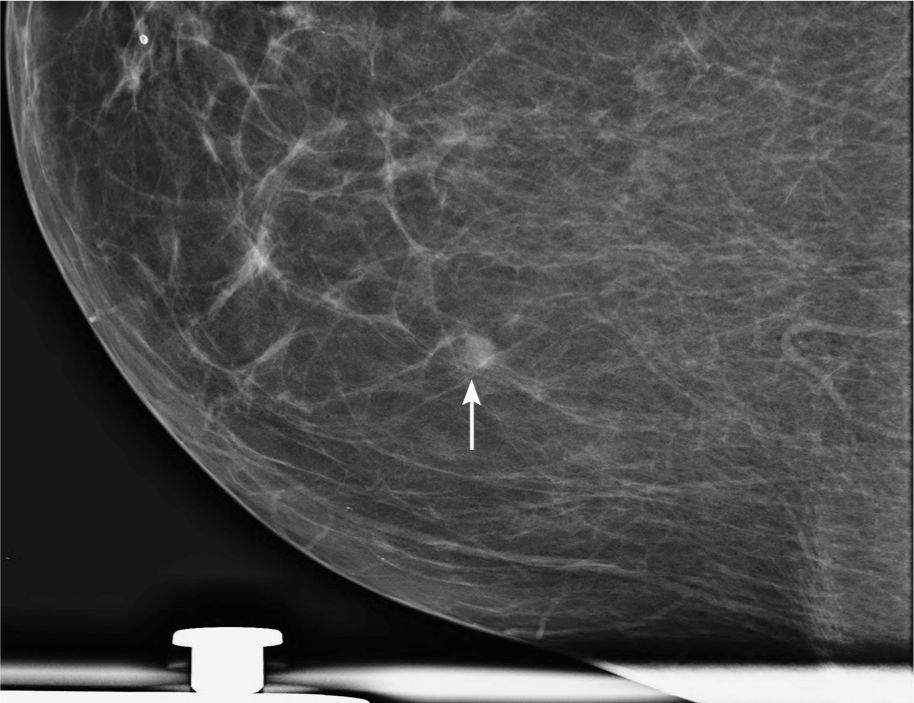
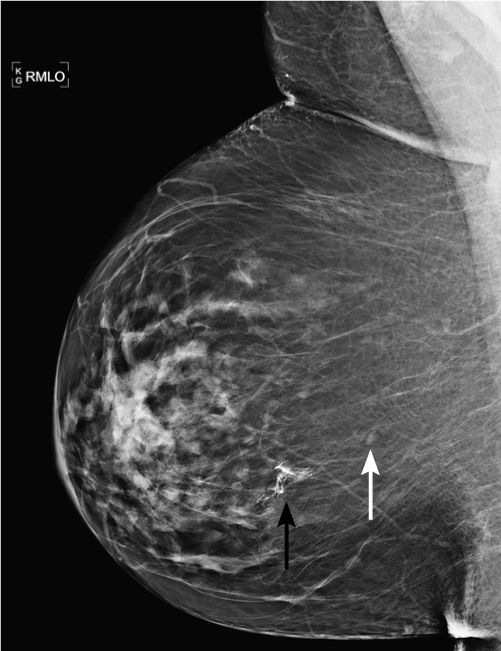
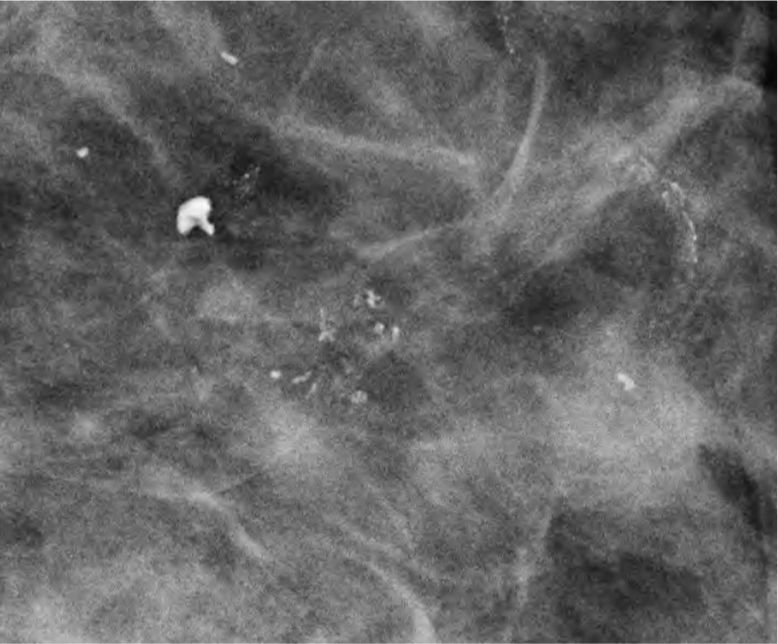
Diagnostic mammogram of right magnification CC view (additional electronically magnified) demonstrating several groups of “amorphous” calcifications.
Answers
1. Architectural distortion in the superior medial breast.
2. Differential diagnosis includes radial scar, malignancy, or prior surgery.
3. Any malignancy can result in the presence of distortion, but in general typical for this appearance would be tubular carcinoma. Tubular carcinoma is a malignancy with relatively good prognosis.
4. There are at least four groups of “amorphous” calcifications in proximity to the area of architectural distortion.
5. Given that all groups are similar in morphology, it would be reasonable to biopsy one group only as done in this case. Depending on the result, in case of positive for malignancy or atypia, all groups should be included into the excision. If the biopsy demonstrates benign, histology findings can be followed in 6 months.
Suggested Reading
D’Orsi CJ, Bassett LW, Berg WA, et al. Breast Imaging Reporting and Data System: ACR BI-RADS Mammography. 4th ed. Reston, VA: American College of Radiology; 2003.
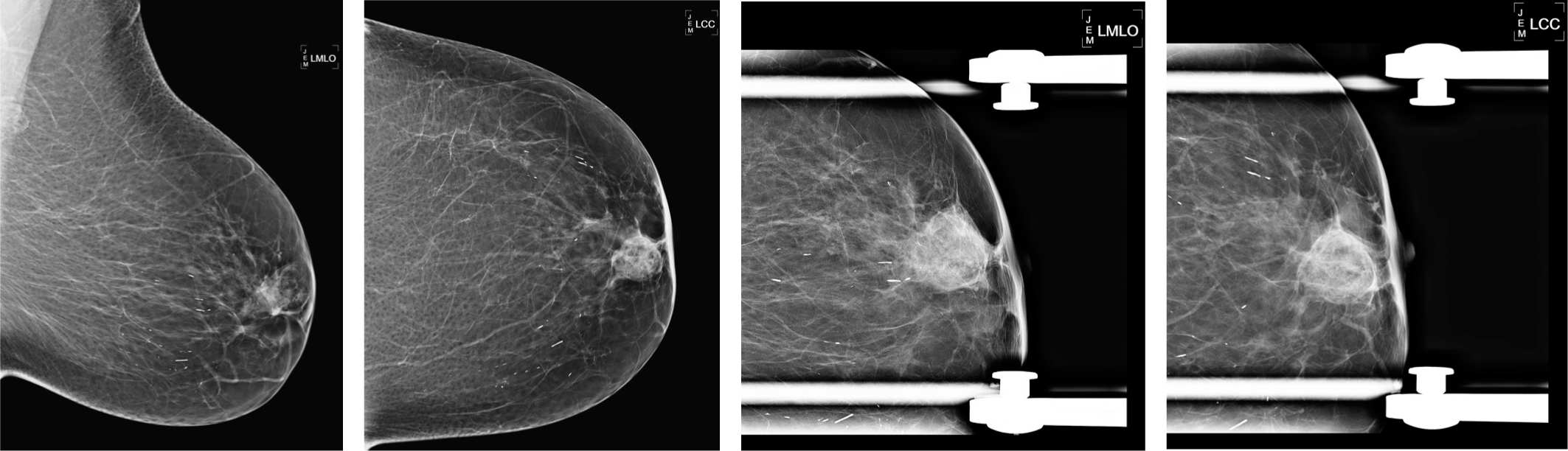
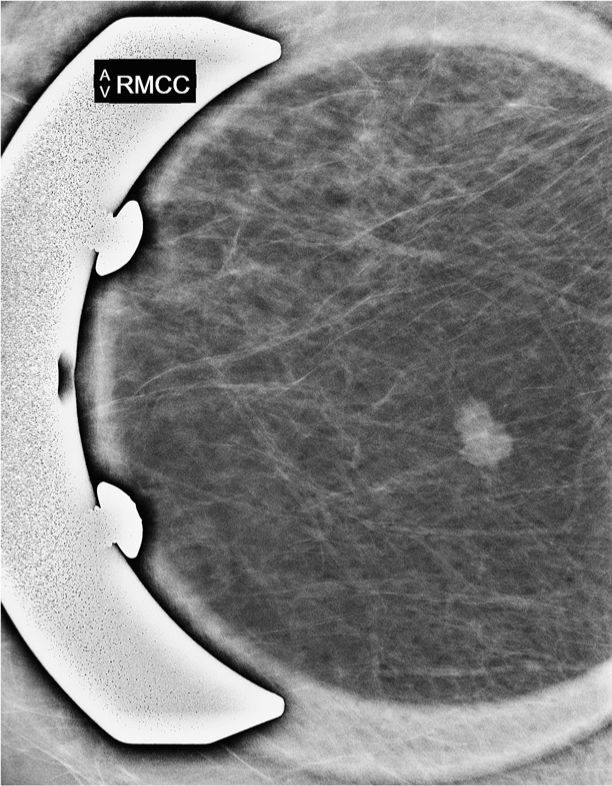
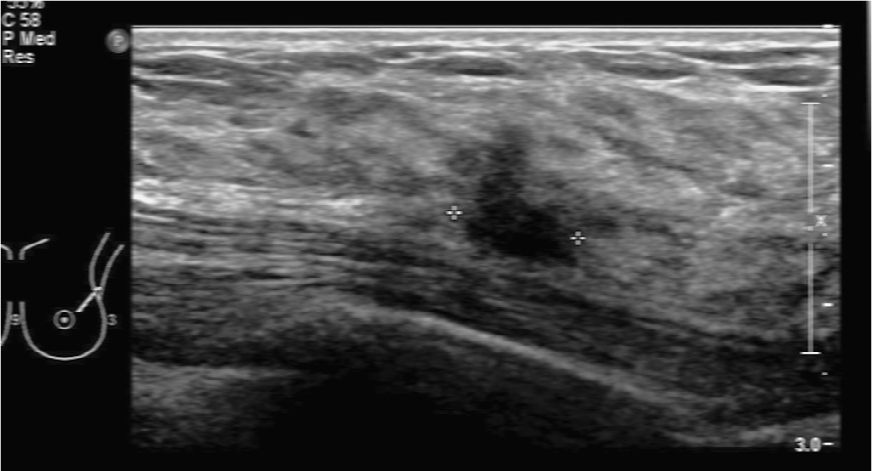
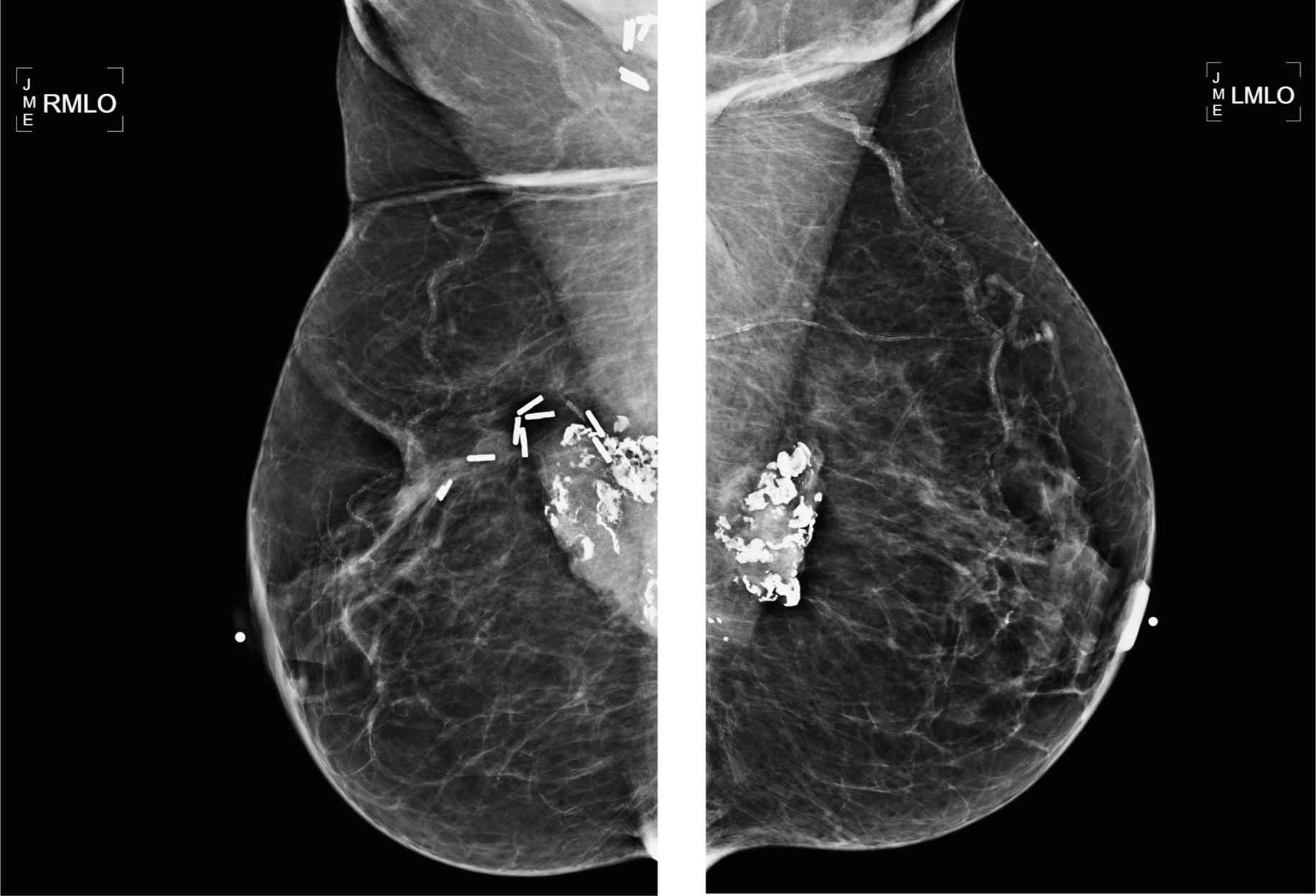
Prior right mastectomy and new palpable lump in contralateral breast
1. What BI-RADS classification should be used here?
2. What should be the next diagnostic imaging exam?
3. What are the causes of fat necrosis?
4. What calcification descriptor would you use in this case?
5. What type of biopsy would you recommend?
Fat necrosis in remaining breast 1797
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
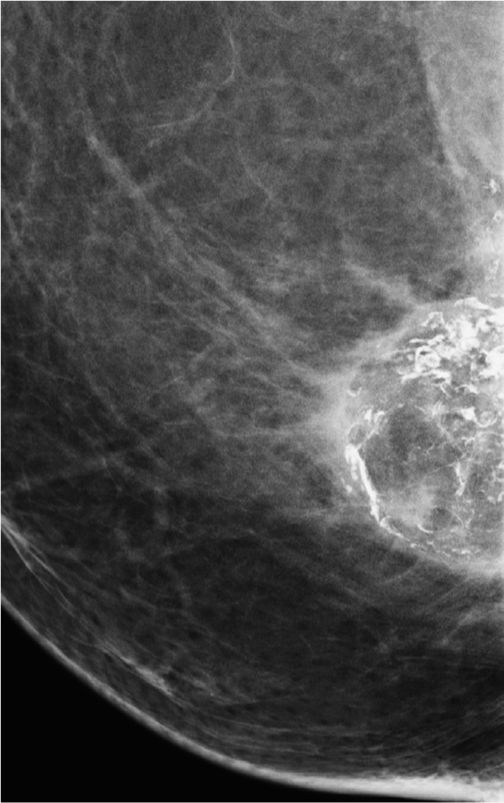
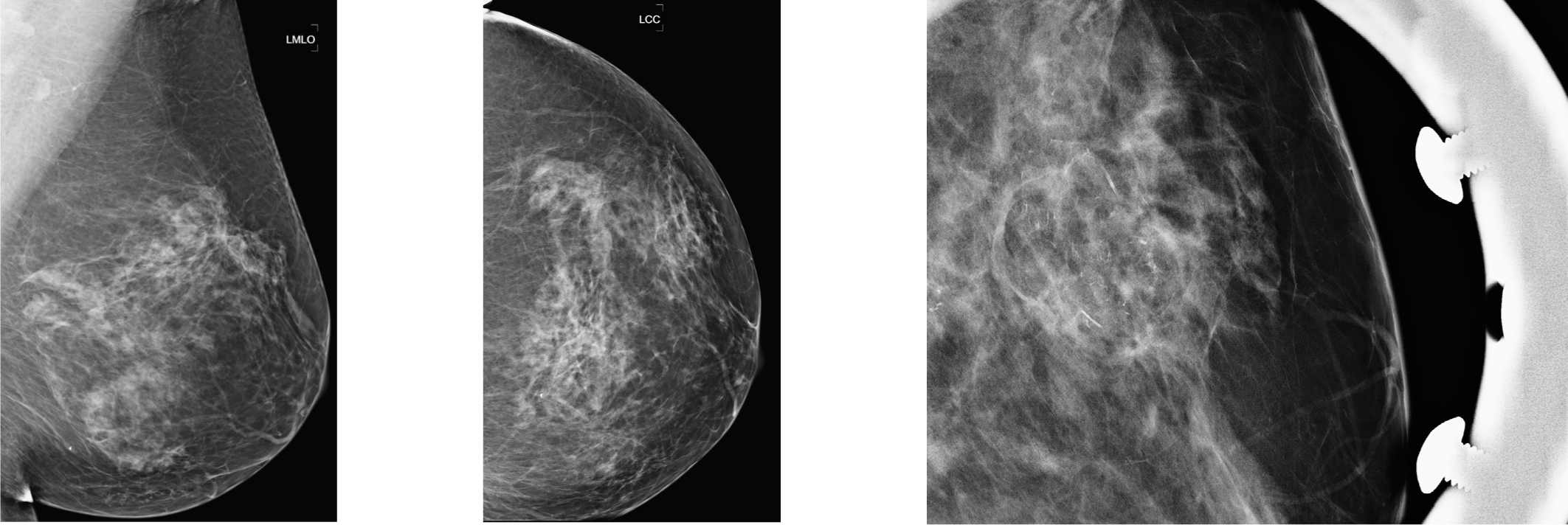
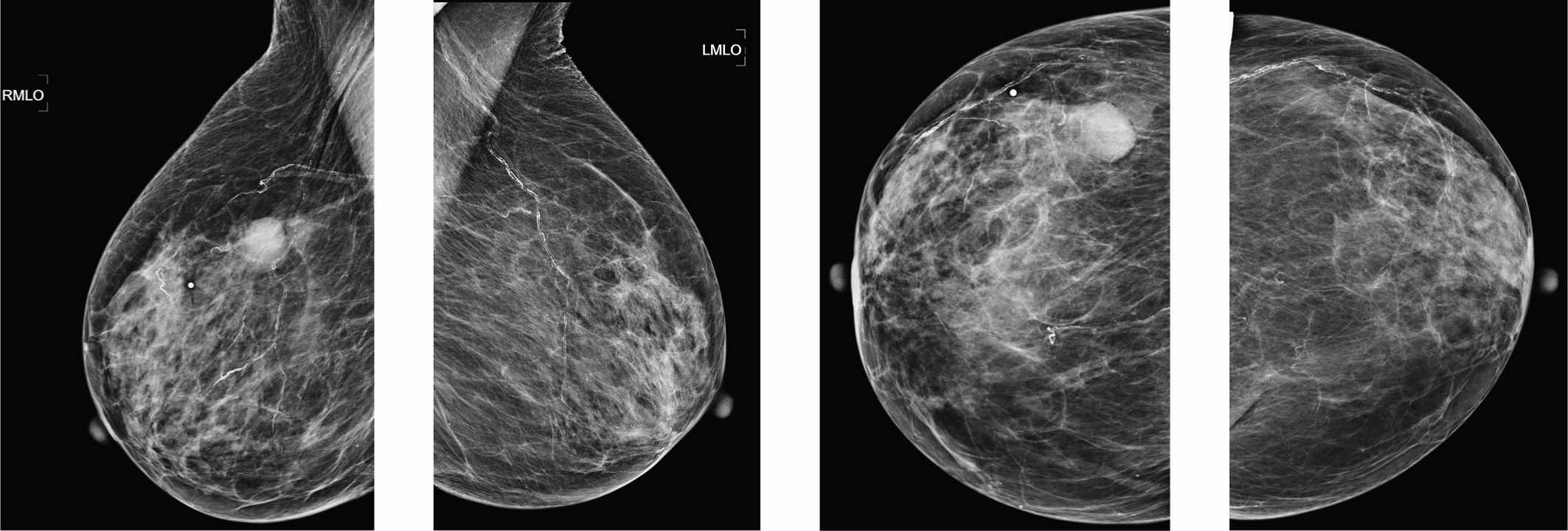
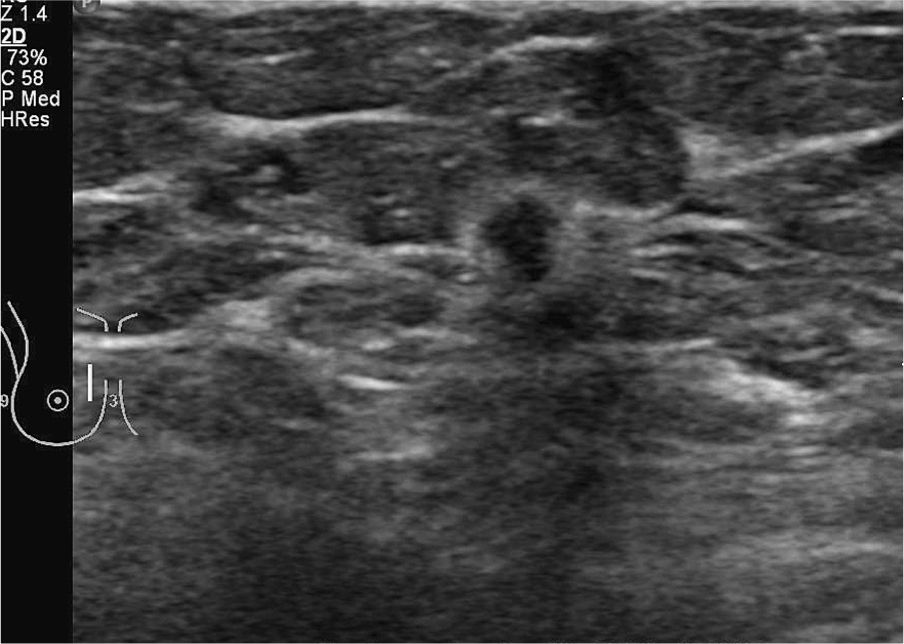
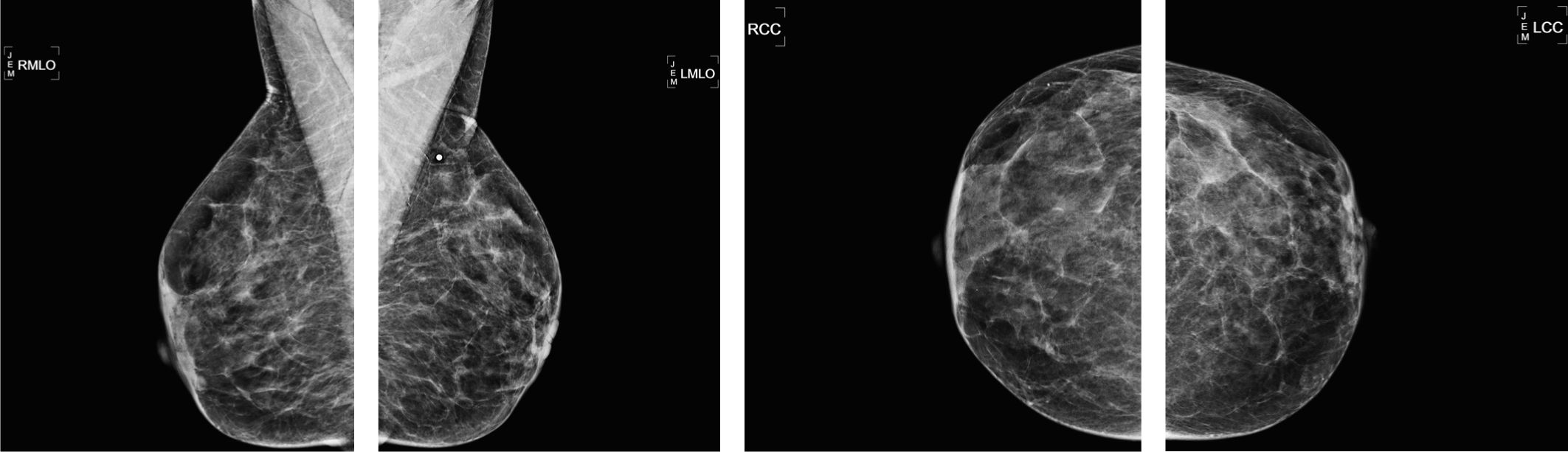
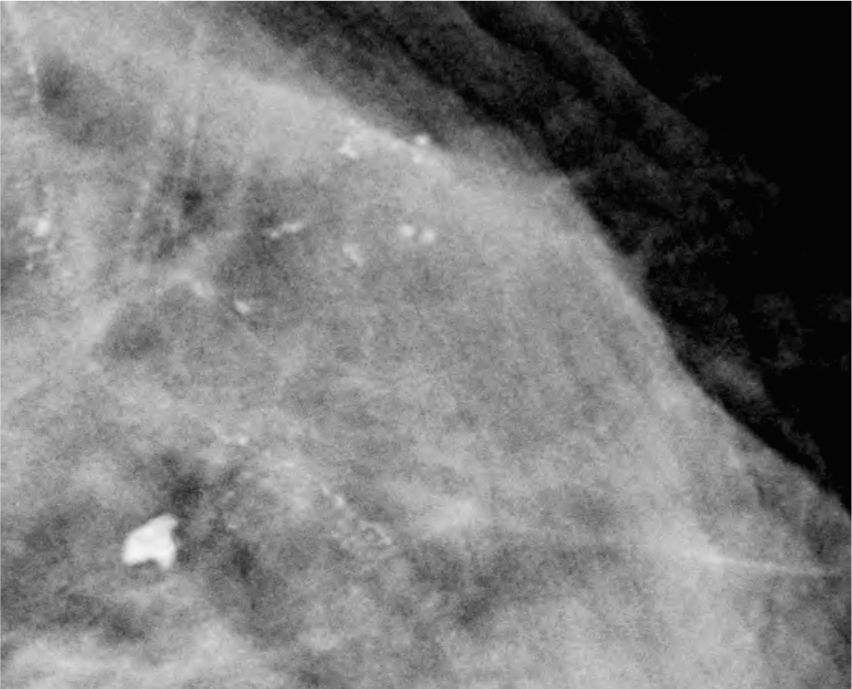
Left CC spot magnification view.
Left ML spot magnification view.
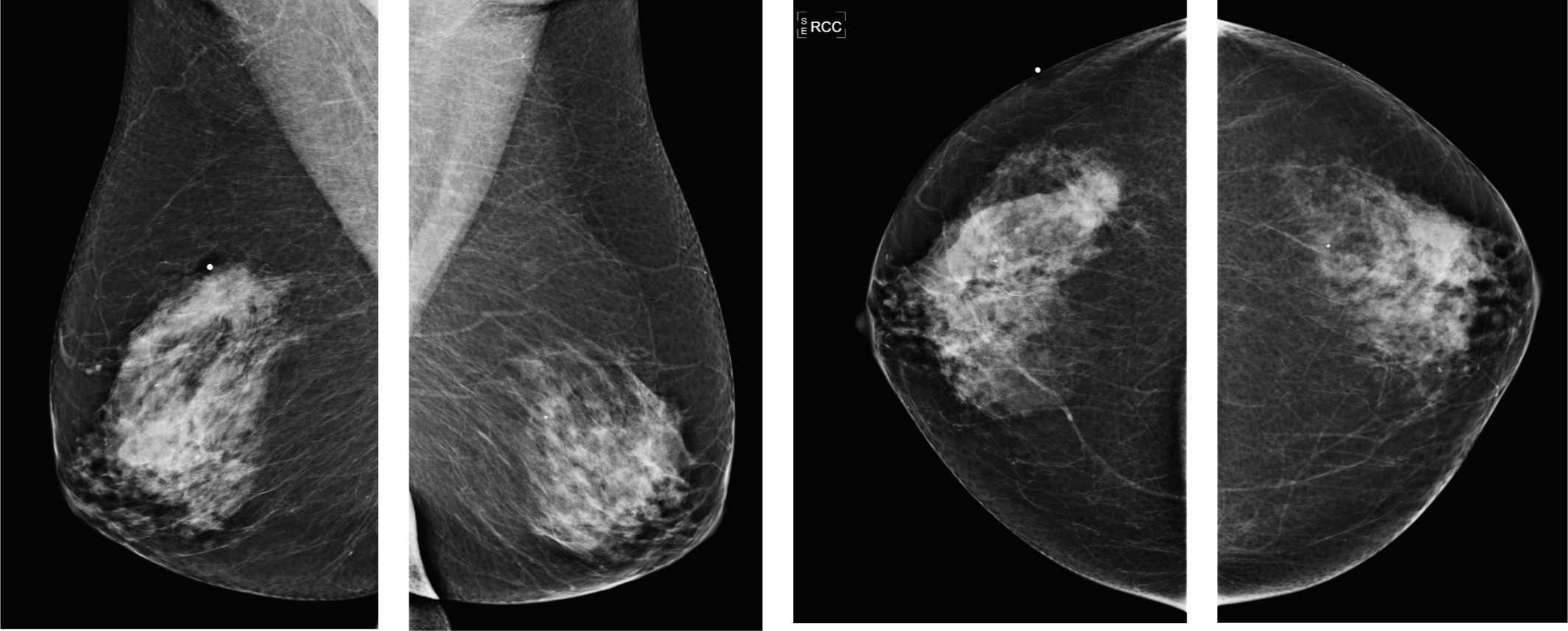
Different patient, similar mass but with much more calcifications.
Answers
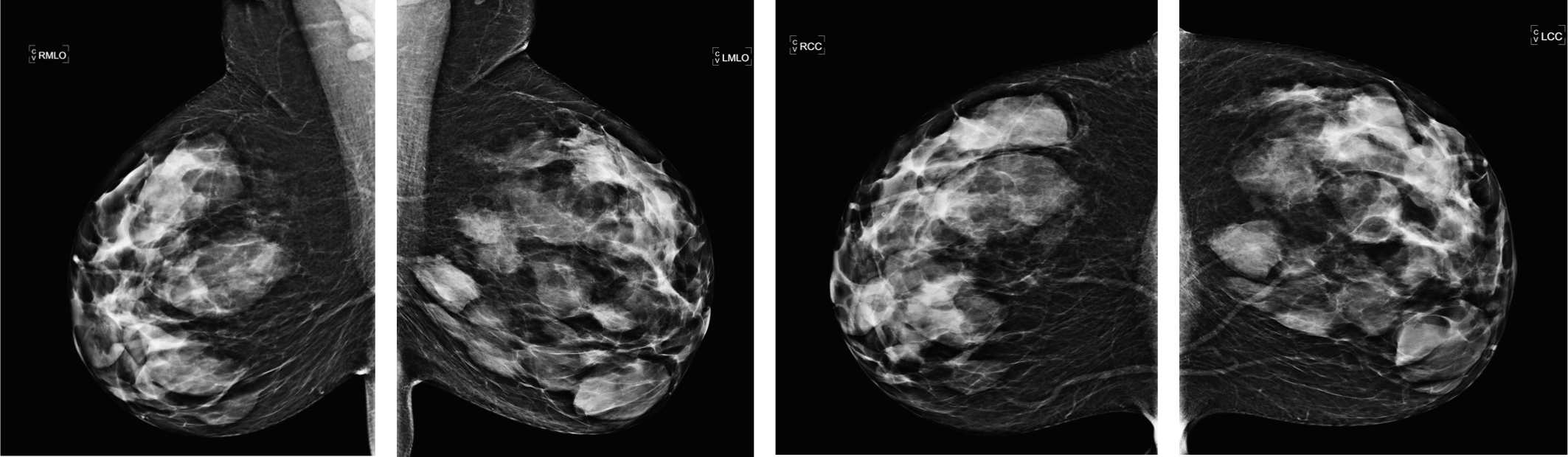
1. These calcifications are mainly denser, rod like, and seen in orthogonal planes to lie around the periphery of the fat density mass. Fat density masses are characteristically benign. The appropriate assessment is therefore BIRADS 2.
2. As there is calcification present, spot magnification views should be performed to characterize the calcific particles. Tomosynthesis may visualize an associated mass better. Ultrasound can be characteristic, with cystic changes and hyper-echogenicity. It can, however, be suspicious when there is calcification in the inflammatory wall of the necrosis. Non–fat-saturation MRI sequence would help to distinguish, if any remaining doubt.
3. Most of the above points may be a cause of fat necrosis. It is a response to injury, whether minor, as in grandchildren or pets climbing on to chest, or to a reaction to surgery and radiation treatment (can be marked in patients having intraoperative brachytherapy. Plastic surgery is a potent cause of fat necrosis.
4. Use of the “linear calcifications” descriptor is a suspicious term that you would use if you chose to biopsy this lesion. If this is stable and characteristically benign, then you should use a low-risk descriptor such as “curvilinear.”
5. This patient has a palpable finding, and if you were concerned about the calcifications, stereotactic core biopsy could be performed. However, the calcifications are associated with the periphery of the fat necrosis mass, and therefore performing an ultrasound core biopsy of the margin of the mass and performing a specimen x-ray could be just as diagnostic.
Suggested Readings
Bilgen IG, Ustun EE, Memis A. Fat necrosis of the breast: clinical, mammographic and sonographic features. Eur J Radiol. 2001;39(2):92-99.
DiPiro PJ, Meyer JE, Frenna TH, Denison CM. Seat belt injuries of the breast: findings on mammography and sonography. AJR Am J Roentgenol. 1995;164(2):317-320.
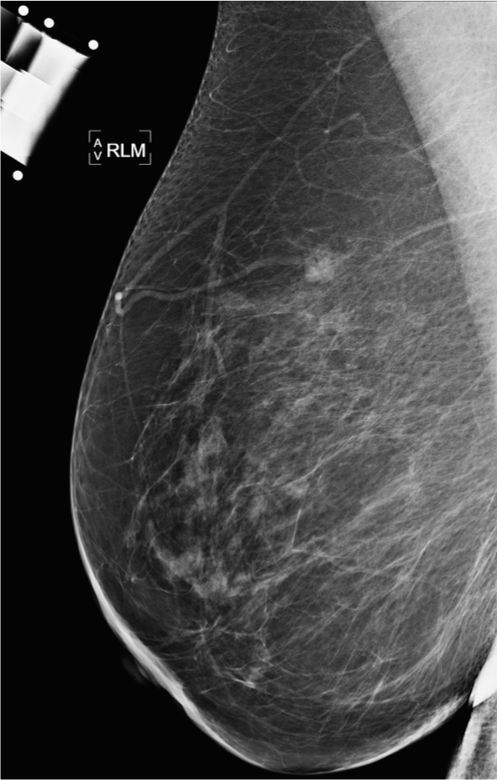
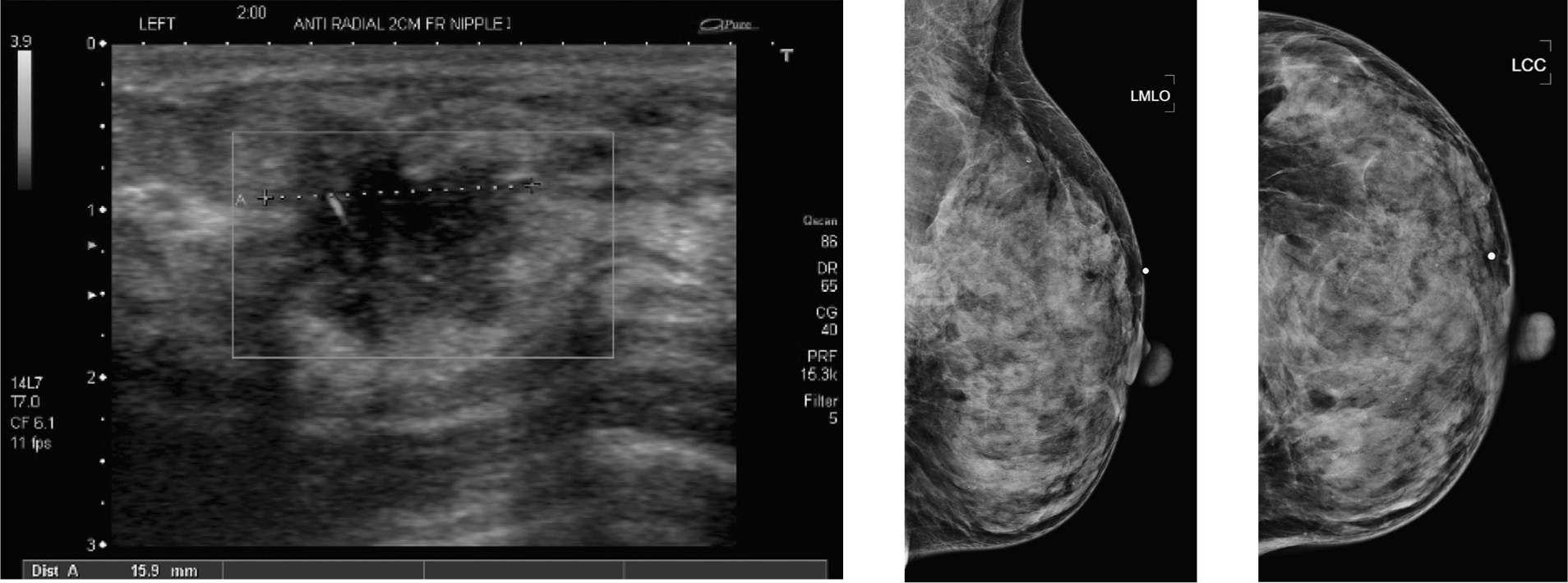
Palpable lump in the right breast
1. What BI-RADS classification should be used here?
2. What should be the next diagnostic imaging exam?
3. What is the likely pathology of a circumscribed mass?
4. What type of biopsy would you recommend?
5. If this is a malignancy, what would you expect to see on ultrasound?
Circumscribed breast cancer 1868
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
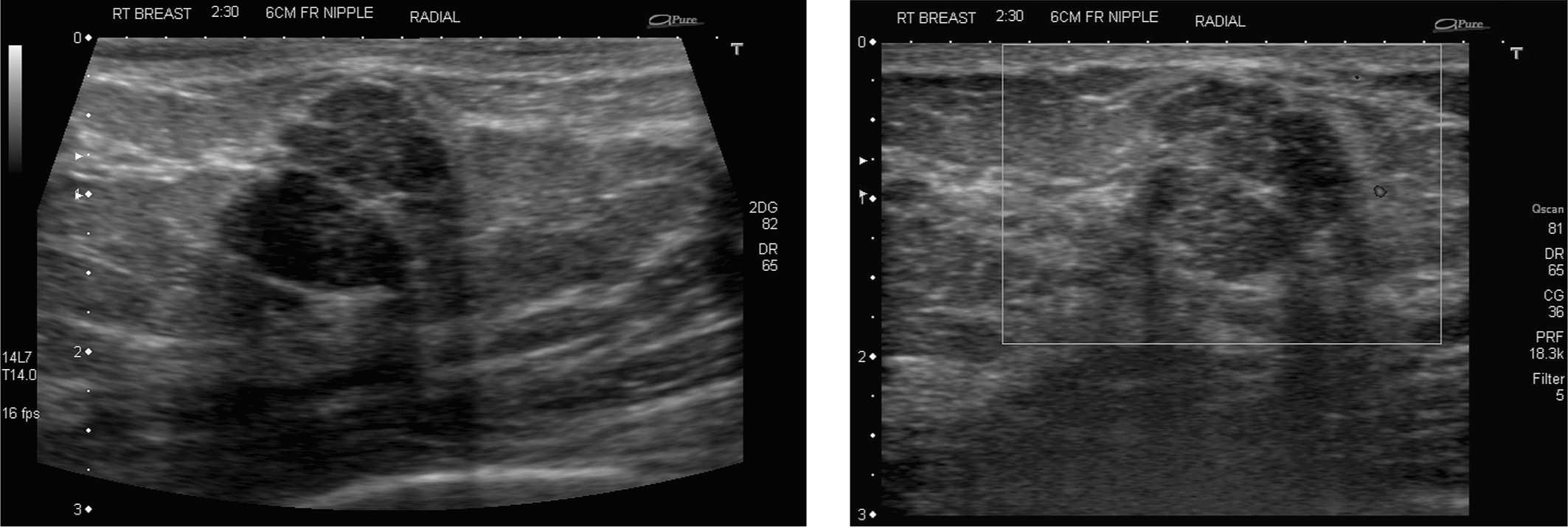
Right CC spot magnification views.
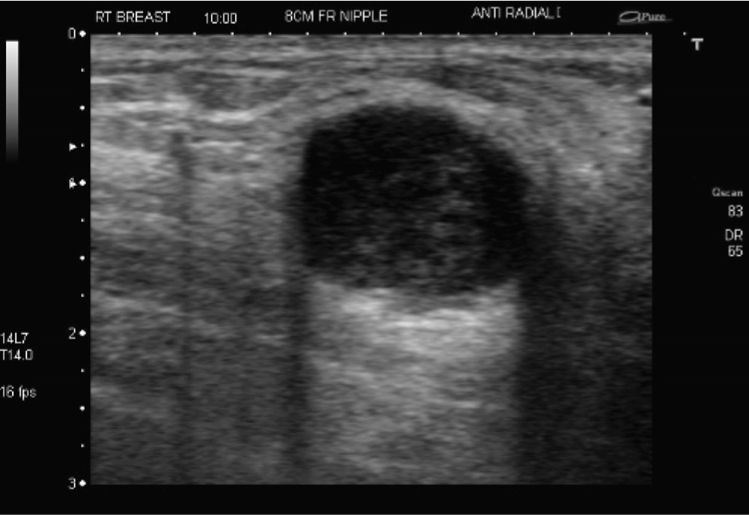
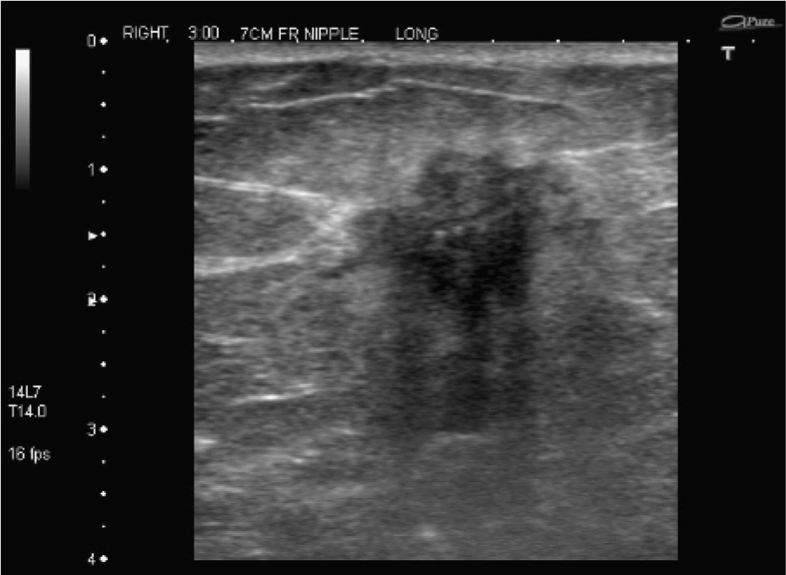
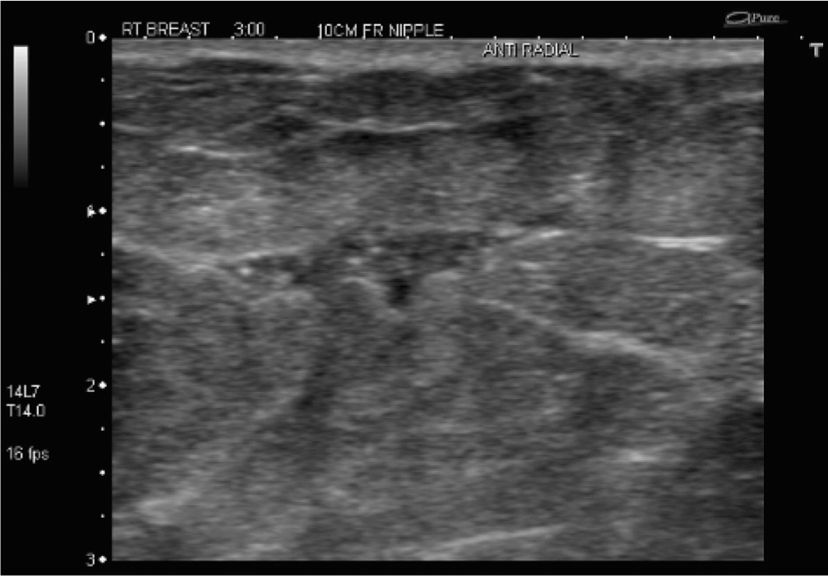
Targeted ultrasound.
Doppler ultrasound of mass.
Answers
1. In this context, this lesion does not fulfill the criteria for a benign mass; therefore, it should be treated with suspicion. See ultrasound images on page 2.
2. Tomosynthesis may not add anything extra in this lesion, but, in general, it is said to be equal to regular diagnostic projections for analyzing the margins of the mass. Ultrasound is the next most important exam to determine the nature of the lesion, and in this type of case, some would go directly to ultrasound from conventional mammography. MRI is not likely to add additional useful information. Core biopsy should not be performed before the diagnostic workup is complete.
3. In older patients who still have cysts, they may have stuck around for decades, and contain proteinaceous debris, such that there will never be a simple cyst, and likely to have appearances of a complicated cyst. Note: the term complex cyst was dropped in 2003 with the 4th edition of BI-RADS, as it was confusing. In the elderly and in the young, a malignancy may grow with circumscribed margins.
4. Ultrasound-guided core biopsy is appropriate here, as it is easy to find, cheap, and quick to perform. If the lesion was isoechoic and not easily visible, then stereotactic core biopsy would be appropriate.
5. The mass usually has some internal echoes (which may be difficult to appreciate if the patient has a mucus-secreting tumor). Vascularity within a mass is a suspicious ultrasound finding. The echo pattern is usually mixed echo (or heterogeneous) pattern.
Suggested Readings
Boisserie-Lacroix M, Mac Grogan G, Debled M, et al. Radiological features of triple-negative breast cancers (73 cases). Diagn Interv Imaging. 2012;93(3):183-190.
Gwak YJ, Kim HJ, Kwak JY, et al. Ultrasonographic detection and characterization of asymptomatic ductal carcinoma in situ with histopathologic correlation. Acta Radiol. 2011;52(4):364-371.
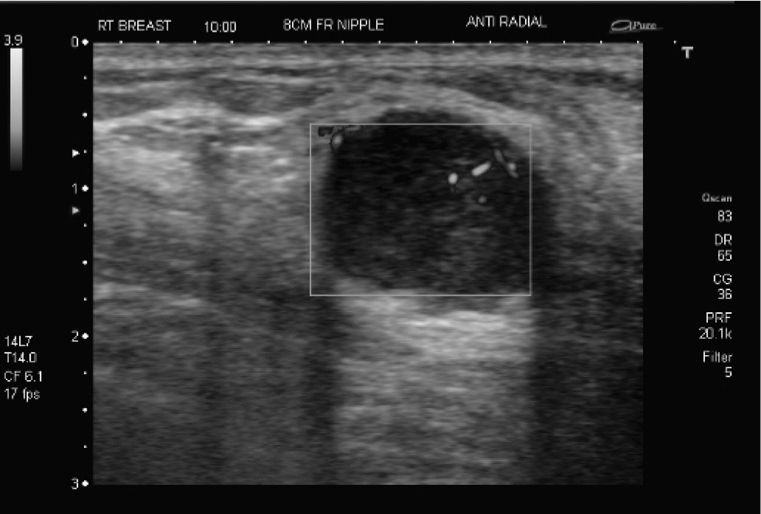
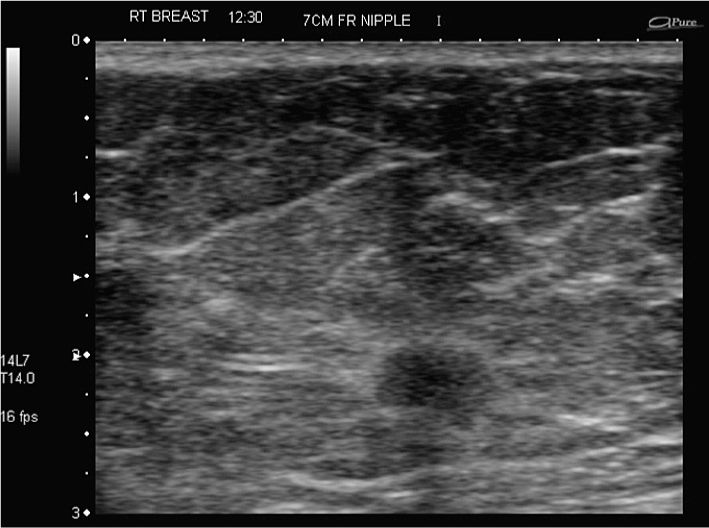
History of infection several months ago—now palpable lump
1. What is the best descriptor explaining the palpable abnormality?
2. What is the most likely reason for the palpable lump?
3. What are other typical findings of fat necrosis on mammography?
4. What are the features of fat necrosis on ultrasound?
5. What is an appropriate final assessment?
Fat necrosis 1310
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic

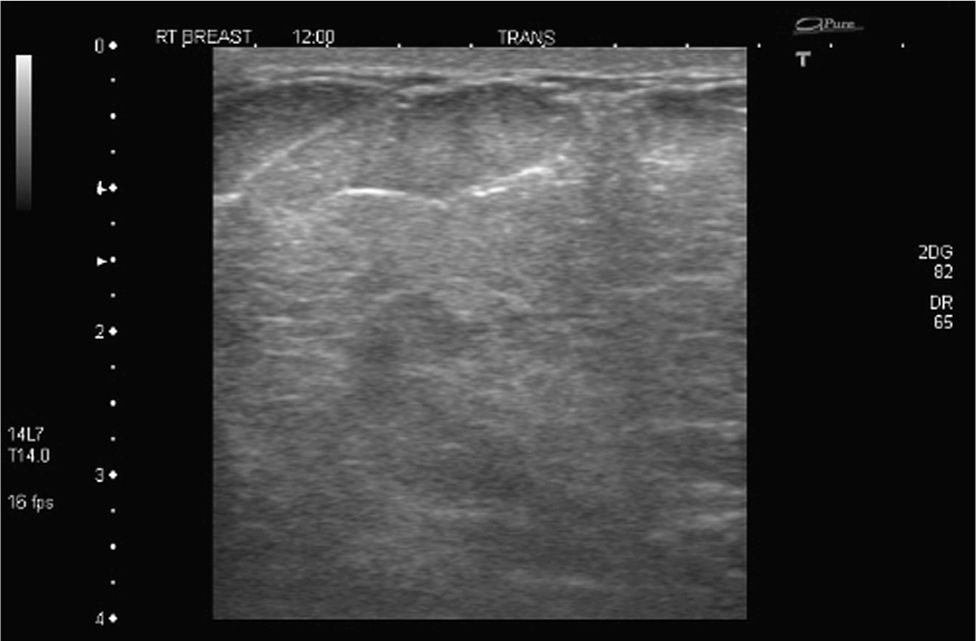
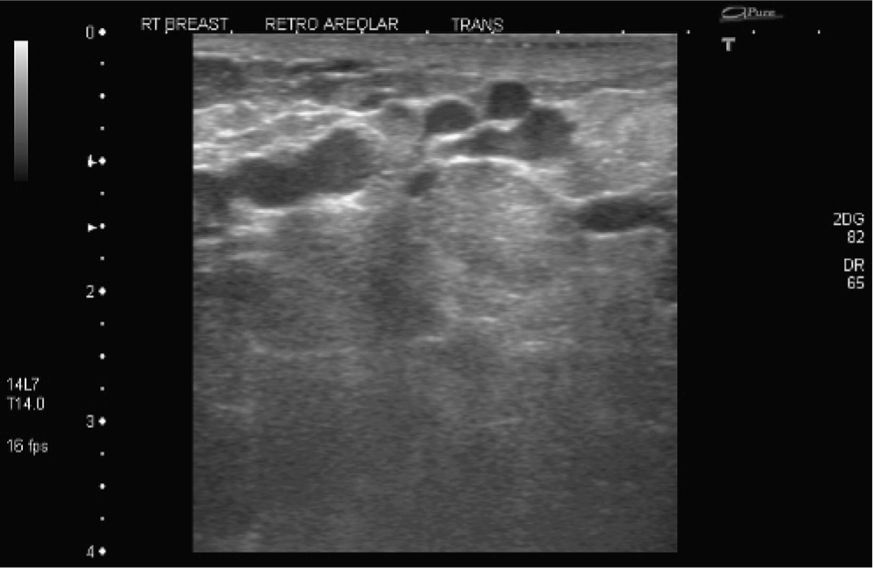
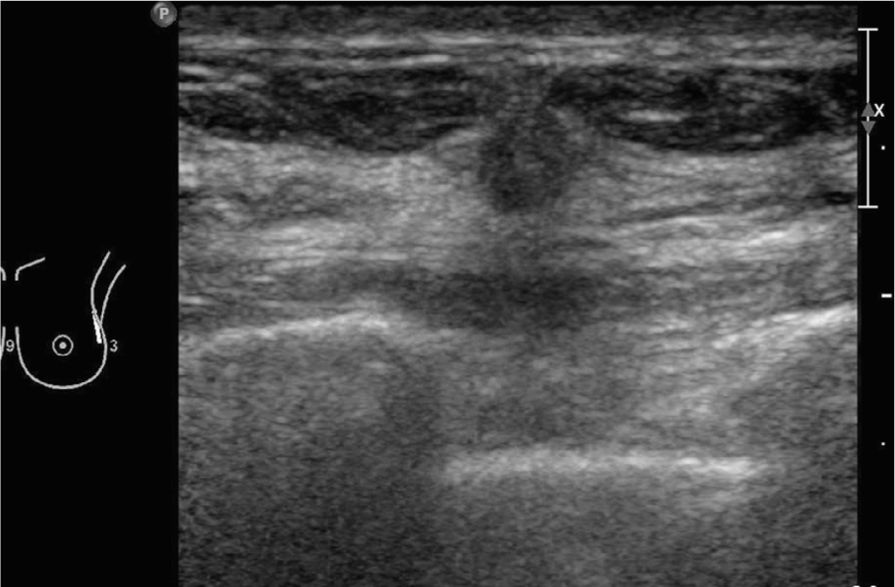
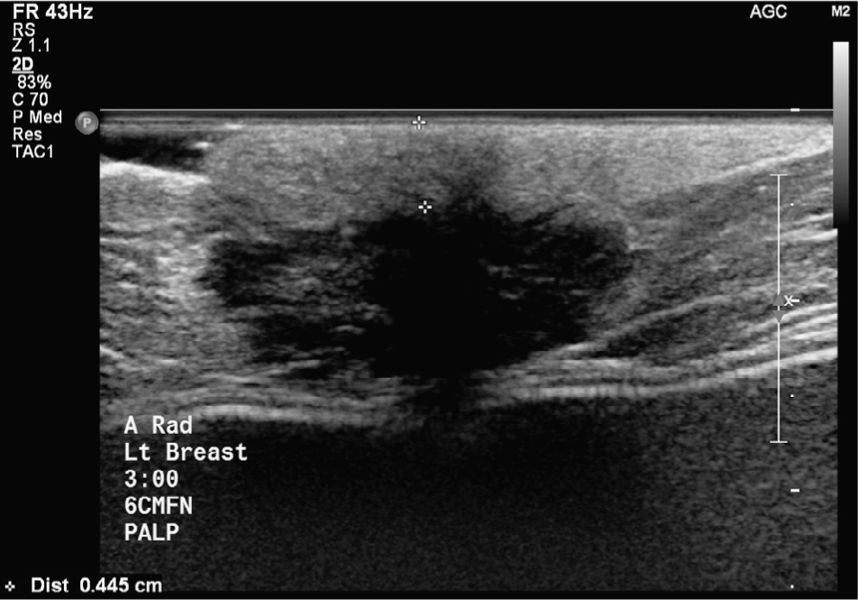
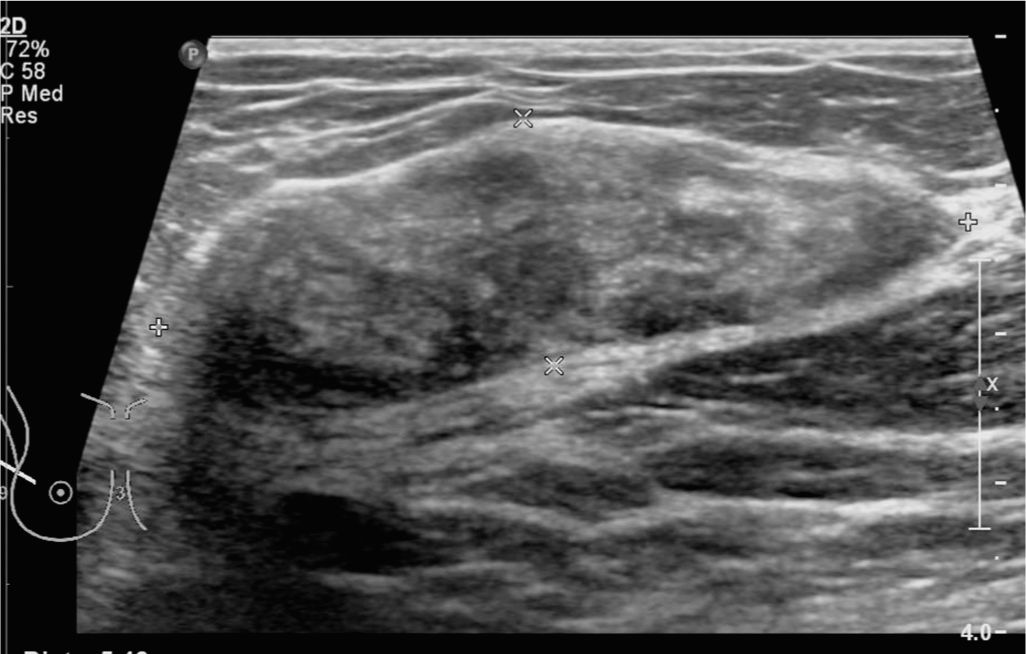
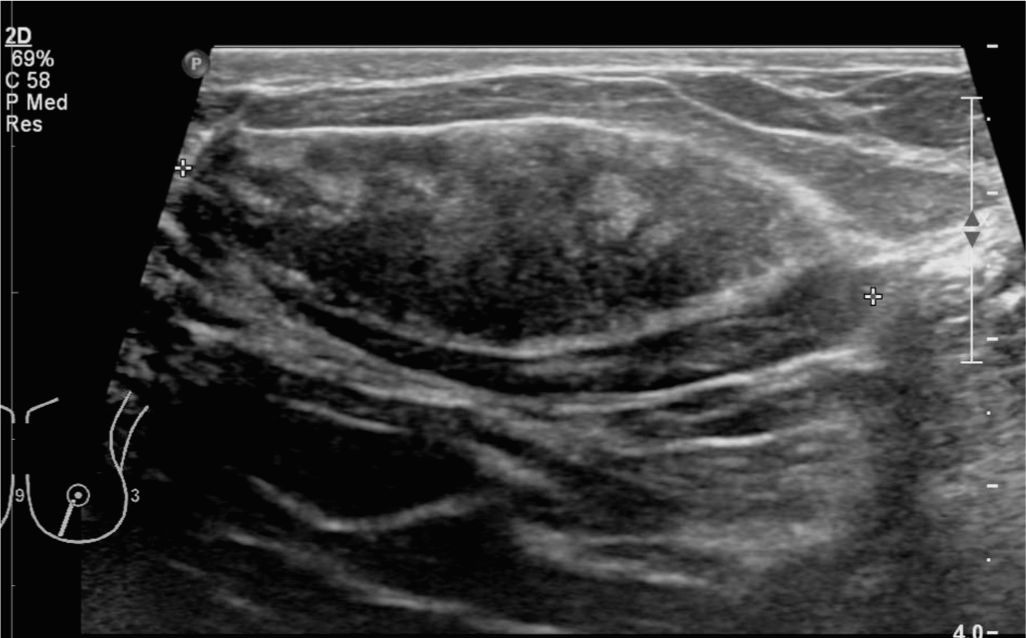
Diagnostic ultrasound demonstrates corresponding “complex mass” with mixed echogenicity and posterior shadowing.
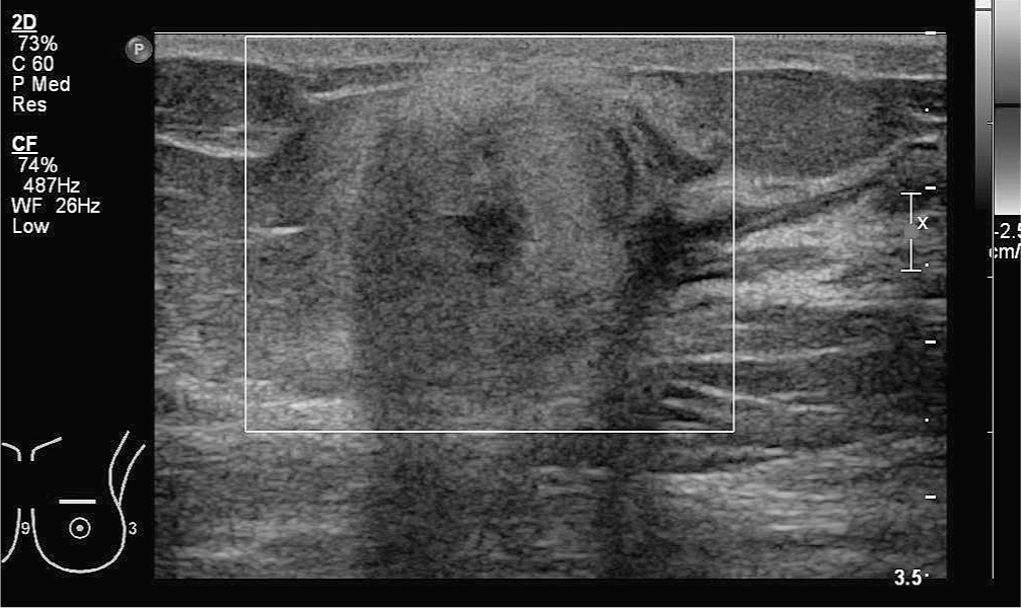
Diagnostic ultrasound demonstrates corresponding “complex mass” without increased flow on duplex.
Answers
1. Finding is consistent with round mass with “heterogeneous” density. It includes areas of low, fat-like density.
2. Given the history of recent infection, the finding most likely represents fat necrosis. The mammogram finding does correlate to fat necrosis given its heterogeneous density including areas of low fat density.
3. Fat necrosis can present in many different forms. Some findings are specific and can be classified as BI-RADS 2: benign, for example, fat-containing oil cysts, curvilinear calcifications associated with radiolucent mass. Some findings are more indeterminate such as “coarse” calcifications. Some findings cannot be differentiated from malignancy, and biopsy cannot be avoided, for example, in case of “spiculated” mass.
4. Fat necrosis again can show up in many different forms. Well-circumscribed mass may be classified as BI-RADS 2 or BI-RADS 3, while heterogeneous mass or ill-defined masses are unspecific and malignancy is difficult to exclude.
5. Given the presence of new palpable mass after infection, appropriate assessment is BI-RADS 3 (probably benign) and 6-month follow-up with mammogram.
Suggested Reading
Taboada JL, Stephens TW, Krishnamurthy S, Brandt KR, Whitman GJ. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009;192(3):815-825.
Screening—asymptomatic
1. What is the correct BI-RADS classification in this case?
2. What is the next imaging test?
3. What are the features of a mass that distinguish a lymph node from another mass on mammography?
4. What are the features of a normal lymph node on ultrasound?
5. What ultrasound features are considered suspicious?
Small posterior cancer simulates intramammary lymph node 1838
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
Right mediolateral.

Right ML spot magnification.
Right CC spot magnification shows “irregular” mass.
Targeted ultrasound.
Answers
1. This patient is a screening patient with a normal physical examination. The finding should therefore be given a BI-RADS 0 and further views plus ultrasound scanning recommended.
2. If you have tomosynthesis, then that test will replace the need for multiple examinations to determine the margins of the mass. Ultrasound will be required to determine the likely nature of the mass. There is no indication for an MRI at this stage.
3. The only features that help you make a diagnosis of lymph node from other type of mass is the presence of a hilum, either as a fatty lucency within the mass or as a radiological notch. Those are the pathognomonic features of a node. Supporting features include the typical position for an intramammary lymph node.
4. A vascular hilum and a thin smooth cortex are the features of a lymph node. Remember that the node can be enlarged and therefore reactive following a diagnostic biopsy.
5. According to BI-RADS ultrasound, an “irregular mass” with “angular” or “microlobulated” margins are the descriptors of a suspicious lesion which should be biopsied. The “narrow zone of transition” is the opposite of the suspicious finding of a bright echogenic margin to a mass. The “parallel” orientation is the opposite of a taller-than-wide (or “non-parallel”) mass that would be a suspicious finding.
Suggested Readings
Hogan BV, Peter MB, Shenoy H, Horgan K, Shaaban A. Intramammary lymph node metastasis predicts poorer survival in breast cancer patients. Surg Oncol. 2010;19(1):11-16.
Pugliese MS, Stempel MM, Cody HS, Morrow M, Gemignani ML. Surgical management of the axilla: do intramammary nodes matter? Am J Surg. 2009;198(4):532-537.
Vijan SS, Hamilton S, Chen B, Reynolds C, Boughey JC, Degnim AC. Intramammary lymph nodes: patterns of discovery and clinical significance. Surgery. 2009;145(5):495-499.
Lump in the left axillary tail
1. What BI-RADS classification should be used here?
2. What is the most likely pathology based on the imaging?
3. What mammographic views should you perform with these findings?
4. If you find abnormal nodes in the axilla, below the axillary vein, what levels are involved?
5. As a node is present, what staging tests would you perform?
Axillary tail IDC plus DCIS plus lymph node 1762
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
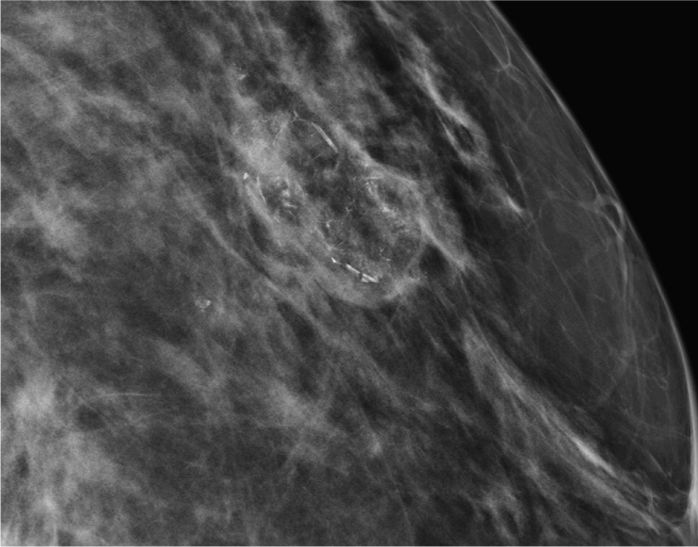
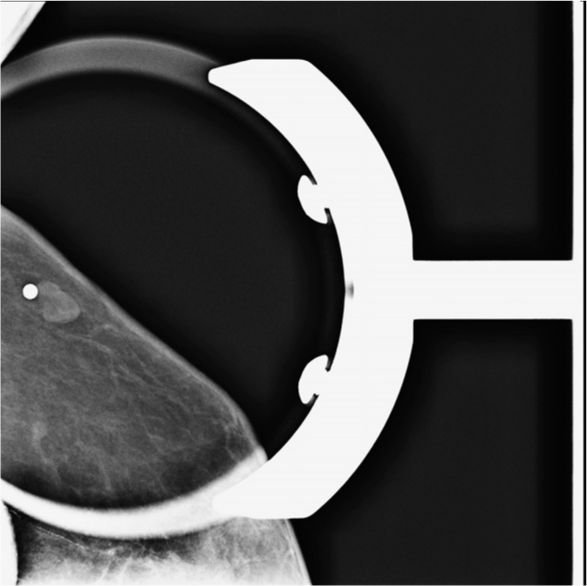
Left ML spot magnification view—in this plane, the masses are not easily seen.
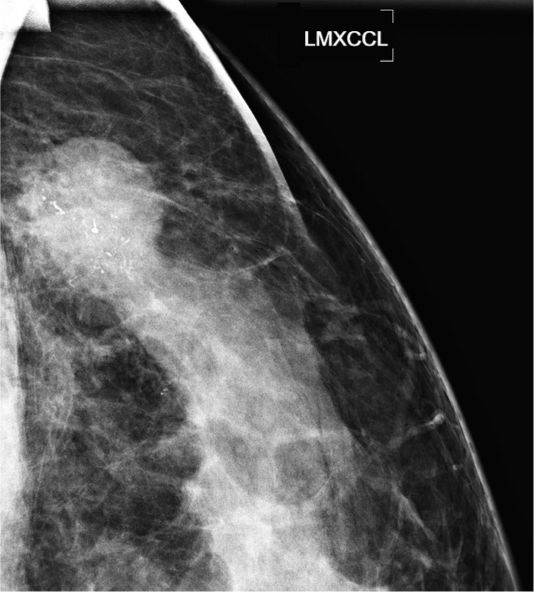
LXCCL spot magnification shows the lateral mass at the edge of the breast disc.
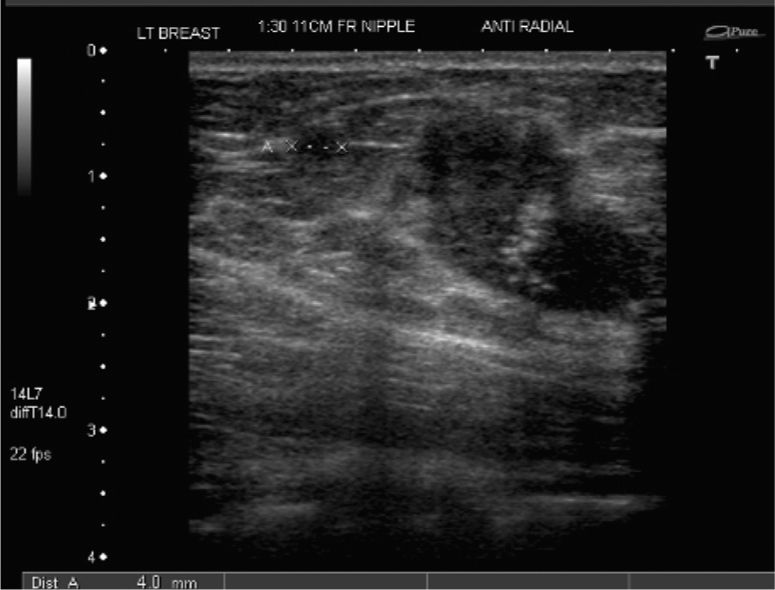
Left breast ultrasound shows not only the main lesion as an irregular mass containing calcification but also a second mass separate from the main mass consistent with a satellite lesion.
Left axillary ultrasound—here the enlarged solid node seen on mammography is demonstrated. Core biopsy confirmed metastatic adenocarcinoma.
Answers
1. BI-RADS 4 or 5 can be used here. The combination of features of an “irregular mass” containing highly suspicious microcalcification plus an abnormal lymph node allows BI-RADS 5 to be used.
2. The most common pathology with these findings is a high-grade IDC plus DCIS.
3. A lateral view is helpful for localization. However, the tumor is in the axillary tail in this instance, and if the mammo tech cannot get posterior enough, the tumor may not be visualized. An XCCL is helpful to determine the lateral extent of the disease. Spot magnification views are probably the best, as you get the maximum resolution to assess the margins of the mass, and to characterize the calcific particles. The Eklund technique is used to visualize breast tissue in front of the implants, known as the implant displaced view.
4. There is no such thing as level 0 or 4. Level 3 refers to disease superior to the boundary formed by the axillary vein. Levels 1 and 2 refer to the levels below the axillary vein.
5. Ultrasound staging of the locoregional nodes is important when you see a suspected malignancy with possible nodes on a mammogram. If the lesion is large, or is more likely to drain medially due to a central or medial position, then scanning longitudinally immediately alongside the sternum may identify involved internal mammary lymph nodes.
Suggested Readings
Iakovlev VV, Arneson NC, Wong V, et al. Genomic differences between pure ductal carcinoma in situ of the breast and that associated with invasive disease: a calibrated aCGH study. Clin Cancer Res. 2008;14(14):4446-4454.
Meyerson AF, Lessing JN, Itakura K, et al. Outcome of long term active surveillance for estrogen receptor-positive ductal carcinoma in situ. Breast. 2011;20(6):529-533.
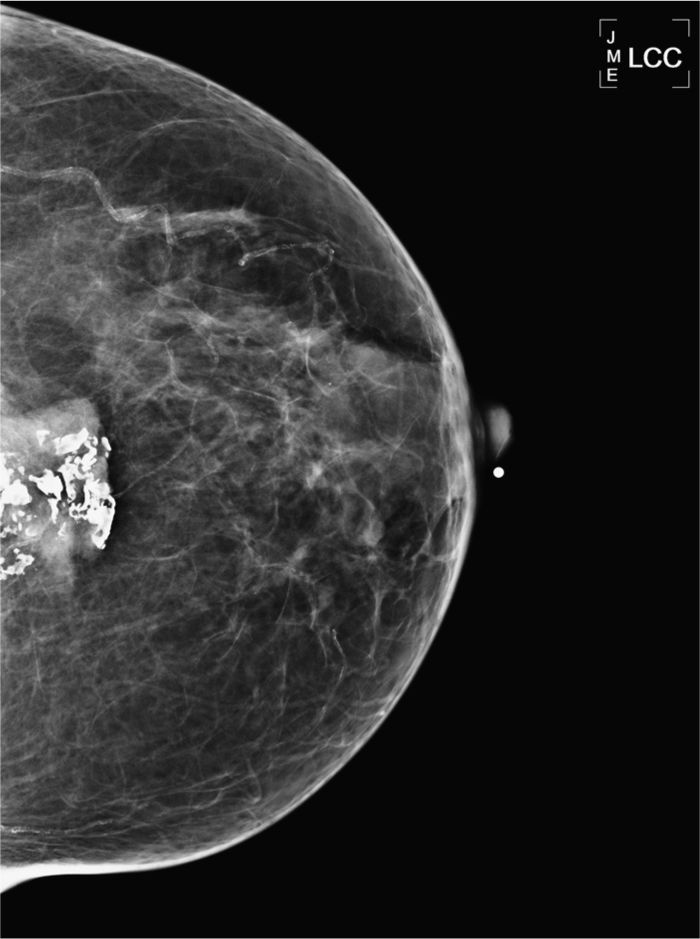
Diagnostic workup of group of indeterminate calcifications
1. What is the best descriptor of this new group of calcification?
2. Why could that group of new calcifications be benign?
3. What is the next step after the standard ML and CC magnification view?
4. What is the appropriate technique to obtain tangential view?
5. What is the final assessment based on the tangential view?
Skin calcifications 1309
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
Diagnostic mammogram, right ML magnification view demonstrating group of indeterminate calcifications.
Diagnostic mammogram, right CC magnification view demonstrating group of indeterminate calcifications.
Diagnostic mammogram, right CC magnification view with grid demonstrating the group of indeterminate calcifications at the coordinates I—7.5.
Diagnostic mammogram, tangential view with BB, demonstrates group of calcifications within the skin.
Answers
1. This is a group of “round and oval” calcifications, one or two of the calcifications demonstrate “lucent center.”
2. Because one or two of the calcifications appear to have lucent center suspects that this could be skin calcifications.
3. Based on the standard ML and CC magnification views, the group of calcifications needs to be further worked up by obtaining a tangential view to prove their location within the skin.
4. The appropriate way is to have a paddle with grid to place a BB on the group of calcifications. An alternative could be to place the patient on the stereotactic biopsy table and place the BB. Next step is to obtain magnification view in second plane tangential to the BB—and thus tangential to the calcifications. Stereotactic biopsy unit could also be used to calculate the Z value, which, in case of the presence of skin calcifications, had to be very small.
5. Calcifications are in the skin—BI-RADS 2 “benign” recommend patient to return for next screening mammogram in 1 year.
Suggested Readings
Berkowith JE, Gatewood OM, Donovan GB, et al. Dermal breast calcifications: localization with template-guided placement of skin marker. Radiology. 1987;163(1):282.
Linden SS, Sullivan DC. Breast skin calcifications: localization with a stereotactic device. Radiology. 1989;171(2):570-571.
Palpable finding in the right breast

1. What BI-RADS classification should be used here?
2. What is the most likely pathology based on the imaging?
3. What is the next best imaging test?
4. What is the relevance of calcifications suspicious for DCIS outside of the tumor?
5. Do you have any recommendations for follow-up, other than normal mammography?
IDC plus DCIS with EIC 1761
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic

Right CC spot magnification view shows microcalcifications both within the tumor and outside extending anteriorly toward the nipple.
Ultrasound shows “irregular mass” with “angular margins,” containing reflective echoes consistent with microcalcifications.
Ultrasound—another area closer to the nipple shows a “dilated duct” containing microcalcifications.
Answers
1. BI-RADS 4 or 5 can be given depending on your certainty. It is extremely unlikely to be a benign finding, so a BI-RADS 5 may be the best fit. This is not a screening exam; therefore, BI-RADS 0 should not be used. If it was a screening exam, then a BI-RADS 0 would be appropriate, along with recommendations for a diagnostic workup to include spot magnification views and targeted ultrasound.
2. DCIS masses can look like this, but are more likely to be noncalcified and circumscribed. Invasive lobular cancer can present like this, but it is extremely rare. This is much more of a typical situation where there is both DCIS and invasive cancer.
3. Ultrasound should be the first test to validate the presence of a mass, which can then be used to target for biopsy. For extent of DCIS, MRI is the best test, but expensive, and may over-estimate the disease, as it is often associated with proliferative change, especially in pre-menopausal women. There is currently no evidence that preoperative MRI improves the eventual outcome of the patient, but it may be helpful to map the disease for the surgeons.
4. DCIS is commonly found within tumors, but when seen outside it takes on a serious connotation. The disease outside of the index cancer is known as extensive intraductal component (EIC). This needs measuring and the distance from the primary tumor noting on the report. It has a significant impact on the local recurrence rate, even with a boost during radiation therapy. Some patients have a mastectomy to reduce this chance of recurrent disease.
5. Recurrent disease is likely to involve calcifications; therefore, ensure that all calcifications have been adequately removed at surgery. Some centers perform spot magnification views prior to radiation treatment to ensure there is no residual DCIS.
Suggested Readings
Schouten van der Velden AP, Boetes C, Bult P, Wobbes T. Magnetic resonance imaging in size assessment of invasive breast carcinoma with an extensive intraductal component. BMC Med Imaging. 2009;9(9):5.
Van Goethem M, Schelfout K, Kersschot E, et al. MR mammography is useful in the preoperative locoregional staging of breast carcinomas with extensive intraductal component. Eur J Radiol. 2007;62(2):273-282.
Yiu CC, Loo WT, Lam CK, Chow LW. Presence of extensive intraductal component in patients undergoing breast conservative surgery predicts presence of residual disease in subsequent completion mastectomy. Chin Med J (Engl). 2009;122(8):900-905.
High-risk patient with diffuse pain in the left lateral inferior breast
1. What could be the next step after a normal diagnostic mammogram in a high-risk patient?
2. If spot compression views and ultrasound are negative, what is the next step?
3. What is the appropriate scenario to order problem-solving MRI?
4. What is the finding of the breast MRI?
5. What is the consequence and next step after the MRI?
Invasive ductal carcinoma in the left breast 1304
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
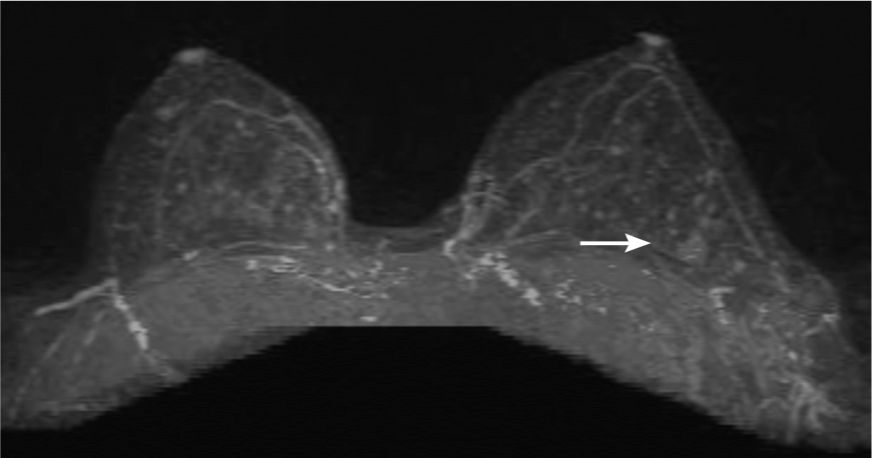
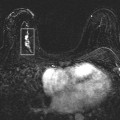
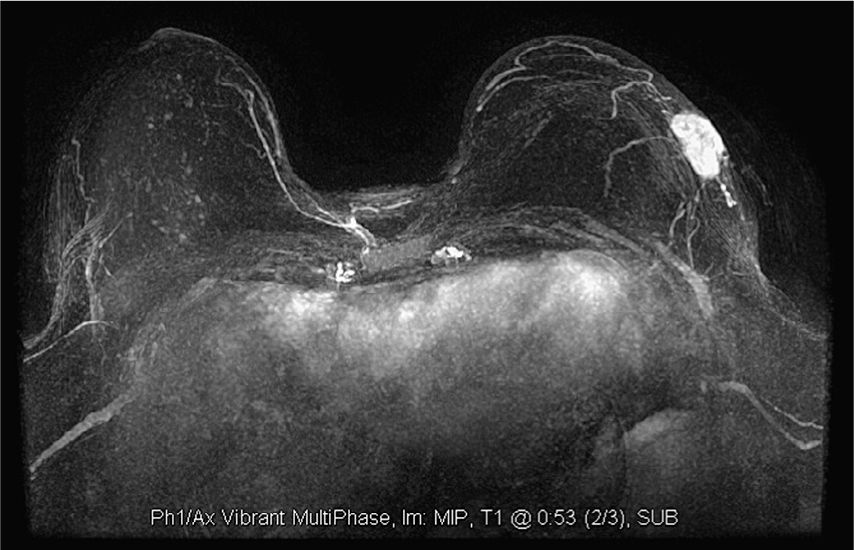
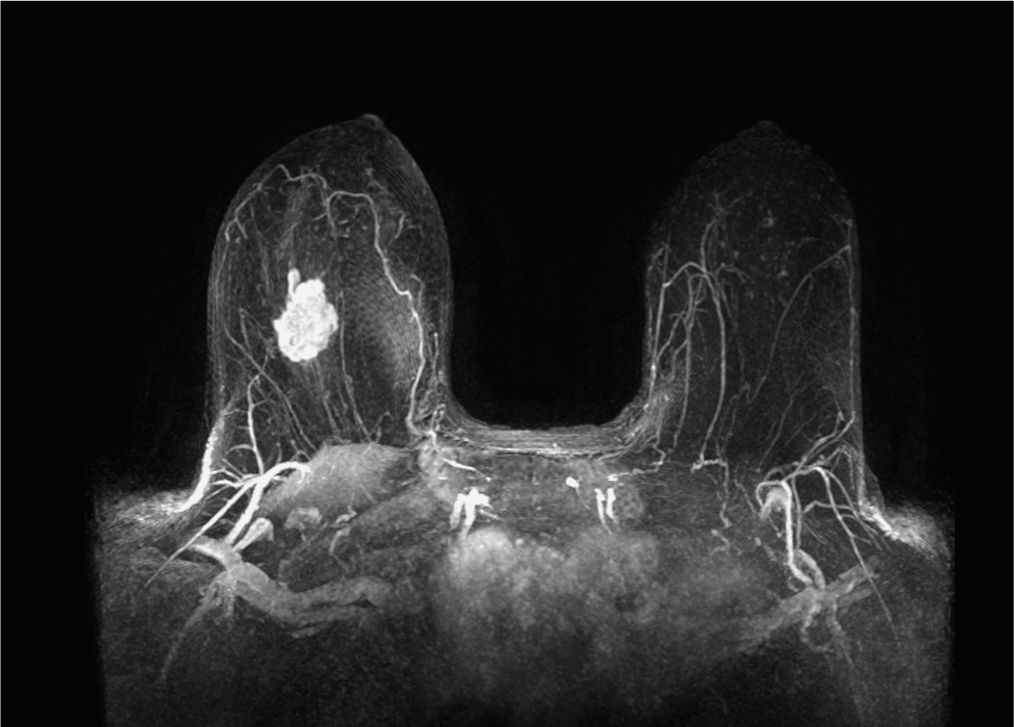
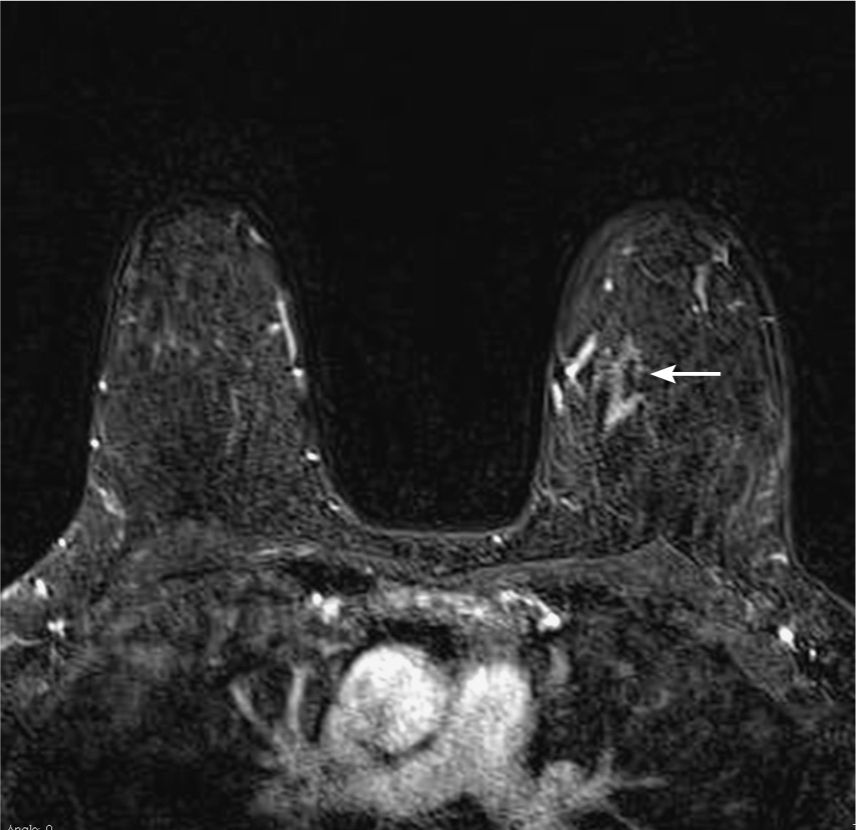
MRI post contrast Maximum Intensity Projection (MIP) demonstrates a small area of suspicious enhancement within the posterior left breast.

MRI after IV contrast with subtraction technique demonstrates focal area of enhancement left lateral posterior breast.
Second look gray-scale ultrasound image demonstrating corresponding “angular” mass.
Answers
1. Ultrasound, in general, would be the next step directed to the area of pain felt by the patient. However, if patient has a high-risk background, MRI as a problem-solving modality can also be considered.
2. This is a common scenario that patient feels a lump, or has some pain, and mammogram or ultrasound is unremarkable. It is not unreasonable to send patient with BI-RADS 1 (negative) assessment back to the referring physician and add a statement that “further assessment of the pain/lump should be based on clinical grounds.” That basically means that if the pain/mass is highly suspicious to the clinician, it might still be necessary for the clinician to perform a non image guided biopsy based on palpation. MRI is also an option but should be used wisely. It cannot be used in every patient in that scenario.
3. Problem-solving MRI can be helpful but should be used wisely. In particular, it should not be used to characterize a lesion based on ultrasound, and/or mammographic morphological criterion is suspicious and needs biopsy. That means it would need biopsy, regardless of the finding on MRI. In this particular case, MRI was helpful, since it is a symptomatic high-risk patient with very dense tissue, and indeed abnormality was found.
4. Noted is a mass in the left posterior superior breast, about 7 mm in diameter.
5. Since the lesion is very far back in the left breast near the chest wall, second look ultrasound is recommended as next step. MRI-guided biopsy would be technically very difficult, if not impossible. If ultrasound does not show corresponding lesion, MRI-guided biopsy or at least needle localization or marking of the lesion with clip is recommended to guide surgical excision.
Suggested Readings
Abe H, Schmidt RA, Shah RN, et al. MR-directed (“Second-Look”) ultrasound examination for breast lesions detected initially on MRI: MR and sonographic findings. AJR Am J Roentgenol. 2010;194(2):370-377.
Moy L, Elias K, Patel V, et al. Is breast MRI helpful in the evaluation of inconclusive mammographic findings? AJR Am J Roentgenol. 2009;193(4):986-993.
Yau EJ, Gutierrez RL, DeMartini WB, Eby PR, Peacock S, Lehman CD. The utility of breast MRI as a problem-solving tool. Breast J. 2011;17(3):273-280.
Palpable lump in a breast-feeding postpartum woman
1. What BI-RADS classification should be used here?
2. In a lactating woman, what is the differential diagnosis?
3. If this patient was presenting to you for the first time, which imaging modality is your first choice?
4. What BI-RADS descriptors would you apply to this lesion?
5. What is the best staging test for this patient?
Breast cancer in a lactating woman 1754
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
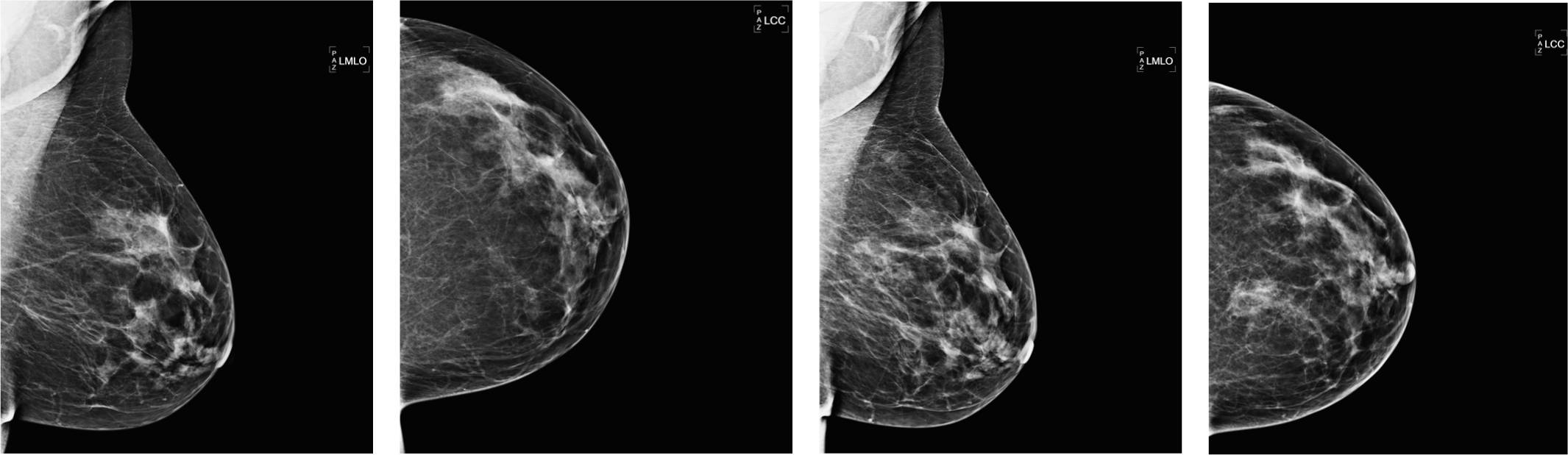
LCC spot magnification—minimal change seen. There is some distortion, but the mass is completely invisible because of lack of contrast. Some microcalcifications are also seen.
Another lactating patient showing what normal breast tissue can look like when lactating. Note the relatively bright glandular tissue with few features.
Another lactating patient showing prominent dilated milk filled ducts.
Answers
1. BI-RADS 4 or 5 can be used here based on the highly suspicious ultrasound. The mammogram is not particularly helpful, except from excluding associated DCIS microcalcifications.
2. All of the above are correct, as they can all present with a noncalcified mass in a lactating woman.
3. A nonionizing examination is the modality of choice in a young woman. This can be challenging in a woman who is lactating, but less so than in a pregnant patient, prepartum. If you see a suspicious abnormality, then mammography is warranted, as high-grade IDC can present first with microcalcifications in otherwise dense breasts. MRI can be reserved for challenging cases or for staging.
4. This is a suspicious lesion and suspicious BI-RADS descriptors should be used such as “irregular mass” and “angulated margins.” It is taller than it is wide, which BI-RADS describes as “nonparallel” contrary to a benign lesion that is “parallel” to the skin.
5. MRI is the best (nonionizing radiation) exam. It may have decreased sensitivity because of the hormonal change related to postpartum. PEM and BSGI could be used to detect more than one lesion in the breast, but there is currently a significant radiation dose from the isotope used. PET/CT can be used if the lesion is large and there is evidence on nodal spread.
Suggested Readings
Espinosa LA, Daniel BL, Vidarsson L, Zakhour M, Ikeda DM, Herfkens RJ. The lactating breast: contrast-enhanced MR imaging of normal tissue and cancer. Radiology. 2005;237(2):429-436.
Sabate JM, Clotet M, Torrubia S, et al. Radiologic evaluation of breast disorders related to pregnancy and lactation. Radiographics. 2007;27(Suppl 1):S101-S124.
Saglam A, Can B. Coexistence of lactating adenoma and invasive ductal adenocarcinoma of the breast in a pregnant woman. J Clin Pathol. 2005;58(1):87-89.
Patient with new abnormality on screening exam: MLO and CC view
1. What is the next step?
2. What is the appropriate BI-RADS classification?
3. What is the appropriate description of the mammogram abnormality?
4. What is the differential diagnosis of this new mass based on mammogram?
5. If the finding is stable since several years on standard mammogram, what is the assessment?
Invasive ductal carcinoma 1306
Diagnostic mammogram of right spot compression MLO view demonstrating small mass.
Diagnostic mammogram of right spot compression CC view demonstrating small mass.
Gray-scale ultrasound demonstrating small corresponding “hypoechoic mass” with “irregular” shape with thick echogenic halo and “indistinct” margin.
Answers
1. Next step is diagnostic workup with spot compression views.
2. BI-RADS 0 incomplete exam—patient needs to be recalled.
3. This is a finding of a small mass with partially obscured margin and of equal density to the surrounding tissue and of “irregular” shape and “indistinct” margin.
4. The finding is indeterminate and could represent inflamed cyst, hematoma, or malignancy, which could include invasive ductal carcinoma, DCIS, and invasive lobular carcinoma.
5. If the finding is stable for more than 2 years on standard screening mammogram, it can be called BI-RADS 2. The finding is not specific and could also represent benign finding as discussed in question 4, for example, a complicated cyst. The presence of “irregular” shape and “indistinct” margin is not appreciated on standard views. In this particular case, the appearance on spot compression views and on the ultrasound makes a difference and raises concern.
Suggested Reading
D’Orsi CJ, Bassett LW, Berg WA, et al. Breast Imaging Reporting and Data System: ACR BI-RADS–Mammography. 4th ed. Reston, VA: American College of Radiology; 2003.
Palpable finding in the right breast
1. What BI-RADS classification should be used here?
2. What is the most likely pathology based on the imaging?
3. What is the next best imaging test?
4. What type of biopsy would you recommend?
5. If phyllodes tumor is found on biopsy, what is the appropriate management?
Atypical fibroadenoma 1745
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
Right MLO.
Right lateromedial exam. The mass was medial in the breast, so a LM exam is the preferred projection. “Lobulated circumscribed mass.”
Answers
1. The ultrasound features are suspicious, in that it is an “irregular mass” with “microlobulated” margins, and a “heterogeneous echo pattern.”
2. Strictly, all of the answers could be correct, as they all can appear with similar findings. The most likely finding in a 29-year-old woman is fibroadenoma or phyllodes tumor, and it is the concern about the latter that prompts biopsy.
3. All of the above have been performed before in this situation. MRI is expensive and likely to show an enhancing mass, which will not affect the outcome. Elastography may show some tissue stiffness, but in younger women, fibroadenomas often have a more cellular component and are therefore softer than fibroadenomas in older patients. In view of the suspicious imaging, biopsy needs to be performed. Mammography can be considered, especially with findings that are not definitely characteristic of a fibroadenoma.
4. If it is visible on ultrasound, then the best way to do is a biopsy. If the lesion is palpable, some surgeons may prefer to do the biopsy themselves, but ultrasound should be used to confirm that the biopsy is sampling the right parts of the mass.
5. Phyllodes tumors need to be excised with a good margin, as they have a high chance of local recurrence but do not metastasize. Fibroepithelial lesions are a type of fibroadenoma variant that has been recognized, which needs surgical excision, to ensure that the mass has been adequately sampled.
Suggested Readings
Chung A, Scharre K, Wilson M. Intraductal fibroadenomatosis: an unusual variant of fibroadenoma. Breast J. 2008;14(2):193-195.
Sklair-Levy M, Sella T, Alweiss T, Craciun I, Libson E, Mally B. Incidence and management of complex fibroadenomas. AJR Am J Roentgenol. 2008;190(1):214-218.
Thein KY, Trishna SR, Reynolds V. Benign and malignant breast lesions mimicking each other: imaging-histopathologic correlation. Cancer Imaging. 2011;11(Spec No A):S180.
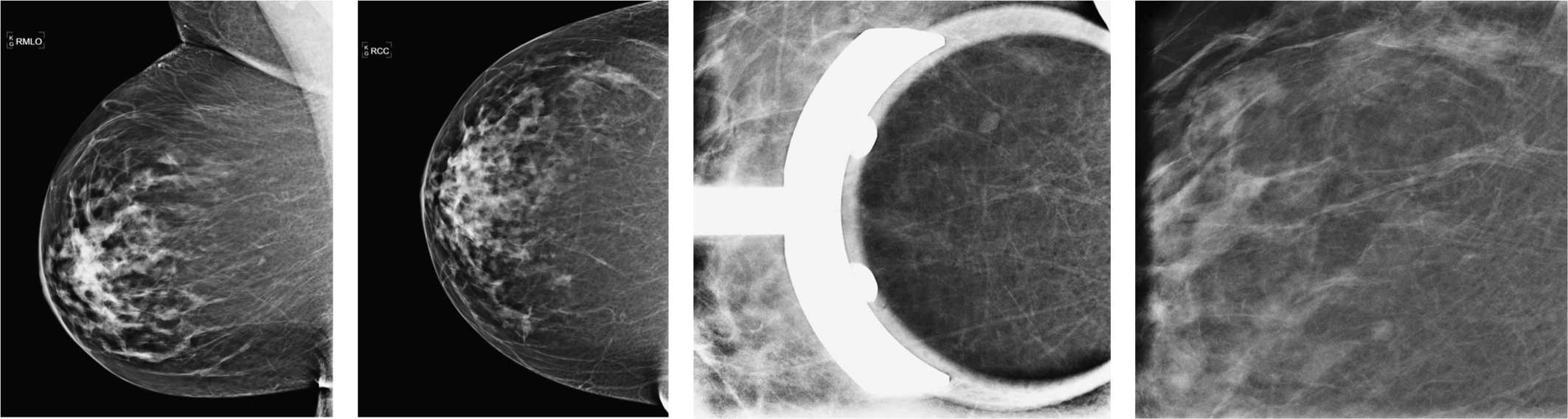
Prior breast cancer on the right breast: surveillance mammograms
1. What BI-RADS classification should be used here?
2. What is the most likely pathology based on the imaging?
3. What type of implant causes calcified capsules?
4. What is the best examination for looking at implant integrity?
5. What is the name used for an intracapsular rupture of an implant on MRI?
Calcified collapsed implants in patient postlumpectomy 1742
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
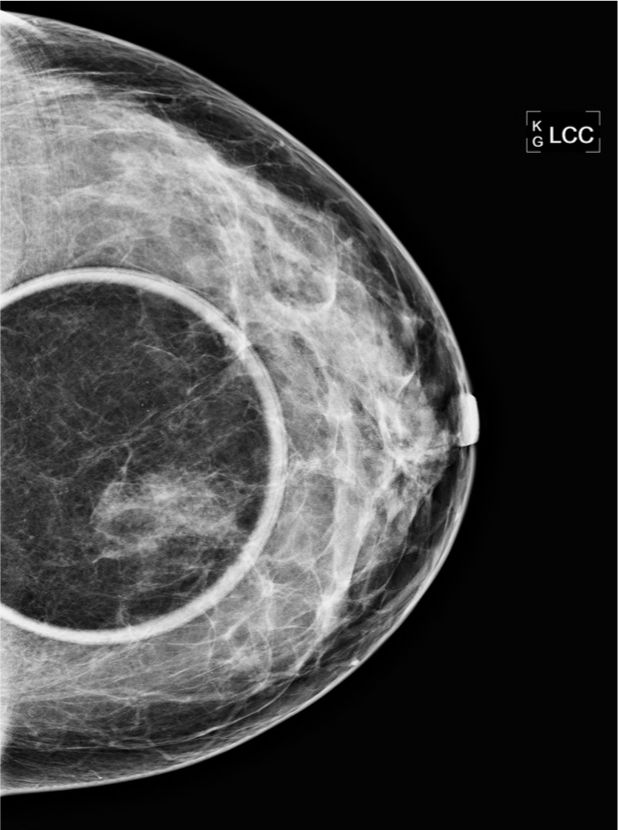
Right CC.
Another case—left MLO shows almost identical features. The calcification is coarse and “popcorn” like, but very extensive in the retro-pectoral space.
Answers
1. Whether screening or diagnostic, these findings are characteristically benign and therefore BI-RADS 2.
2. These are the appearances of collapsed calcified implant capsules following explantation of silicone pre-pectoral implants. Fat grafting gives changes similar to either lipomas or to fat necrosis, depending on how the body responds to the treatment. Injected silicone looks very dense and different to this type of density. Guinea worms look like irregular coils of calcium. Found when an adult dracunculus parasite dies, it is usually small in caliber, but can occasionally be very large. They do not tend to be seen bilaterally or symmetrically.
3. There is some evidence for calcified capsule formation with saline implants, but this is rare. Silicone leaking across the implant causes an intense inflammatory reaction, which is prone to calcifying. Capsular calcification is normally seen in the pre-pectoral type of implant, normally from a cosmetic surgery in the past. Saline implants are preferred for the retro-pectoral space, as they do not have any complications from rupture, unlike silicone gel. Trilucent implants were used in Europe for a time, before they were banned from use. They were relatively easy to see through, causing less obstruction of normal breast tissue.
4. MRI is the best exam for implant integrity, as you can see the whole of the implant and the capsule, as well as performing silicone dark and silicone bright sequences. Ultrasound is good for a palpable finding (usually on the anterior margin of the implant). Diagnostic mammograms can show complications of capsules, and contour abnormalities may suggest weakening of the implant wall, but is not the best test.
5. The term used is Linguine sign, of the collapsed inner capsule within the main capsule. Not to be confused with other delicious forms of Italian pasta.
Suggested Readings
Dershaw DD, Chaglassian TA. Mammography after prosthesis placement for augmentation or reconstructive mammoplasty. Radiology. 1989;170(1, Pt 1):69-74.
Peters W, Pritzker K, Smith D, et al. Capsular calcification associated with silicone breast implants: incidence, determinants, and characterization. Ann Plast Surg. 1998;41(4):348-360.
Peters W, Smith D, Fornasier V, Lugowski S, Ibanez D.
An outcome analysis of 100 women after explantation of silicone gel breast implants. Ann Plast Surg. 1997;39(1):
9-19.
Palpable abnormality in the left breast: 73-year-old patient
1. What is the first step of workup of palpable abnormality in a 73-year-old patient?
2. What would be the workup if patient had prior normal screening mammogram 7 months ago?
3. What would be the workup if there was a normal mammogram 3 months ago?
4. What is the most likely morphological appearance of low-grade DCIS?
5. What is the likelihood of the presence of malignancy in case of normal imaging despite the presence of palpable abnormality?
Low-grade DCIS 733
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic

Spot compression left MLO view with BB marker on palpable abnormality demonstrating small mass.
Spot compression left CC view with BB marker on palpable abnormality demonstrating small mass.
Gray-scale ultrasound image of palpable abnormality demonstrates small hypoechoic mass.
Answers
1. Workup of patients in that age group includes diagnostic mammogram with spot compression views with BB marker on the palpable finding and then ultrasound.
2. If patient had recent mammogram more than 6 months ago, in general, repeat mammogram is recommended. Remember, 6 months is the time frame used to follow BI-RADS 3 findings. There is no need to repeat mammogram at this point at the nonsymptomatic right side. This can be done when patient is due for next screening mammogram.
3. In general, if there is a normal mammogram available, performed less than 6 months ago, there is no need to repeat mammogram and it is not unreasonable to perform an ultrasound first. If the ultrasound is negative and the palpable abnormality is very questionable, it would be reasonable to stop here. However, this depends also on the confidence of the assessment of the last mammogram, performed less than 6 months ago. If breast parenchyma was very dense and therefore limits the assessment, it would not be unreasonable to repeat the mammogram, even if it was called BI-RADS 1 (“negative”) less than 6 months ago. Remember at that time no spot compression views were obtained, since it was a screening mammogram.
4. In this case, a mass turned out to be low-grade DCIS, which is rather uncommon. In general, low-grade DCIS presents as a group of calcifications that are usually rather “amorphous” or “round and oval” and less likely “pleomorphic.”
5. There are not many studies available looking at this issue. The study by Gumus et al. (2012) looked over a 12-year period of time at 251 patients with palpable abnormalities and normal imaging and found only 1.2% of the patients having malignancy (false-negative mammogram). However, the false-negative rate will also depend on the density of the breast parenchyma. It can be suspected that it will be even lower in “fatty replaced breast” versus in “extremely dense breast.”
Suggested Readings
DiPiro PJ, Meyer JE, Denison CM, Frenna TH, Harvey SC, Smith DN. Image-guided core breast biopsy of ductal carcinoma in situ presenting as a non-calcified abnormality. Eur J Radiol. 1999;30(3):231-236.
Gumus H, Gumus M, Mills P, et al. Clinically palpable breast abnormalities with normal imaging: is clinically guided biopsy still required? Clin Radiol. 2012;67(5):437-440.
Prior left mastectomy and reconstruction for triple-negative breast cancer
1. What BI-RADS classification should be used here?
2. Which is the best modality to assess implants?
3. Which is the best modality to assess a palpable finding associated with an implant?
4. What further tests do you recommend at this stage?
5. If a patient has an implant reconstruction as part of a mastectomy, what is the initial implant used?
Palpable recurrence on mastectomy site with reconstruction 1580
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
Ultrasound—relationship with implant and skin—technique using gentle pressure with standoff gel.

MRI—T1 postcontrast, unsubtracted exam.
Subtracted MIP image in axial plane.
Answers
1. You can either use BI-RADS 4 straight off or wait until you have done the ultrasound and give a combined BI-RADS assessment. There is a vague density seen on the left ML, but best seen in this instance on the CC view. Implant-displaced views cannot be performed because there is no “breast tissue,” as this implant was placed following a tissue expander.
2. MRI is the only modality that allows for full assessment of implants. Using silicone suppression sequences allows for distinguishing between cysts and silicone granulomas. MRI can see the posterior aspect of the implant, no accessible with ultrasound.
3. Ultrasound should be the first modality to use, as no ionizing radiation, and can be targeted easily, and correlated with the physical findings. MRI overall is the best modality for assessing implants themselves.
4. If there is no biochemical evidence of metastatic deposits, then PET or bone scans may not be needed; however, some centers have these tests as local protocol for any patient with a breast cancer recurrence. MRI is the most helpful initial test to determine the extent of the recurrence and check on skin coverage for surgical planning, which is usually a completion mastectomy in a patient who has had breast conservation. This patient, however, has already had a mastectomy with tissue expanders and followed by implant reconstruction.
5. The patient has a special type of implant inserted, which is a tissue expander. This type of implant has a saline bag and tubing with a valve, which is gradually expanded over a period of weeks to stretch the skin. Once the skin has reached the required volume, the expander is switched out for a conventional implant.
Suggested Readings
Destounis S, Morgan R, Arieno A, Seifert P, Somerville P,
Murphy P. A review of breast imaging following mastectomy with or without reconstruction in an outpatient community center. Breast Cancer. 2011;18(4):259-267.
Patterson SG, Teller P, Iyengar R, et al. Locoregional recurrence after mastectomy with immediate transverse rectus abdominis myocutaneous (TRAM) flap reconstruction. Ann Surg Oncol. 2012;19(8):2679-2684.
Sim YT, Litherland JC. The use of imaging in patients post breast reconstruction. Clin Radiol. 2012;67(2):128-133.
45-year-old female with new 3–4 mm “focal asymmetry” on screening mammogram, spot compression views (the two figures on the right) confirm the presence of 3–4 mm mass
1. What is the difference between an asymmetry and a mass?
2. What is the workup of an asymmetry on a first screening mammogram?
3. If there is a finding on ultrasound—which correlates to the mammogram—what is the next step?
4. What is the next step in regard to the “focal asymmetry” if it is new?
5. What would be a way to correlate an ultrasound with a mammogram finding, if in doubt?
Pseudoangiomatous stromal hyperplasia 321
Case ranking/difficulty: ![]()
![]() Category: Screening
Category: Screening
Mammogram of right spot compression CC view confirming small 3–4 mm mass on the right lateral breast.
Ultrasound directed to the right breast demonstrating small hypoechoic mass of corresponding size in the central breast.
Diagnostic mammogram, right MLO view demonstrates iodine contrast (black arrow) and mass (white arrow).
Answers
1. BI-RADS differentiates between “mass” and “asymmetry.” Mass is always seen in two projections and has a clear border and conspicuity which is visible on both projections. An asymmetry is sometimes seen only in one projection, but can be seen on two projections as well and is less defined. A “focal asymmetry” is differentiated from a larger “global asymmetry” by size alone. A global asymmetry can involve an entire quadrant and is in general more likely to represent normal tissue.
2. The patient needs to be recalled for a diagnostic work up including spot compression views CC and MLO. Then ultrasound should be performed. It is also important to confirm that there is no palpable abnormality in that area. In the absence of an underlying palpable abnormality, the finding can be followed in 6 months and classified as “probably benign” if ultrasound is normal.
3. The ultrasound finding has to be a simple cyst to justify calling this a benign finding and return the patient to screening. Any other finding should be biopsied, since this is a new mass on mammogram. An exception could be cluster of small cysts and follow-up in 6 months could be performed. However, if there is any doubt, biopsy would be preferred in case of a new mass on mammogram.
4. If the finding is a new asymmetry and has not any corresponding finding on ultrasound, it has to be biopsied or excised—BI-RADS 4 (suspicious). First step would be to attempt stereotactic biopsy. If finding is not visible on the stereotactic biopsy table, needle localization and subsequent surgical excision can be performed.
5. One way is to place a BB on the ultrasound finding and perform a tangential view to see if it correlates. Other methods would be to aspirate the finding, in case it is a cyst, and repeat mammogram to see if the mammogram finding is gone. Other options could be to place a Homer needle (removable needle localization) and repeat mammogram, or to inject small trace of air or iodine contrast and repeat mammogram. This can be helpful if there are multiple small findings or if the findings are so small that cyst aspiration is technically difficult.
Suggested Readings
Ellis RL. Sonographic confirmation of a mammographically detected breast lesion. AJR Am J Roentgenol. 2011;196(1):225-256.
Sickles EA. The spectrum of breast asymmetries: imaging features, work-up, management. Radiol Clin North Am. 2007;45(5):765-771, v.
Palpable finding in the right breast
1. What BI-RADS classification should be used here?
2. What is the next imaging test?
3. If calcification is seen with this finding, what is the likely pathology?
4. This lesion is palpable. What type of biopsy should be performed?
5. Based on the imaging, what is the likely pathology on core biopsy?
Cancer partially obscured by dense breast tissue 1578
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic

Ultrasound showing an “irregular” mass with “microlobulated” superior “margins.”
Right breast sagittal subtracted thin MIP.
Axial subtracted MIP showing 4.3-cm solitary enhancing mass.
Answers
1. Either BI-RADS 4 or 5 is a valid answer. Even though you are not supplied with spot or spot magnification views, you get the impression that this is quite a large lesion.
2. Ideally, you want to maximize the information you can get from mammography before proceeding to other tests. Lateral projection and spot or spot magnification films should be used to get a better idea of the extent of this lesion. If available, tomosynthesis may help to evaluate the mass margins. Ultrasound is the next examination when this is done. In some patients with very dense breasts, it is not possible to adequately measure the extent of disease, and MRI may be the more accurate modality.
3. In the setting of a “spiculate mass,” there are several possibilities, which include benign conditions such as fat necrosis (where the calcification is usually easier to distinguish as appears dystrophic), radial scar, or complex sclerosing lesion, which can be associated with DCIS in 20%. Lobular cancer may be associated with amorphous calcifications. A classic “spiculate mass” with “fine linear pleomorphic” calcifications is usually a high-grade invasive ductal cancer with high-grade DCIS.
4. Although palpation guidance can be used, ultrasound guidance allows you to confirm that the needle passes through different areas of the mass, and gets the most representative samples of the tumor. If the lesion is not clearly seen on ultrasound, or there are confounding appearances on ultrasound, such that your confidence for sampling the mass accurately is low, then consider stereotactic core biopsy.
5. The appearances of a mass with distortion are more likely to be a feature of invasive ductal carcinoma. Invasive lobular cancer may present as a mass (better seen on the CC) but is more common as subtle distortion, a slowly shrinking breast, or even with no mammographic findings, but obvious palpation abnormalities or ultrasound changes.
Suggested Reading
Huynh PT, Jarolimek AM, Daye S. The false-negative mammogram. Radiographics. 2006;18(5):1137-1154; quiz 1243-1244.
Bilateral masses in screening patient: what is the consequence?
1. What are the findings on the screening mammogram?
2. What is the most likely etiology?
3. What is the next step after screening mammogram of asymptomatic patient?
4. What is the appropriate BI-RADS assessment?
5. What is the likelihood of malignancy in this case? (best answer)
Bilateral benign masses 1625
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
On B-mode ultrasound, there are scattered benign-appearing, well-circumscribed masses noted in the right breast.
On B-mode ultrasound, there are scattered benign-appearing, well-circumscribed masses noted in the left breast.
Answers
1. Noted are bilateral scattered benign-appearing masses.
2. Most likely bilateral masses will be due to the presence of bilateral fibrocystic changes (cysts) or less likely due to bilateral fibroadenomas.
3. In general, there is no need for further workup, since it has been shown that the likelihood of malignancy is not higher than in normal screening population. In this particular case, the patient felt multiple lumps and therefore ultrasound was performed.
4. The appropriate classification is BI-RADS 2 (benign) and next screening exam is due in 1 year.
5. Among 1440 patients with bilateral scattered masses, only 2 interval cancers were found based on a study by Leung and Sickles (2000), which results in an incidence rate of malignancy of 0.14% that is lower than the age-matched ultrasound incident cancer rate of 0.24%.
Suggested Reading
Leung JW, Sickles EA. Multiple bilateral masses detected on screening mammography: assessment of need for recall imaging. AJR Am J Roentgenol. 2000;175(1):23-29.
Screening exam: prior films on left
1. What is the pertinent finding?
2. What malignancy can present in that way?
3. Would MRI, in this case, help to eliminate biopsy?
4. Does it make a difference if there were no old images available?
5. Why is ultrasound necessary for workup in this case?
Developing “focal asymmetry” 762
Case ranking/difficulty: ![]()
![]() Category: Screening
Category: Screening
Diagnostic mammogram, left CC spot compression view, demonstrating “focal asymmetry.”
MRI, T1-weighted sequence after IV contrast with subtraction technique, demonstrating “non–mass-like” area of enhancement.
Answers
1. Noted is the development of subtle “focal asymmetry” in the left superior breast, posterior depth.
2. All malignancies can present as “focal asymmetry.” Pseudoangiomatous stromal hyperplasia (PASH) is not a malignant lesion but can present as focal asymmetry.
3. In general, the negative predictive value of breast MRI is high, close to 100% but not exactly 100%. Therefore, the mainstream opinion is to biopsy any suspicious abnormality seen on mammogram—including developing “focal asymmetry.” However, there is a recent shift and there are more publications suggesting that negative MRI might eliminate the need for biopsy. The article from Europe in 2011, for example, suggests that this is feasible.
4. If this was a “focal asymmetry” on a baseline mammogram, the workup would be the same. But if there was no underlying suspicious morphology, the finding could be classified as BI-RADS 3 and could be followed in 6 months, and again 6 months later and then 1 year later to have a monitoring period of 2 years in total.
5. In case of a new asymmetric density, it is necessary to determine if there is any corresponding abnormality that could be biopsied under ultrasound guidance. In case of an asymmetric density on a baseline mammogram, ultrasound is necessary to further exclude corresponding abnormality. If ultrasound is normal, it can be followed in 6 months.
Suggested Readings
Dorrius MD, Pijnappel RM, Sijens PE, van der Weide MC, Oudkerk M. The negative predictive value of breast magnetic resonance imaging in noncalcified BI-RADS 3 lesions. Eur J Radiol. 2012;81(2):209-213.
Leung JW, Sickles EA. Developing asymmetry identified on mammography: correlation with imaging outcome and pathologic findings. AJR Am J Roentgenol. 2007;188(3):667-675.
Piccoli CW, Feig SA, Palazzo JP. Developing asymmetric breast tissue. Radiology. 1999;211(1):111-117.
Bilateral calcifications on first screening exam
1. What would be the description of these calcifications on a screening exam?
2. What is the consequence these descriptors?
3. What other benign proliferative changes can cause pleomorphic calcifications?
4. What is the consequence of the presence of pleomorphic calcifications on diagnostic exam?
5. Pathology showed fibrocystic changes and sclerosing adenosis on the right side (calcifications seen in specimen) and DCIS on the left side. What is the management?
Bilateral suspicious calcifications 761
Case ranking/difficulty: ![]()
![]() Category: Diagnostic
Category: Diagnostic
Right ML magnification view with additional electronic magnification demonstrating group of “pleomorphic” calcifications.

Right CC magnification view with additional electronic magnification demonstrating group of “pleomorphic” calcifications.
Left ML magnification view with additional electronic magnification demonstrating group of “pleomorphic” calcifications.
Left CC magnification view with additional electronic magnification demonstrating group of “pleomorphic” calcifications.
Answers
1. Screening mammogram demonstrates bilateral scattered benign calcifications and also group of indeterminate calcifications in the right inferior medial breast and left superior lateral breast. On screening mammogram, calcifications should not be further characterized. All indeterminate calcifications need to be magnified and then can be further described with appropriate BI-RADS descriptors.
2. Patient needs to be recalled for additional magnification views bilaterally.
3. Sclerosing adenosis and early calcifications in a fibroadenoma can present as “pleomorphic” calcifications.
4. “Pleomorphic” calcifications indicate the need for biopsy.
5. Both findings are concordant. Patient needs lumpectomy of left breast and 6-month follow-up mammogram of right side with magnification views. A preoperative MRI would also be helpful. Any benign biopsy in general will be followed in 6 months. Any follow-up of calcifications has, by definition, to include magnification ML and CC views.
The same principle applies to follow-up of “focal asymmetries” or “masses”; it should always include spot compression views. You want to have the best information to follow something that is considered BI-RADS 3 or was recently biopsied to look for change.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree