Pericardial Disease
QUESTIONS
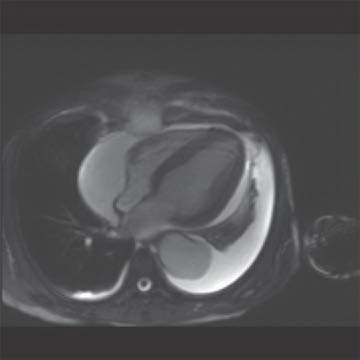
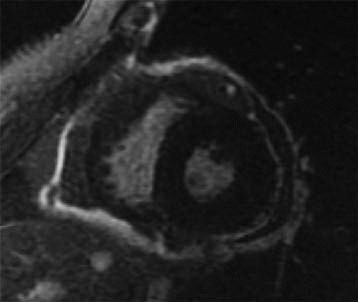
1 The patient presents with dyspnea and has cardiomegaly based on a radiograph (not shown). Which of the following cardiac findings shown on the four-chamber balanced steady-state image?
|
A. Atrial septal defect
B. Enlarged left ventricle
C. Mitral valve prolapse
D. Pericardial effusion
E. Pericarditis
View Answer
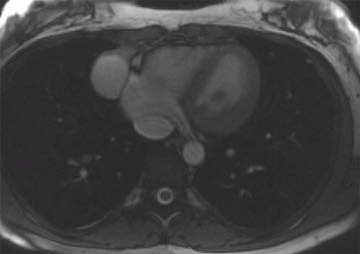
1 Answer D. The patient has a large pericardial effusion on the bright blood sequence. Normally, the pericardium is a thin sac composed of two layers enveloping the heart (an inner serous membrane and an outer fibrocollagenous layer). Normally, the pericardium contains 10 to 50 mL of an ultrafiltrate of plasma. If it contains a greater volume, it will cause a pericardial effusion.
References: Bogaert J, Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson 2009;11:14.
Roberts WC, Spray TL. Pericardial heart disease: a study of its causes, consequences, and morphologic features. Cardiovasc Clin 1976;7:11-65.
2 What contributes to MRI overestimating the pericardial thickness?
A. Chemical shift artifact at the fat fluid interface
B. Higher spatial resolution compared to CT
C. Lack of motion of the pericardial layers
D. Low temporal resolution
View Answer
2 Answer A. The pericardium normally measures up to 2 mm in systole and 1 mm in diastole; however, accurate measurement of the pericardium using MRI can be challenging. MRI has been shown to overestimate the pericardial thickness, which may be secondary to chemical shift artifact, spatial resolution limits, and motion of the pericardial layers.
References: Bogaert J, Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson 2009;11:14.
Sechtem U, Tscholakoff D, Higgins CB. MRI of the abnormal pericardium. AJR Am J Roentgenol 1986;147:245-252.
A. Constrictive pericarditis
B. Pericardial lipoma
C. Pericardial lymphoma
D. Pneumopericardium
View Answer
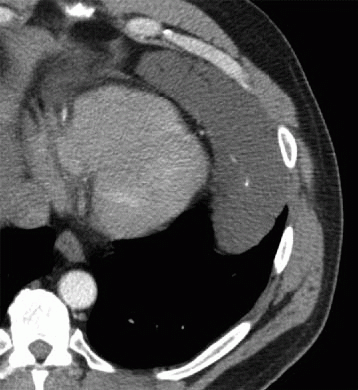
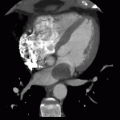
3 Answer B. Primary pericardial tumors are uncommon. Pericardial lipomas have been reported to account for up to 10% of all primary pericardial neoplasms. The mass is of fat attenuation and is well encapsulated. Tumors are usually detected incidentally and are usually asymptomatic. In symptomatic patients, the tumor may lead to compression of the cardiac chambers.
References: Steger CM. Intrapericardial giant lipoma displacing the heart. ISRN Cardiol 2011;2011:4. Article ID 243637. http://dx.doi.org/10.5402/2011/243637
Stoian I, et al. Rare tumors of the heart-angiosarcoma, pericardial lipoma, leiomyosarcoma, three case reports. J Med Life 2010;3(2):178-182. Published online 2010 May 25.
A. Calcifications
B. Serous pericardial effusion
C. Restrictive physiology
D. Systemic malignancy
View Answer
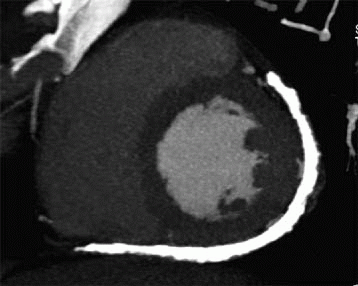
4 Answer A. The mass is low in density, septated, and contains calcifications. These features are most characteristic of a pericardial lymphangioma. There are no areas of nodularity or enhancement in the mass, indicating it is not due to a primary cardiac malignancy or metastatic disease. Pericardial lymphangiomas are uncommon primary tumors that may extend into the mediastinum and may compress cardiac or adjacent mediastinal structures leading to respiratory distress or altered cardiac function.
References: Shaheen F, Lone N. A rare case of pericardial lymphangioma causing tamponade: routine and dynamic MR findings. Eur J Radiol Extra 2009;69(1):e9-e10.
Zakaria RH, et al. Imaging of pericardial lymphangioma. Ann Pediatr Cardiol 2011;4(1):65-67. doi: 10.4103/0974-2069.79628.
A. Absent pericardium
B. Calcific pericarditis
C. Pericardial effusion
D. Pericardial metastasis
View Answer
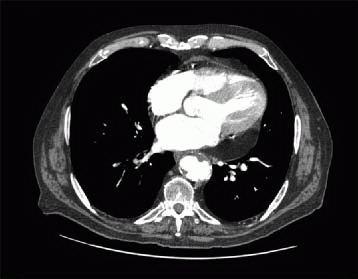
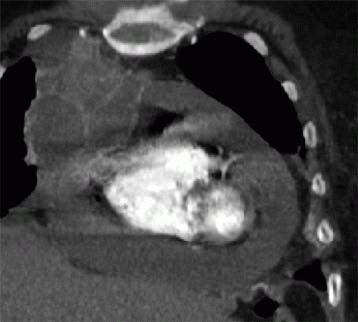
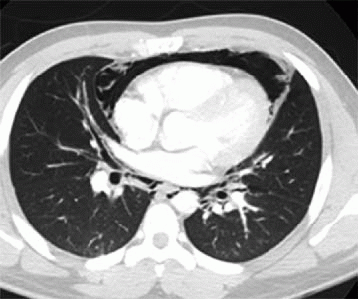
5a Answer B. The image shows the pericardium is thickened (measuring >4 mm) along the lateral and inferior wall of the heart and is densely calcified. These findings are compatible with calcific pericarditis. Calcific pericarditis can be secondary to prior inflammation, infection (tuberculosis), connective tissue disease, radiation therapy, or uremia. The finding of calcifications can be associated with constrictive physiology.
References: Macgregor JH, Chen JT, Chiles C, et al. The radiographic distinction between pericardial and myocardial calcifications. AJR Am J Roentgenol 1987;148(4):675-677.
Wang ZJ, Reddy GP, Gotway MB, et al. CT and MR imaging of pericardial disease. Radiographics 2003;23:S167-S180.
5b Constrictive pericarditis can cause which of the following changes?
A. Decreased right ventricular volume
B. Decreased IVC caliber
C. Normal-sized liver
D. Rightward displaced interventricular septum
View Answer
5b Answer A. Constrictive pericarditis can be associated with decrease in size of the right ventricle reduced right ventricular volume, dilation of the IVC and SVC, hepatomegaly, and ascites. The interventricular septum can be displaced toward the left ventricle or develop a sigmoid shape.
References: Higgins CB. Acquired heart disease. In: Higgins CB, Hricak H, Helms CA (eds.). Magnetic resonance imaging of the body. Philadelphia, PA: Lippincott-Raven, 1997:409-460.
Wang ZJ, Reddy GP, Gotway MB, et al. CT and MR imaging of pericardial disease. Radiographics 2003;23:S167-S180.
A. Dilated heart
B. Pericardial calcification
C. Separation of the epicardial and pericardial fat
D. Widening of the mediastinum
View Answer
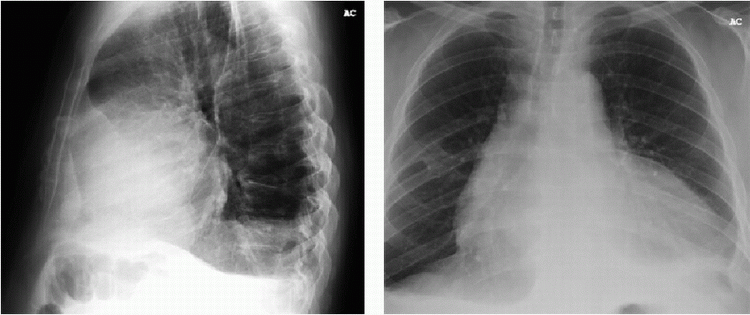
6 Answer C. The patient has a large pericardial effusion. Radiography is not sensitive for the diagnosis of a pericardial effusion large effusions can be identified using several radiographic findings. The effusion is best visualized on the lateral view and is outlined by the epicardial and pericardial fat (“oreo-cookie sign”). Other findings suggestive of a pericardial effusion include a dilated cardiac silhouette and widening of the subcarinal angle.
References: Chen JT, Putman CE, Hedlund LW, et al. Widening of the subcarinal angle by pericardial effusion. AJR Am J Roentgenol 1982;139(5):883-887.
Wang ZJ, Reddy GP, Gotway MB, et al. CT and MR imaging of pericardial disease. Radiographics 2003;23:S167-S180.
A. Compression of the cardiac chambers
B. Enhancement on postcontrast MR imaging
C. Intermediate signal on T1 images if it is simple
D. Most commonly located at the right cardiophrenic angle
E. Septations on T2 images
View Answer
7 Answer D. The image shows a mass at the right cardiophrenic angle that is most compatible with a pericardial cyst. Pericardial cysts are most commonly located at the right cardiophrenic angle, have increased T2 signal, lack septations, and have no enhancement. Pericardial cysts are formed during development of the pericardial sac and while most common at the right cardiophrenic angle can be located in the anterior and posterior mediastinum. Less commonly, pericardial cysts can cause compression or become infected.
References: Patel J, Park C, Michaels J, et al. Pericardial cyst: case reports and a literature review. Echocardiography 2004;21:269-272.
White CS. MR evaluation of the pericardium. Top Magn Reson Imaging 1995;7:258-266.
A. Calcific pericarditis
B. Constrictive pericarditis
C. Malignant pericardial effusion
D. Pericardial effusion
E. Pericardial lymphangioma
View Answer
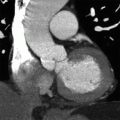
8 Answer C. The image shows a large pericardial effusion with septations and nodular enhancement of the pericardium, compatible with a malignant pericardial effusion. Irregular and nodular pericardial thickening and enlarged mediastinal lymph nodes increase the specificity when diagnosing a malignant pericardial effusion. Fluid-based sampling and cytology are used to confirm the diagnosis of a malignant pericardial effusion.
References: Rienmüller R, Gröll R, Lipton MJ. CT and MR imaging of pericardial disease. Radiol Clin North Am 2004;42:587-601.
Sun JS, Park KJ, Kang DK. CT findings in patients with pericardial effusion: differentiation of malignant and benign disease. AJR Am J Roentgenol 2010;194(6):W489-W494.
A. Aneurysmectomy
B. CABG
C. Pericardectomy
D. Radiation therapy
View Answer
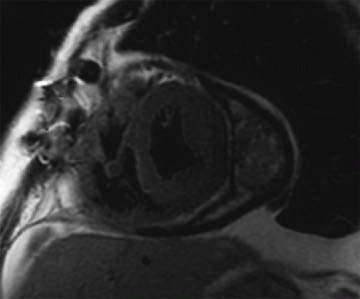
9 Answer C. The patient has a thickened and enhancing pericardium and a hematoma indicating underlying constrictive pericarditis. The patient underwent a pericardiectomy. A pericardiectomy can be performed via either a median sternotomy or anterolateral thoracotomy. A pericardiectomy is performed as definitive treatment for constrictive pericarditis. During the procedure, the pericardium is removed to the greatest extent possible. However, despite the procedural success, hemodynamics may not return to their baseline state.
References: Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases. Eur Soc Cardiol 2004;25(7):587-610.
Tiruvoipati R, Naid RD, Loubani M, et al. Surgical approach for pericardiectomy: a comparative study between median sternotomy and left anterolateral thoracotomy. Cardiovasc Thorac Surg 2003;2(3):322-326. doi: 10.1016/S1569-9293(03)00074-4.
A. Absent inflammation
B. Mild disease
C. Fatty proliferation
D. Increased neovascularization
View Answer
10 Answer D. The patient has pericarditis with a thickened pericardium and late gadolinium enhancement. The presence of late gadolinium enhancement in pericarditis is associated with increased inflammation, neovascularization, proliferation of fibroblasts, and granulation tissue indicating ongoing inflammation. Patients without late gadolinium enhancement but a thickened pericardium are more likely to have mild or absent inflammation.
References: Srichai MB. CMR imaging in constrictive pericarditis: is seeing believing? J Am Coll Cardiol Imaging 2011;4(11):1192-1194. doi: 10.1016/j.jcmg.2011.09.009.
Young PM, Glockner JF, Williamson EE. MR imaging findings in 76 consecutive surgically proven cases of pericardial disease with CT and pathologic correlation. Int J Cardiovasc Imaging 2012;28(5):1099-1109. [E-pub ahead of print].
11 What best describes the principle of ventricular independence as it relates to septal bounce?
A. Increased in volume of one ventricle causes a reduced volume in the opposite ventricle.
B. The bounce is decreased during inspiration.
C. A decrease in right ventricular pressure causes the shift toward the left ventricle.
D. Increased venous return has no impact on ventricular interdependence.
View Answer
11 Answer A. The principle of ventricular interdependence defines how an increase in volume of one ventricle causes a decreased volume in the opposite ventricle. The septal bounce is characterized by movement of the interventricular septum initially toward the left ventricle and subsequently away from the left ventricle during early diastole. During early diastole, since right ventricular filling occurs before left ventricular filling, the increased right ventricular volume will shift the septum toward the left. This will reverse as the left ventricle subsequently fills increased venous return, which occurs during inspiration, will increase the septal bounce.
References: Giorgi B, Mollet NR, Dymarkowski S, et al. Clinically suspected constrictive pericarditis: MR imaging assessment of ventricular septal motion and configuration in patients and healthy subjects. Radiology. 2003;228:417-424.
Walker CM, Chung JH, Reddy GP. Septal bounce. J Thorac Imaging 2012;27(1):w1. doi: 10.1097/RTI.0b013e31823fdfbd.
A. Atrioesophageal fistula
B. Fistula to the mediastinum
C. Pneumothorax
D. Pneumopericardium
E. Pneumoperitoneum
View Answer




12a Answer D. The patient has extensive pneumopericardium with air between the pericardium and right atrium and ventricle. Pneumopericardium can be secondary to trauma (blunt or penetrating), postoperative, infectious, or a fistula. If the air is extensive it can cause tamponade physiology.
References: Bejvan SM, Bejvan SM, Godwin JD. Pneumomediastinum: old signs and new signs. AJR Am J Roentgenol 1996;166(5):1041-1048.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree