FOOT AND ANKLE
THIRD EDITION
IMAGING OF THE
FOOT AND ANKLE
Editor
Thomas H. Berquist, M.D., F.A.C.R.
Professor of Diagnostic Radiology
Mayo Clinic College of Medicine
Rochester, Minnesota
Consultant in Diagnostic Radiology
Mayo Clinic in Florida
Jacksonville, Florida

Acquisitions Editor: Charles W. Mitchell
Product Manager: Ryan Shaw
Vendor Manager: Alicia Jackson
Senior Manufacturing Manager: Benjamin Rivera
Senior Marketing Manager: Angela Panetta
Design Coordinator: Joan Wendt
Production Service: MPS Limited, A Macmillan Company
© 2011 by LIPPINCOTT WILLIAMS & WILKINS, a WOLTERS KLUWER business
Two Commerce Square
2001 Market Street
Philadelphia, PA 19103 USA
LWW.com
All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form by any means, including photocopying, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright.
Printed in China
Library of Congress Cataloging-in-Publication Data
Imaging of the foot and ankle / editor, Thomas H. Berquist.—3rd ed.
p. ; cm.
Rev. ed. of: Radiology of the foot and ankle / editor, Thomas H. Berquist.
2nd ed. c2000.
Includes bibliographical references and index.
ISBN 978-1-60547-572-1 (alk. paper)
1. Foot—Imaging. 2. Ankle—Imaging. 3. Foot—Diseases—Diagnosis.
4. Ankle—Diseases—Diagnosis. I. Berquist, Thomas H. (Thomas Henry), 1945–
II. Radiology of the foot and ankle.
[DNLM: 1. Foot Diseases—diagnosis. 2. Ankle—radiography. 3. Ankle Injuries—diagnosis. 4. Diagnostic Imaging—methods. 5. Foot—radiography. WE 880
I305 2011]
RC951.R33 2011
617.5’85—dc22
2010019254
Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. Application of the information in a particular situation remains the professional responsibility of the practitioner.
The authors, editors, and publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accordance with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any change in indications and dosage and for added warnings and precautions. This is particularly important when the recommended agent is a new or infrequently employed drug.
Some drugs and medical devices presented in the publication have Food and Drug Administration (FDA) clearance for limited use in restricted research settings. It is the responsibility of the health care provider to ascertain the FDA status of each drug or device planned for use in their clinical practice.
To purchase additional copies of this book, call our customer service department at (800) 638-3030 or fax orders to (301) 223-2320. International customers should call (301) 223-2300.
Visit Lippincott Williams & Wilkins on the Internet: at LWW.com. Lippincott Williams & Wilkins customer service representatives are available from 8:30 am to 6 pm, EST.
1 2 3 4 5 6 7 8 9 10
To my loving wife, Mary, for her continued support and the total joy she brings to our lives
CONTENTS
| Chapter 1 | Anatomy, Normal Variants, and Basic Biomechanics Thomas H. Berquist |
| Chapter 2 | Diagnostic Techniques Thomas H. Berquist |
| Chapter 3 | Soft Tissue Trauma and Overuse Syndromes Thomas H. Berquist |
| Chapter 4 | Fractures/Dislocations Thomas H. Berquist |
| Chapter 5 | Arthritis Thomas H. Berquist and Laura W. Bancroft |
| Chapter 6 | Bone and Soft Tissue Tumors and Tumor-like Conditions Thomas H. Berquist and Mark J. Kransdorf |
| Chapter 7 | Infection Thomas H. Berquist |
| Chapter 8 | Bone and Soft Tissue Ischemia Thomas H. Berquist and Anthony B. Adelson |
| Chapter 9 | Pediatric Foot and Ankle Disorders Thomas H. Berquist, Laura W. Bancroft, and Debbie J. Merinbaum |
| Chapter 10 | Reconstructive Procedures: Preoperative and Postoperative Imaging Thomas H. Berquist and Joseph L. Whalen |
| Chapter 11 | Miscellaneous Conditions Thomas H. Berquist |
| Index |
CONTRIBUTING AUTHORS
Anthony B. Adelson, M.D.
Assistant Professor
Senior Associate Consultant
Vascular/interventional Radiology
Mayo Clinic College of Medicine
Rochester, Minnesota
Consultant in Diagnostic Radiology
Mayo Clinic in Florida
Jacksonville, Florida
Laura Wasylenko Bancroft, M.D.
Professor of Diagnostic Radiology
Adjunct faculty, University of Central Florida
Diagnostic Radiology
Florida Hospital System
Orlando, Florida
Thomas H. Berquist, M.D.
Professor of Diagnostic Radiology
Mayo Clinic College of Medicine
Rochester, Minnesota
Consultant in Diagnostic Radiology
Mayo Clinic in Florida
Jacksonville, Florida
Mark J. Kransdorf, M.D.
Professor of Diagnostic Radiology
Mayo Clinic College of Medicine
Rochester, Minnesota
Consultant in Diagnostic Radiology
Mayo Clinic in Florida
Jacksonville, Florida
Debbie J. Merinbaum, M.D.
Chairperson, Department of Medical Imaging
Division of Pediatric Radiology
Nemours Children’s Clinic
Jacksonville, Florida
Joseph L. Whalen, M.D.
Assistant Professor of Orthopedics
Mayo Clinic College of Medicine
Rochester, Minnesota
Consultant in Diagnostic Radiology
Mayo Clinic in Florida
Jacksonville, Florida
PREFACE
The First Edition of this text was published in 1989 and the Second Edition in 2000. Imaging approaches have changed significantly since the First Edition. Though radiographs or computed radiography images remain as useful screening technique, there has been a significant increase in multimodality imaging approaches to solve diagnostic challenges in the foot and ankle. Specifically, ultrasound, MR imaging, CT, and diagnostic interventional techniques are more commonly employed. In order to more accurately reflect these practice changes we have changed the Third Edition title from Radiology of the Foot and Ankle to Imaging of the Foot and Ankle.
The overall goals of the text have not changed significantly. In order to accomplish these goals we again review the appropriate utilization of imaging techniques for evaluation of foot and ankle disorders. This requires a thorough knowledge of the advantages and limitations of available imaging techniques and interventional procedures. Secondly, the complex anatomy of the foot and ankle must be clearly understood. Finally, close communication between clinicians (internists, podiatrists, orthopedic surgeons, rheumatologists, emergency room physicians) and radiologists is essential to select the most appropriate imaging approach or approaches to answer the clinical question. The combined knowledge of the clinician and radiologist is essential to optimize patient care and provide economically wise clinical and imaging decisions.
As in previous editions, Chapter 1 reviews anatomy, normal variants, and basic biomechanics of the foot and ankle.
Chapter 2 discusses principles and applications of imaging procedures and interventional techniques. This chapter provides basic background information on technical aspects, applications, and limitations of imaging procedures. The discussion is intended to fulfill two purposes. First, to provide sufficient information, primarily for non-imagers, so they can understand the technique and what patients may experience during and imaging examination for a given modality. Secondly, the information presented can be referred to in subsequent chapters to avoid redundancy when techniques are discussed as they apply to specific pathologic conditions.
Chapters 3 through 8 are pathologically oriented. Soft tissue trauma and overuse syndromes, fracture/dislocations, arthritis, bone and soft tissue tumors, infection and ischemic conditions are discussed. These chapters review clinical features and imaging approaches as they apply to these conditions.
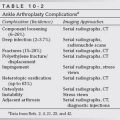
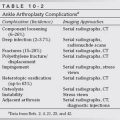
Chapter 9 is devoted to pediatric conditions with an emphasis on congenital foot disorders. Chapter 10 discusses pre- and postoperative imaging of joint replacement and reconstructive procedures in the foot and ankle. Imaging of postoperative complications is emphasized in this chapter. Chapter 11 covers a large variety of miscellaneous conditions such as metabolic disease, Paget disease, and other conditions that are less commonly encountered on foot and ankle images.
This text provides a comprehensive reference for radiologists, radiologists in training, podiatrists, orthopedic surgeons, rheumatologists, emergency room physicians, and other clinicians that deal with foot and ankle disorders. We hope the combined clinical and imaging information presented in this text will serve to emphasize the importance of communication between radiologists and clinicians in dealing with the imaging approaches to foot and ankle disorders.
Thomas H. Berquist
ACKNOWLEDGEMENTS
Preparation of this text was facilitated by the efforts of many individuals in the department of Diagnostic Radiology at Mayo Clinic in Florida. The numerous figures in the Third Edition were selected from case material at Mayo Clinic facilities and Nemours Children’s Clinic in Jacksonville, Florida. I wish to thank Noel Bahr, Dallas Thorpe, Lynn Hill, and Frank St. George for their leadership and assistance as Supervisors of diagnostic imaging, CT, MR imaging, and ultrasound, respectively.
The departments of photographics and medical illustration provided critical support for the images and illustrations. Daniel Hubert assisted in providing timely images and John Hagen provided the superb illustrations necessary to demonstrate the anatomy, specific injuries, and classifications.
The manuscript and orchestration of printed material was performed by my secretary, Suzanne Taylor.
Finally, I wish to thank James Ryan and Brian Brown from Lippincott-Williams and Wilkins for their support during preparation of this text.
CHAPTER 1
Anatomy, Normal Variants, and Basic Biomechanics
Thomas H. Berquist
- Introduction
- Soft Tissue Anatomy
- Posterior Musculature
- Neurovascular Anatomy of the Calf
- Anterolateral Musculature
- Anterior Compartment Musculature
- Neurovascular Anatomy of the Anterolateral Muscles
- Foot Musculature
- Neurovascular Supply of the Foot
- Posterior Musculature
- Skeletal and Articular Anatomy
- Ossicles and Sesamoids of the Foot and Ankle
- Basic Biomechanics
- Plantar Flexion
- Dorsiflexion
- Inversion
- Eversion
- Adduction
- Abduction
- Supination and Pronation
- External Rotation
- Varus
- Valgus
- Plantar Flexion
- Mechanics of the Foot and Ankle Motion
- References
INTRODUCTION
The anatomy of the foot and ankle is complex. There is frequent overlap of osseous structures using conventional radiographs. This factor makes it difficult to evaluate all osseous and articular structures even when multiple projections are obtained. Demonstration of soft tissue anatomy is also critical. Today, computed tomography (CT) with reformatting in the coronal and sagittal planes or three-dimensional reconstruction is frequently used for osseous abnormalities. CT is also useful for certain soft tissue disorders. However, magnetic resonance (MR) imaging offers superior tissue contrast for evaluation of subtle bone and soft tissue changes in multiple image planes. Therefore, a thorough knowledge of skeletal and soft tissue anatomy in multiple image planes is essential [17,29,53,56,83,92]. Normal variants must also be mastered to distinguish normal from pathologic changes in the foot and ankle [4,43,44,50,52,72,87,89]. A basic understanding of biomechanics is also essential for selecting the proper diagnostic techniques [12,13]. Mastering the anatomy and basic functions of the foot and ankle is equally important to physicians involved in imaging procedures, clinical medicine, and surgery.
SOFT TISSUE ANATOMY
The lower extremity musculature develops from mesodermal tissues of the lower limb bud [1]. Functional muscle groups are organized in fascial compartments. Therefore, to simplify the muscular anatomy of the foot and ankle, this discussion focuses on compartments or functional groups of muscles, including their origins, insertions, and actions. Normal variants are also discussed.
The muscles of the leg can be divided into anterior, posterior, and lateral compartments (Fig. 1-1). One of these muscles crosses only the knee, and two cross the knee and ankle. Most arise in the leg and act on both the foot and the ankle (Fig. 1-2) [2,29,83].
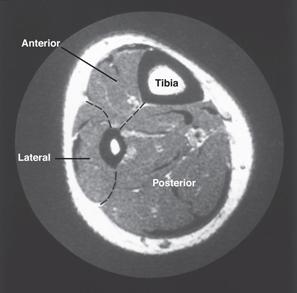
FIGURE 1-1 Axial T1-weighted magnetic resonance image demonstrating the compartments of the leg.
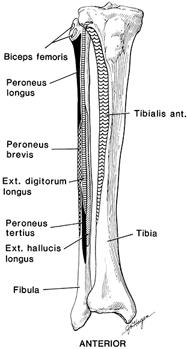
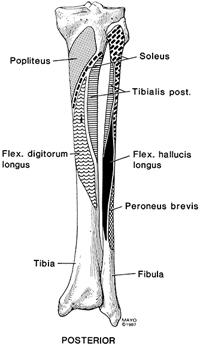
FIGURE 1-2 Anterior (A) and posterior (B) illustrations of the tibia and fibula demonstrating the origins of muscles that insert on or affect the foot and ankle.
Posterior Musculature
The superficial and deep muscles of the calf are divided into compartments by the crural fascia (Fig. 1-3). The superficial muscle group includes the gastrocnemius, soleus, and plantaris (Fig. 1-4). The gastrocnemius has two heads arising from the medial and lateral femoral condyles (Fig. 1-5). The two heads unite to form the bulk of the muscle in the upper calf. At about the midpoint of the calf, the muscle ends in a wide, flat tendon (see Figs. 1-4A and 1-6). The soleus inserts into the anterior aspect of the gastrocnemius tendon (see Figs. 1-4B and 1-6D). Below this level, the tendon narrows in transverse diameter and thickens, forming the Achilles tendon (tendo calcaneus), which inserts on the posterior calcaneus (see Figs. 1-4A and 1-6E). The gastrocnemius plantar flexes the foot and also assists in knee flexion during non–weight bearing. Innervation is by the tibial nerve, and the vascular supply is primarily derived from the posterior tibial artery [29,54,57,83]. Reported variations of the gastrocnemius include absence of the lateral head and central origins from the posterior femur [29,83].
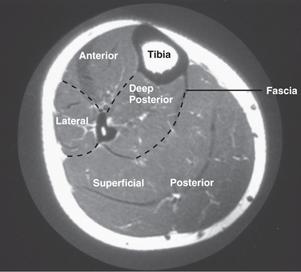
FIGURE 1-3 Axial magnetic resonance image of the calf demonstrating the compartments with crural fascia separating the deep and superficial posterior muscle groups.
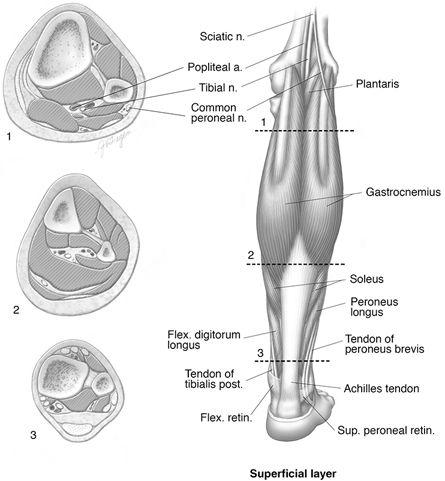
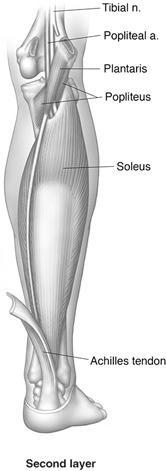
FIGURE 1-4 Muscles of the posterior leg. A) Illustration of superficial musculature with cross sections at levels 1, 2, and 3. B) Illustration of soleus, popliteus, plantaris, and upper vascular relationships.

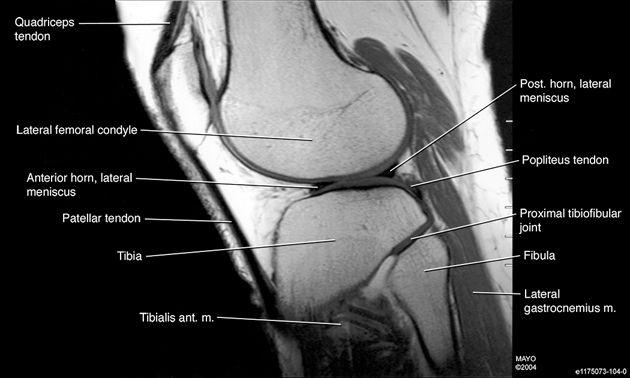
FIGURE 1-5 Coronal (A) and sagittal (B) magnetic resonance images of the knee demonstrating the origins of the gastrocnemius muscles.
The soleus lies deep to the gastrocnemius (see Figs. 1-2, 1-4B, and 1-6C) and also has two heads, one arising from the posterior superior fibula and the second from the popliteal line and posteromedial surface of the proximal tibia (see Fig. 1-2B). The popliteal vessels and tibial nerve pass deep to the body of the soleus (see Fig. 1-4B). The soleus inserts in the anterior aspect of the gastrocnemius tendon, forming the thicker Achilles tendon (see Fig. 1-6D and E) [57,83].
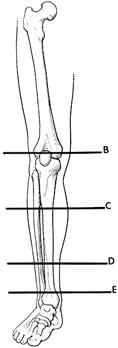
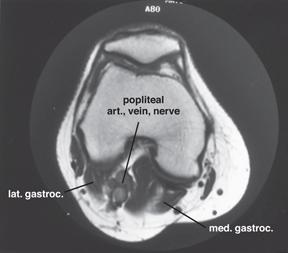

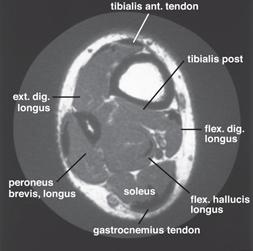

FIGURE 1-6 A) Illustration demonstrating levels of axial magnetic resonance images (MRI). B) Axial MR image at the level of the femoral condyles. C) Axial MR image through the upper calf. D) Axial MR image through the lower leg. E) Axial MR image just above the ankle joint.
The soleus has no effect on the knee, but it serves as a plantar flexor of the foot. Innervation is via the tibial nerve, with vascular supply from the posterior tibial artery [29,57,83].
An important, but uncommon, normal variant is the accessory soleus muscle. Cadaver studies estimate that this muscle is present in up to 6% of the population. The accessory soleus may arise from the anterior soleus muscle or from the fibula and soleal line of the tibia. This accessory muscle bundle extends into Kager fat triangle anterior to the Achilles tendon and inserts in the anterior aspect of this tendon, the posteromedial calcaneus, or the flexor retinaculum [4,6,16,17]. This muscle may be incidentally noted, but some patients may have clinical symptoms. This anomalous muscle may mimic a lipoma, hemangioma, or sarcoma. The most common presenting complaints are soft tissue prominence and pain following exercise. Thus, it is important to differentiate this normal variant from a torn muscle remnant, tendon, or a soft tissue mass [16,17,57,81]. The accessory soleus may be identified on radiographs, but MR imaging is diagnostic (Fig. 1-7). In most cases, no treatment is necessary. However, when symptoms persist, especially with exercise, one should consider exploration with either resection of the accessory soleus or fasciotomy [81].


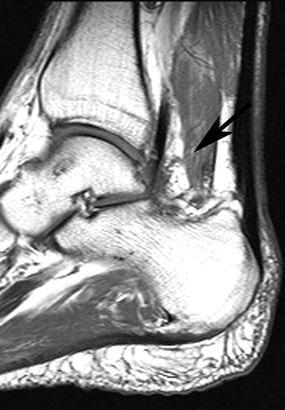
FIGURE 1-7 Lateral radiographs of demonstrating the normal fat density of Kager triangle (arrows) (A) and soft tissue density due to an accessory soleus (arrow) (B). C) Sagittal T1-weighted MR image demonstrating the accessory soleus (arrow).
The plantaris is the third muscle included in the superficial compartment. This small muscle takes its origin from the lateral epicondyle of the femur and the oblique popliteal ligament (see Fig. 1-2). The belly of the muscle is only several inches long and passes between the gastrocnemius and soleus in an oblique direction (see Fig. 1-4A and B). The long, thin tendon passes distally along the medial margin of the Achilles to insert in the calcaneus, Achilles, or flexor retinaculum. Occasionally, the muscle is double, and it may be totally absent [2,29,83].
The plantaris functions as a minor flexor of the knee and a plantar flexor of the foot. Innervation and blood supply are from the tibial nerve and the posterior tibial artery [2,83].
The deep compartment of the calf contains the popliteus, tibialis posterior, flexor hallucis longus, and flexor digitorum longus muscle groups (Fig. 1-8). The popliteus is a small triangular muscle forming a portion of the floor of the popliteal fossa (see Figs. 1-4B and 1-8). Its origin is from the lateral femoral epicondyle, the arcuate popliteal ligament, and the capsule of the knee. The insertion is the posterior surface of the upper tibia above the origin of the soleus (see Figs. 1-2 and 1-8) [2,29,83]. The popliteus acts on the knee and leg as a flexor and a medial rotator. Neurovascular supply is by the tibial nerve and the posterior tibial artery [83].
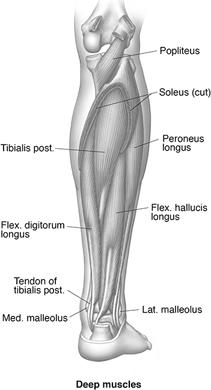
FIGURE 1-8 Illustration of the deep muscles of the posterior leg.
Variations may occur in the origins of the popliteus. In 14% of patients, this muscle arises from the inner aspect of the fibular head and inserts above the oblique tibial line [29,83].
The flexor hallucis longus is the most lateral of the three remaining deep muscles of the leg (flexor hallucis longus, flexor digitorum longus, and tibialis posterior) (see Figs. 1-6C and D and 1-8). It arises from the lateral aspect of the middle half of the posterior fibula (see Fig. 1-2). Its tendon begins above the malleoli of the ankle and courses medially behind the ankle deep to the flexor retinaculum (see Fig. 1-8). The tendon is posterior to the tendons of the tibialis posterior (or posterior tibial tendon) and flexor digitorum longus behind the medial malleolus (Fig. 1-9). The tendon passes along the plantar aspect of the foot to insert in the distal phalanx of the great toe (see Figs. 1-18 and 1-19) [2,15,29,83].
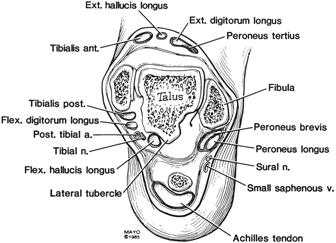
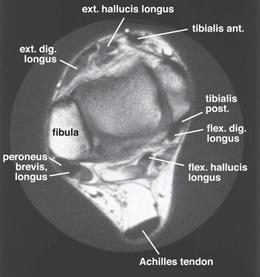
FIGURE 1-9 A) Illustration of tendon and neurovascular relationships about the ankle. (From Berquist TH. MRI of the Musculoskeletal System. 3rd ed. New York: Lippincott–Raven; 1996, with permission.) B) Axial magnetic resonance image with anatomy labeled.
The flexor hallucis longus is a flexor of the great toe and assists in ankle flexion. The muscle is innervated by the tibial nerve and receives its blood supply from the posterior tibial artery [29].
Minor variations in the origin of the flexor digitorum longus are not uncommon. An accessory muscle, peroneocalcaneus internus, occurs in 1% of asymptomatic patients [4,6,58]. Up to 75% of these muscles are bilateral. The muscle arises from the lateral flexor hallucis longus and the posterior fibula. The peroneocalcaneus internus lies posterolateral to the flexor hallucis longus as it courses inferiorly to the sustentaculum tali to insert on the calcaneus. Both tendons may be visible on sagittal and axial MR imaging studies as they pass inferiorly to the sustentaculum tali (Fig. 1-10) [4,58]. The peroneocalcaneus internus muscle does not present as a soft tissue mass or cause neurovascular compression, which can occur with other accessory muscles [6,16,17,58]. However, in some cases, it may displace the flexor hallucis longus muscle and may cause indirect neurovascular compression [58].
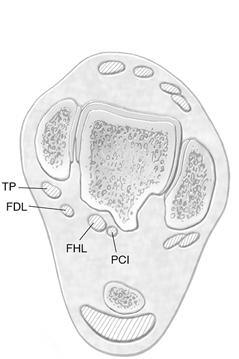
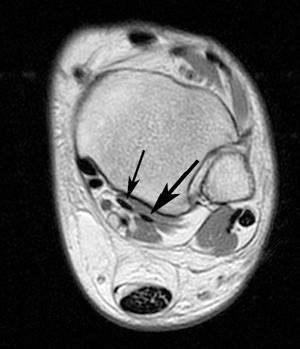
FIGURE 1-10 A) Axial illustration of the ankle demonstrating four medial tendons instead of the usual three tendons: tibialis posterior (TP), flexor digitorum longus (FDL), flexor hallucis longus (FHL), and peroneocalcaneus internus (PCI). B) Axial T1-weighted MR image demonstrating the peroneocalcaneus internus (large arrow) lateral to the flexor hallucis longus (small arrow). (From Bancroft LW, Bridges MD. MRI: Normal Variants and Pitfalls. : Lippincott Williams & Wilkins; 2008, with permission.)
The flexor digitorum longus lies medially in the deep compartment of the calf (see Figs. 1-6D and 1-8). It arises from the upper half of the posteromedial aspect of the tibia (see Fig. 1-2). Along the caudad course, it passes posterior to the tibialis posterior so that, at the ankle, it lies between the flexor hallucis longus and the tibialis posterior (see Fig. 1-9). The tendon passes through the flexor retinaculum, posterior to the medial malleolus, and then divides into four slips, which insert in the distal phalanges of the lateral four digits (see Figs. 1-18 and 1-19). On the plantar aspect of the foot, these four tendon slips are associated with the lumbrical muscles and pass through the divided slips of the flexor digitorum brevis before inserting on the distal phalanges [2,29,83].
The flexor digitorum longus flexes the lateral four toes and also plantar flexes the foot and supinates the ankle. The muscle is innervated by branches of the tibial nerve and receives its vascular supply from posterior tibial artery branches [29,83].
A fairly common accessory flexor muscle can be demonstrated. The flexor accessorius longus digitorum arises from the lower fibula, interosseous membrane, and tibia and passes beneath the flexor retinaculum to insert in the flexor digitorum longus tendon or quadratus plantae tendon [4,29].
The tibialis posterior is the deepest and most centrally located muscle in the deep posterior compartment (see Figs. 1-6C and D and 1-8). It arises from the upper posterior aspects of the tibia and fibula and the interosseous membrane (see Fig. 1-2). Thus, it is positioned between the flexor hallucis longus and the flexor digitorum longus. The tendon passes medially deep to the flexor retinaculum and the flexor digitorum longus (see Fig. 1-6E). Therefore, it is the most anterior of the three tendons as it passes behind the medial malleolus (see Fig. 1-9). The tendon flares (Fig. 1-11) to insert in the navicular, tarsal bones, and bases of the second to fourth metatarsals (see Fig. 1-21) [2,29,83].
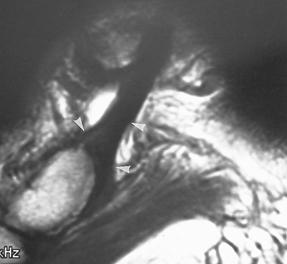
FIGURE 1-11 Sagittal magnetic resonance image demonstrating the normal flare or widening (arrowheads) of the tibialis posterior tendon as it inserts onto the navicular.
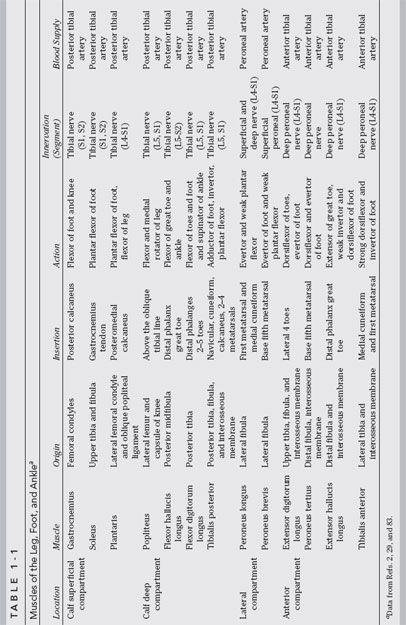
The tibialis posterior aids in adduction, inversion, and plantar flexion of the foot. The muscle is innervated by branches of the tibial nerve and receives its blood supply from the posterior tibial artery [2,29]. Table 1-1 summarizes the muscles of the calf and their functions.
Neurovascular Anatomy of the Calf
The tibial nerve is a continuation of the sciatic nerve at the level of the popliteal fossa. As it passes inferiorly, it enters the calf between the heads of the gastrocnemius muscle, passing deep to the soleus to lie between the soleus and tibialis posterior in the deep compartment (Fig. 1-12) [2,83]. The tibial nerve sends branches to all the superficial and deep muscles of the calf (see Table 1-1 and Figs. 1-8 and 1-12). At the ankle level, the nerve generally lies between the flexor hallucis longus and the flexor digitorum longus tendons (see Figs. 1-9 and 1-12). Distal to the flexor retinaculum, it divides, forming the medial and lateral plantar nerves [2,29,83].
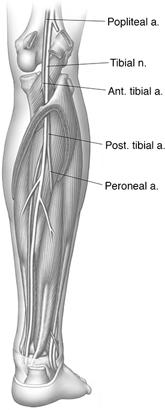
FIGURE 1-12 Illustration of the major neurovascular structures of the posterior compartment.
The popliteal artery is a direct continuation of the superficial femoral artery as it passes through the adductor canal (see Fig. 1-12). It divides into anterior and posterior tibial branches at the level of the popliteus muscle. The anterior tibial artery enters the anterolateral leg above the upper margin of the interosseous membrane, whereas the posterior tibial artery joins the tibial nerve in the deep compartment of the calf (see Figs. 1-12 and 1-16B). In the leg, it provides muscular branches to all the calf muscles and a nutrient artery to the tibia. Its largest branch, the peroneal artery, arises high in the leg and passes deep to the flexor hallucis longus near the interosseous membrane and the fibula (see Figs. 1-12 and 1-16B). At the ankle level, it forms anastomotic branches with the posterior tibial artery and perforates the interosseous membrane to supply the dorsal aspect of the foot. Generally, paired veins accompany the arteries. These veins are more variable and enter the popliteal vein superiorly [2,29,83].
Anterolateral Musculature
The peroneus longus and brevis are the two muscles of the lateral compartment. Both arise from the superior lateral surface of the fibula. The origin of the peroneus longus is more superior, with the muscle passing superficial to the peroneus brevis (see Fig. 1-2). The muscles progress caudad in the lateral compartment (see Figs. 1-1, 1-6, and 1-9), with their tendons entering a common tendon sheath above the ankle (see Figs. 1-9 and 1-13). The tendons pass posterior to the lateral malleolus and deep to the superior and inferior peroneal retinacula (Fig. 1-14). The tendons diverge on the lateral surface of the foot with the peroneus brevis inserting on the base of the fifth metatarsal. The peroneus longus takes an inferior course, passing under the lateral aspect of the foot, where it inserts on the base of the first metatarsal and the medial cuneiform (see Fig. 1-21) [2,20,29,86,105].
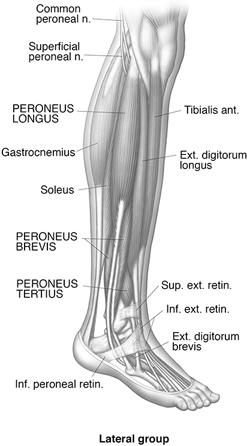
FIGURE 1-13 Illustration of the lateral muscles of the leg and their tendinous relationships at the ankle.

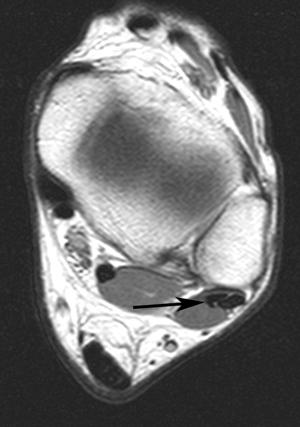
FIGURE 1-14 Sagittal fat-suppressed T2-weighted (A) and axial T1-weighted MR images demonstrating the normal low signal intensity and position of the peroneus brevis and longus as they pass below the lateral malleolus (A) and at the level of the ankle (B).
These muscles serve as evertors of the foot and assist in plantar flexion. Innervation is from the superficial peroneal nerve with branches of the common or deep peroneal nerve supplying a portion of the peroneus longus. Vascular supply is via the peroneal artery [2,29].
Multiple peroneal variations may cause confusion on MR imaging or CT images. The muscles (longus and brevis) may fuse to form one unit, and occasionally the peroneus longus insertion expands to include the bases of the third to the fifth metatarsals. An accessory peroneal muscle may arise from the fibula between the peroneus longus and brevis. Its tendon generally inserts in the peroneus longus tendon on the plantar aspect of the foot [83,86,105].
The peroneus quadratus is present in about 10% to 17% of patients [4,6,11,17,86,105]. This anomalous muscle is three times as common in males compared with females [11]. Three variations of the peroneus quadratus have been described, based on their insertions. One of this subgroup inserts on the calcaneus (peroneocalcaneus externum), one on the cuboid (peroneocuboideus), and the third variation inserts on the peroneal tendon (long peroneal) [32]. The peroneus quadratus has been associated with clinical symptoms (pain and instability), and it is associated with peroneal tendon subluxation, which is discussed in detail in Chapter 3 [11]. On MR images (Fig. 1-15), the peroneus quadratus tendon is posterior to the brevis and longus tendons [4,11].
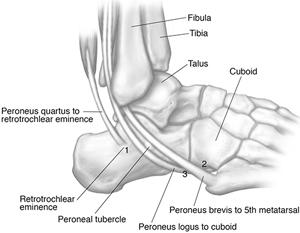
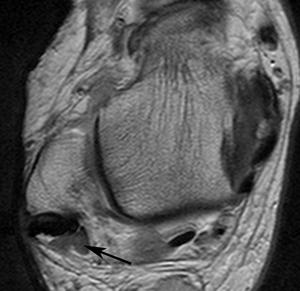
FIGURE 1-15 A) Illustration of the peroneus quadratus, which may insert on the retrotrochlear eminence (1), cuboid (2), or longus tendon (3). B) Axial magnetic resonance image demonstrating peroneus quadratus muscle (arrow) posterior and medial to the peroneus brevis and longus.
The peroneus digiti minimi is rare. It arises from the lower fibula and inserts on the extensor surface of the fifth toe [11,83].
Anterior Compartment Musculature
The anterior compartment has four muscles. These include the extensor digitorum longus, the peroneus tertius, the extensor hallucis longus, and the tibialis anterior (Fig. 1-16).
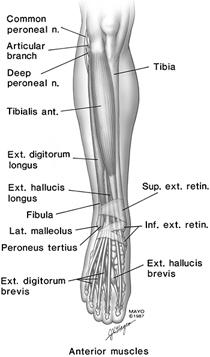
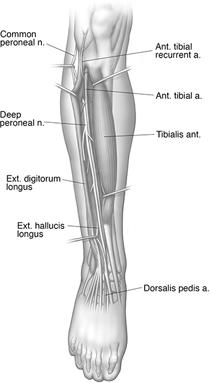
FIGURE 1-16 Illustrations of the anterior muscles (A) and neurovascular anatomy (B) in the anterior leg.
The extensor digitorum longus is the most lateral muscle in the anterior compartment (see Fig. 1-16) [2,29]. It arises from the lateral tibial condyle, the anterior fibula, and the interosseous membrane (see Fig. 1-2). The tendon passes deep to the superior and inferior extensor retinacula (see Fig. 1-9) before dividing into four slips that insert on the dorsal aspects of the four lateral toes (see Fig. 1-16A). The insertions are divided such that portions insert in the middle and distal phalanges [2,29].
This muscle dorsiflexes the toes and also assists in eversion of the foot. It is innervated by the deep peroneal nerve and receives its vascular supply from the anterior tibial artery (see Fig. 1-16B). Variations in its origin and distal insertions are not uncommon, but these rarely cause confusion on CT or MR imaging [4].
The peroneus tertius is closely associated with the extensor digitorum longus, and it may be considered a portion of the latter [2,83]. It arises from the distal anterior fibula, the interosseous membrane, and the membrane of the peroneus brevis (see Fig. 1-2). Its tendon passes deep to the extensor retinacula to insert on the dorsal aspect of the base of the fifth metatarsal (see Fig. 1-16A). It is supplied by the deep peroneal nerve and the anterior tibial artery. This muscle varies in size and may be absent [2,29,83].
The extensor hallucis longus lies deep to the extensor digitorum longus and the tibialis anterior. It arises from the midfibula and the interosseous membrane and becomes superficial in the lower leg (see Fig. l-2). Its tendon passes deep to the extensor retinacula to insert on the distal phalanx of the great toe (see Figs. 1-9 and 1-16A). This muscle extends the great toe and is a weak dorsiflexor and invertor of the foot. It is supplied by the deep peroneal nerve and the anterior tibial artery [2,15,29].
Occasionally an accessory muscle, the extensor ossis metatarsi hallucis, arises from the extensor digitorum longus, the tibialis interior, or the extensor hallucis longus. Unlike the accessory soleus, this muscle is generally too small to be confused with a soft tissue mass [17,29]. An additional accessory tendon, the extensor hallucis capsularis is present in 88% of the population. This tendon lies medial to the extensor hallucis longus and in 14% of patients is suitable for orthopaedic reconstructive procedures. Therefore, it is important to recognize this variant on MR images in patients considered candidates for foot reconstructive surgery [9].
The tibialis anterior arises from the lateral tibia surface, the deep fascia, and the interosseous membrane (see Fig. 1-2). It passes inferiorly, becoming tendinous in the lower leg (see Figs. 1-6, 1-9, and 1-16A). It is the most medial tendon as it passes deep to the extensor retinacula. It passes along the medial foot to insert in the medial cuneiform and plantar portion of the first metatarsal (see Fig. 1-16A) [29,83].
This muscle is a strong dorsiflexor and inverter of the foot. Neurovascular supply is via the deep peroneal nerve and the anterior tibial artery [2,29,83].
Neurovascular Anatomy of the Anterolateral Muscles
The common peroneal nerve is a branch of the sciatic nerve and courses laterally in the popliteal fossa. It is subcutaneous and is relatively unprotected just below the fibular head (see Fig. 1-16B). Therefore, it is susceptible to direct trauma in this area [8,29]. As it descends between the fibula and the peroneus longus, it divides into two or three branches. These are the superficial, deep, and articular branches of the peroneal nerve (see Fig. 1-16B). The superficial peroneal nerve lies between the peroneus longus and brevis and supplies these muscles and the subcutaneous tissues. The deep peroneal nerve courses anteriorly, deep to the peroneus longus, to supply the anterior muscles of the leg (see Table 1-1 and Fig. 1-16B). It joins the anterior tibial artery on the anterior aspect of the interosseous membrane [2,29,83].
The anterior tibial artery passes superior to the interosseous membrane in the upper leg and then lies with the deep peroneal nerve along the anterior aspect of the interosseous membrane (see Figs. 1-12 and 1-16B). It supplies the anterior muscles and continues as the dorsalis pedis artery on the dorsum of the foot [2,29,83]. Table 1-1 summarizes the muscles of the leg, their functions, and neurovascular supply.
Foot Musculature
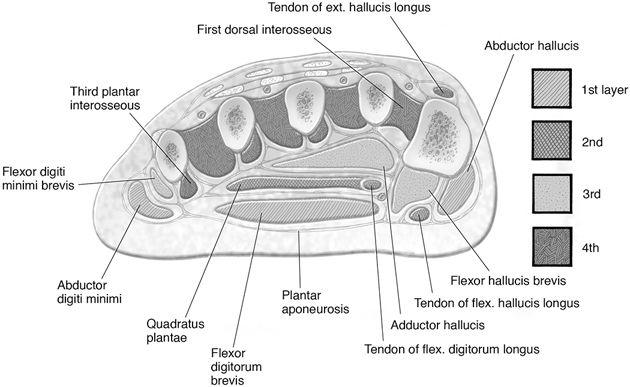
The muscles of the foot are discussed by layer, rather than by compartments as in the leg, to facilitate anatomic discussion (Fig. 1-17) [26,29]. The compartment concept is included later in this section. The superficial layer of plantar muscles includes the abductor hallucis, the flexor digitorum brevis, and the abductor digiti minimi [26,83].