The Cortical Branches of the Middle Cerebral Artery
16.1 Case Description
16.1.1 Clinical Presentation
A 30-year-old woman was investigated with magnetic resonance (MR) in screening for familial aneurysms, and an incidental left-sided broad-based 8-mm middle cerebral artery (MCA) aneurysm was found. The patient was referred to neurosurgery.
16.1.2 Radiologic Studies
See ▶ Fig. 16.1, ▶ Fig. 16.2, and ▶ Fig. 16.3.
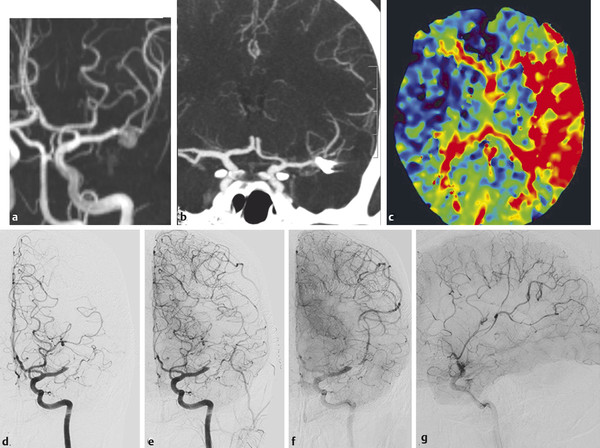
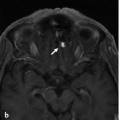
Fig. 16.1 Immediately after clipping of an incidental left-sided MCA aneurysm (MR angiography in a), this 30-year-old patient presented with a complete right-sided hemiparesis and aphasia. CTA (b) failed to demonstrate a normal MCA bifurcation, whereas CT perfusion (Time to Peak [TTP] Map in c) showed significant hypoperfusion of her left hemisphere. The patient was immediately reoperated, and the clip was repositioned. On surgical inspection, however, the operator noted that thrombus was present within the MCA bifurcation, and emergency thrombectomy was requested. Injection into the left internal carotid artery (ICA) in early (d) and late (e) arterial and capillary (f,g) phases revealed occlusion of the distal M1 with good filling of the lenticulostriate arteries and excellent collaterals from the ACA territory reconstituting the dominant superior division of the MCA. Case continued in ▶ Fig. 16.1.
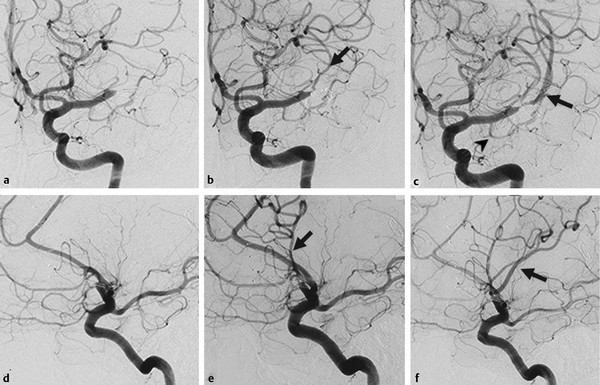
Fig. 16.2 (a,d) Initial angiographic runs; (b,e) runs after the first pass; (c,f) runs after the second pass. After the first pass, the prefrontal or opercular branch was opened (arrow in b,e), which supplies the Broca territory. With the second pass, the dominant superior division, including the Rolandic artery, was opened (arrow in c,f). Note the early anterior temporal branch of the MCA trunk (arrowhead in c). Case continued in ▶ Fig. 16.3.
Fig. 16.3 Axial diffusion-weighted imaging at various levels (a–d) 24 hours after the intervention did not show any areas of ischemia, and the patient had no neurological deficit.
16.1.3 Diagnosis
Acute MCA occlusion with subsequent thrombectomy
16.2 Embryology and Anatomy
Distal to the MCA trunk, the MCA typically splits into two divisions—the superior and the inferior trunk—which are in hemodynamic balance and show considerable variations regarding dominance of one trunk over the other (with concomitant annexed territories). The superior division will supply the frontal convexity, whereas the inferior trunk will supply the temporal lobe. The parietal lobe can be supplied by either trunk (typically the one that is dominant) or by its own division of the MCA; in these cases, a MCA trifurcation is present. An anterior temporal branch can arise proximally from the MCA trunk. Over the frontal and parietal convexity, the distal MCA branches are in hemodynamic balance with the ACA branches (the ACA–MCA watershed), whereas over the temporal lobe, the MCA is in balance with the PCA (see also Case ▶ 17). In addition to their cortical supply, the distal MCA branches also give rise to leptomeningeal perforating arteries that will supply the peripheral white matter and will constitute the hemodynamic watershed with the lenticulostriate arteries of the MCA trunk. The M3 and M4 branches show a certain degree of variability, which is why the nomenclature of these branches varies. In most practices, vessels are named, irrespective of their origin, on the basis of the cortical territory they supply, which will lead to the following MCA “branches”: orbitofrontal, prefrontal, pre-Rolandic, Rolandic, parietal, angular, temporooccipital, posterior temporal, and middle and anterior temporal. These branches are best appreciated on the lateral view (▶ Fig. 16.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree