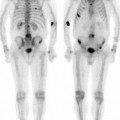
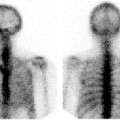
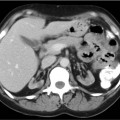
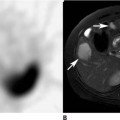
CASE 165 A 10-year-old boy presents with a 6-week history of right leg pain after falling while playing football. Radiographs are suggestive of osteosarcoma. Fig. 165.1 • 99mTc-MDP at 0.2 mCi/kg of body weight is given intravenously. The minimum dose is 1 mCi; the maximum dose is 20 mCi. • Use a high- or ultra-high-resolution, low-energy, parallel-hole collimator. Supplemental pinhole magnification images are obtained in addition to the planar images for improved detail. SPECT is performed for better three-dimensional localization. • The imaging time for an initial radionuclide angiogram is 3-second frames for 1 minute. A static blood pool image should be obtained within 5 to 10 minutes following tracer injection. Whole-body or spot views of the entire bony skeleton should be obtained 4 hours after tracer injection. Spot planar or SPECT views of the region-of-interest should be obtained as needed. Whole-body 99mTc-MDP images (Fig. 165.1) demonstrate a focal area of intense increased uptake in the distal diaphyseal region of the right femur. This corresponds to the area of abnormality seen on radiography. No metastatic disease is visualized. Retained tracer is present in the intravenous line of the left hand and wrist. (Solitary site of focal bony tracer uptake) • Benign primary tumor • Trauma • Primary bone malignancy • Bony metastasis • Osteomyelitis • Bony infarct • Skin contamination overlying bone structure Biopsy of the primary site proved it to be osteosarcoma. The initial metastatic workup was negative. Chemotherapy was initiated, and wide tumor excision with allograft reconstruction was performed. Follow-up skeletal scintigraphy and CT of the chest were obtained at regular intervals for metastatic evaluation. In the fourth year of clinical follow-up, skeletal scintigraphy demonstrated widespread skeletal metastatic disease with soft tissue localization of tracer in pulmonary metastases that was confirmed by CT (Fig. 165.2).
Clinical Presentation
Technique
Image Interpretation
Differential Diagnosis
 Accidental
Accidental
 Post-surgical
Post-surgical
Diagnosis and Clinical Follow-Up
Discussion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree