The Leptomeningeal Anastomoses
17.1 Case Description
17.1.1 Clinical Presentation
A 30-year-old man with history of prosthetic mitral valve replacement associated with rheumatic disease was poorly compliant with his anticoagulation therapy regimen. He presented to the emergency department with aphasia and left-sided hemiplegia, with the arm more pronounced then the leg. Because he had an absolute contraindication to the use of intravenous recombinant tissue plasminogen activator, he was brought to the angio-suite for mechanical thrombectomy.
17.1.2 Radiologic Studies
See ▶ Fig. 17.1, ▶ Fig. 17.2.
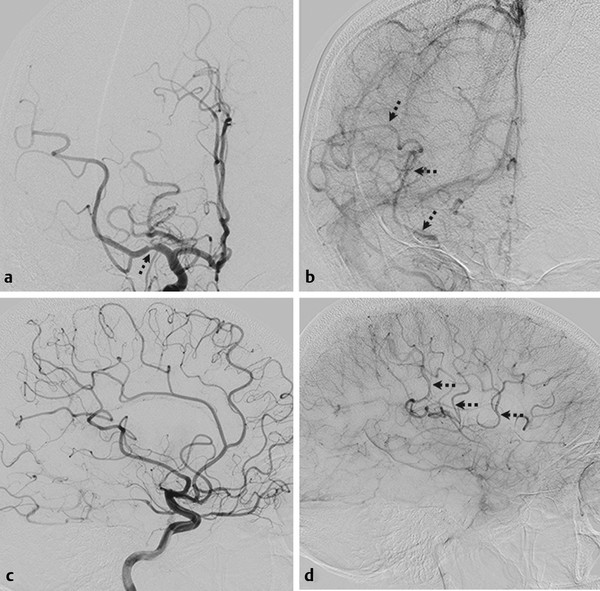
Fig. 17.1 Right internal carotid artery (ICA) angiogram in anteroposterior (AP) (a,b) and lateral (c,d) views in arterial (a,c) and late capillary (b,d) phase. There is occlusion of the superior division of the middle cerebral artery (MCA), with a focal extrinsic filling defect in the M1 trunk (arrow). The late-capillary-phase angiograms show retrograde filling of the superior division of the MCA via LMAs from the ACA (thin arrows in b,d). Case continued in ▶ Fig. 17.2.
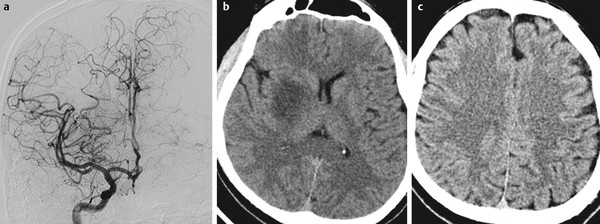
Fig. 17.2 Right ICA angiogram in AP view after thrombectomy (a) demonstrates complete recanalization of the superior division of the MCA with good antegrade flow and no distal filling defects. Control unenhanced axial computed tomography 24 hours after thrombectomy (b,c) shows an infarct in the right striatum but no cortical infarct in the territory of the superior division of the MCA, as the cortex received collateral supply during MCA trunk occlusion, whereas the perforators did not.
17.1.3 Diagnosis
Acute stroke resulting from embolic occlusion of the superior division of the middle cerebral artery (MCA) with excellent leptomeningeal collateral circulation.
17.2 Anatomy
Leptomeningeal anastomoses (LMAs), or leptomeningeal collaterals, are small arteriolar connections (~50–400 µm) between two cerebral arteries supplying two different but adjacent cortical territories. They were initially described by Sir Thomas Willis in 1684, but the first well-documented work demonstrating their presence was done by Heubner in 1874. These vessels form an extensive network that provides a potential route for collateral perfusion, together with the large arterial communications and the circle of Willis.
In LMAs, blood can flow in both directions, depending on the hemodynamic and metabolic needs, thus allowing retrograde perfusion of adjacent territories. Their presence, number, size, and location have a high degree of variability between individuals as well as between hemispheres in the same person. They tend to be more extensive along the convexity, connecting the MCA with the anterior cerebral artery (ACA) and posterior cerebral artery (PCA) territories, but there are also LMAs connecting the ACA and PCA territories (precuneus and splenium of the corpus callosum), as well as both ACA territories (through callosal arteries) and between distal branches of the MCA, PCA, and ACA (▶ Table 17.1).
Territory | Anastomosing Arteries | Location of the Anastomosis |
MCA and ACA | Orbito-frontal (MCA) with fronto-orbital and fronto-polar (ACA) | Inferior and middle frontal gyrus |
Pre-frontal artery (MCA) with anterior/middle internal frontal artery (ACA) | Superior frontal sulcus | |
Pre-central artery (MCA) with posterior internal frontal artery (ACA) | Pre-central sulcus | |
Central artery (MCA) with paracentral artery (ACA) | Central sulcus | |
Parietal artery (MCA) with superior parietal (ACA) | Post-central sulcus or intraparietal sulcus | |
MCA and PCA | Angular or posterior temporal artery (MCA) with parieto-occipital artery (PCA) | Parieto-occipital or intraparietal sulcus |
Temporal arteries (MCA) with inferior temporal trunk branches (PCA) | Middle temporal sulcus | |
ACA and PCA | Superior parietal or pericallosal arteries (ACA) with parieto-occipital artery (PCA) | Parieto-occipital sulcus |