19 Vascular Abnormalities of the Head and Neck
19.1 Introduction
Multiple vascular malformations and vascular neoplasms of the neck are relatively unique to the pediatric population and merit clinical familiarity. The terminology used to describe these vascular malformations and neoplasms can initially be confusing, but they differ in age of onset, features on imaging, and treatment, and the correct terminology for describing them is therefore important. Additionally, traumatic and infectious complications can affect the major arterial and venous structures of the neck and must be recognized and characterized.
19.2 Anatomy
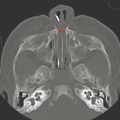
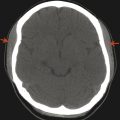
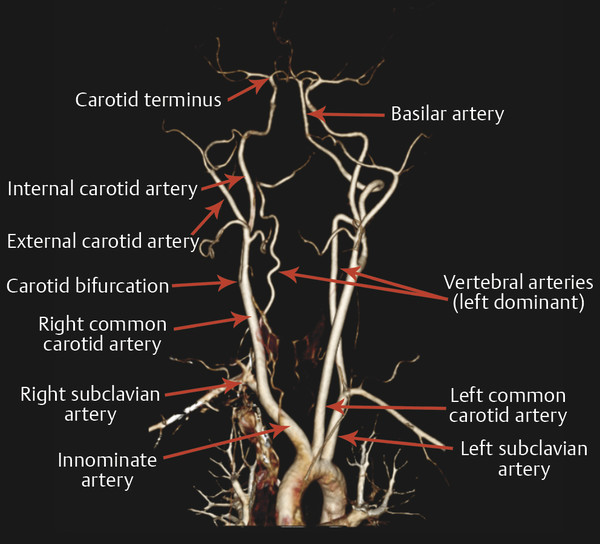
The major arterial structures of the neck are the bilateral carotid and vertebral arteries (Fig. 19.1). The common carotid arteries branch in the midneck to give rise to the internal and external carotid arteries. The internal carotid arteries predominantly supply the intracranial contents, while the external carotid arteries supply the face and neck. The vertebral arteries predominantly supply the posterior cranial fossa, including the brainstem and cerebellum, as well as the thalami and occipital lobes, and contribute to the blood supply of the cervical spinal cord.
19.3 Hemangiomas of Infancy
Vascular malformations of the head and neck are commonly encountered in children, including malformations identified after symptomatic presentation and those found incidentally in the course of examinations for other reasons. These lesions may present as swellings or through mass effect on another structure, sometimes with skin discoloration. A majority, however, are small capillary hemangiomas identified on clinical examination and do not require imaging evaluation.
Rather than being classified as a vascular malformation, the lesions known as capillary hemangiomas are in actuality vascular neoplasms. They differ from “cavernous hemangiomas,” which can, for example, be seen in the adult orbit and are venous malformations rather than vascular neoplasms (and are therefore not hemangiomas, and accordingly the term “cavernous hemangioma” should be avoided), and the prefix “capillary” should be used to describe these lesions to differentiate them from other entities described as hemangiomas.
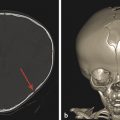
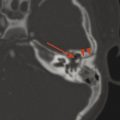
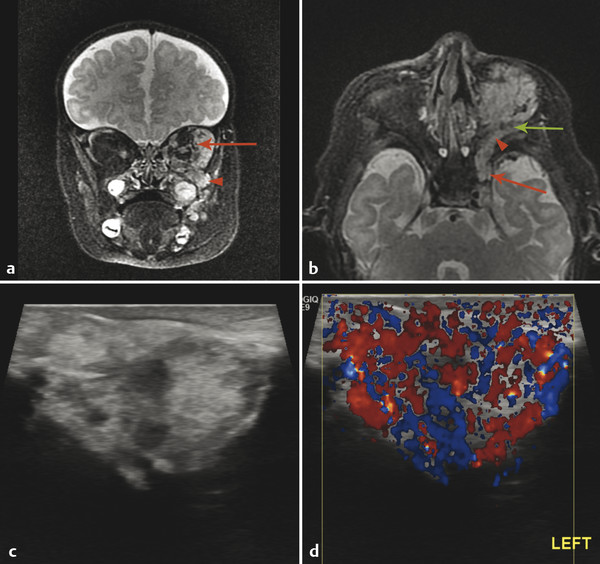
Capillary hemangiomas have several patterns of presentation. An infantile hemangioma, sometimes called a “strawberry mark,” is a capillary hemangioma that is not present at birth, but grows during the first 6 to 12 months of life (proliferative phase), after which it shows a variable period of stability (plateau phase), and eventually involutes (involution phase). Capillary hemangiomas have a characteristic hyperintense appearance on T2 W images, may have internal flow voids, and demonstrate diffuse enhancement (Fig. 19.2). On dynamic imaging the enhancement tends to be in the arterial phase of blood flow through the lesion. The lesions show diffuse vascularity on Doppler ultrasonography.
Although capillary hemangiomas eventually involute spontaneously, the process of involution can be accelerated by beta blocker (propranolol) therapy. The decision to use propranolol is based on several possible indications. One such indication may be large size and/or rapid growth of a hemangioma, and/or mass effect on important structures, such as the airway or major vascular structures. Even small lesions that impair eye movement or eyelid opening may be treated to prevent amblyopia. In some instances, the decision to treat a hemangioma is based on cosmetic rather than clinical concerns.
Magnetic resonance imaging (MRI) and ultrasonography serve a complementary role in evaluating capillary hemangiomas. Computed tomography is typically not needed, given that the information required for identifying and treating these lesions can be obtained by other means, without the use of ionizing radiation.
In addition to infantile hemangiomas, the category of vascular lesions known as capillary hemangiomas includes the lesions known as congenital hemangiomas. In contrast to infantile hemangiomas, congenital hemangiomas are present at birth. Congenital hemangiomas fall into two categories; those that spontaneously involute, and those that do not. These are respectively named rapidly involuting congenital hemangiomas (RICH) and noninvoluting congenital hemangiomas (NICH). However, it may not be possible, without follow-up, to know whether a particular hemangioma belongs in the first or second of these two categories.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree